Primary Retroperitoneal Mucinous Tumor with Borderline Malignancy
by Carla Mayer1, Roman Rechner2*, Thomas Herrmann1,3,4, Achim Fleischmann5, Lukas Boesch5, Jan Klein2,6
1Department of Urology, Spital Thurgau AG, Kantonsspital Münsterlingen, Pfaffenholzstrasse 4, CH 8501, Frauenfeld, Switzerland
2Department of Urology, Spital Thurgau AG, Kantonsspital Münsterlingen, Spitalcampus 1, CH 8596, Münsterlingen, Switzerland
3Division of Urology, Department of Surgical Sciences, Stellenbosch University, Western Cape, South Africa
4Hannover Medical School, Hannover, Germany
5Department of Pathology, Spital Thurgau AG, Kantonsspital Münsterlingen, Spitalcampus 1, CH 8596, Münsterlingen, Switzerland
6University Hospital Ulm, Medical School, Department of Urology and Pediatric Urology, Ulm, Germany
*Corresponding author: Roman Rechner, Department of Urology, Spital Thurgau AG, Kantonsspital Münsterlingen, Spitalcampus 1, CH 8596, Münsterlingen, Switzerland
Received Date: 04 April 2025
Accepted Date: 10 April 2025
Published Date: 12 April 2025
Citation: Mayer C, Rechner R, Herrmann T, Fleischmann A, Boesch L, et al. (2025) Primary Retroperitoneal Mucinous Tumor with Borderline Malignancy. J Surg 10: 11301 https://doi.org/10.29011/2575-9760.011301
Abstract
Background: Primary Retroperitoneal Mucinous Tumors (PRMTs) are extremely rare neoplasms, with only a limited number of cases reported in the literature. They are classified into mucinous cystadenomas, mucinous borderline tumors, and mucinous cystadenocarcinomas.
Case Presentation: We report the case of a 78-year-old female who presented with fatigue, knee pain, and tingling sensations. MRI of the lumbar spine incidentally revealed Grade IV hydronephrosis on the right side. A subsequent CT scan suggested a large renal cell carcinoma, leading to an open radical nephrectomy through a transperitoneal approach. Histopathological examination identified a primary retroperitoneal tumor with borderline malignancy adherent to the kidney. The patient’s postoperative course was initially uneventful; however, she developed paralytic ileus requiring conservative management. Additionally, a persistent pulmonary lesion prompted a segmentectomy, confirming an in-situ adenocarcinoma of the lung.
Discussion: To our knowledge, including this case, only 35 case reports of primaryretroperitoneal mucinous borderline tumors have been published. PRMTs with borderline malignancy are predominantly found in women, with a median age of 42.4 years. Their clinical presentation varies. Imaging studies lack specific diagnostic criteria, and tumor markers are inconsistently elevated. Complete surgical resection remains the primary treatment, yielding an excellent prognosis. Due to the absence of standardized follow-up guidelines, individualized surveillance strategies are recommended.
Conclusion: Primary retroperitoneal mucinous tumors are a rare but a potential differential diagnosis for retroperitoneal masses. Given their excellent prognosis early recognition and complete resection are crucial. Further case studies are necessary to establish standardized management and follow-up protocols.
Introduction
Primary retroperitoneal tumors are rare neoplasms, accounting for only 0.01-0.2% of all neoplasms [1]. An exceedingly rare subtype within this category is Primary Retroperitoneal Mucinous Tumors (PRMTs), which are further classified into mucinous cystadenomas, mucinous borderline tumors, and mucinous cystadenocarcinomas [2]. To date, only 34 cases of mucinous cystadenomas with borderline malignancy have been documented in the literature [3,4]. Here, we present the case of a 78-year-old female patient who was referred for MRI of the lumbar spine due to fatigue, knee pain, and tingling sensations. Upon detection of a newly developed Grade IV hydronephrosis on the right side and the sonographic confirmation of a mass, a CT scan of the abdomen was performed, raising suspicion of a large renal cell carcinoma. The patient subsequently underwent open nephrectomy on the right side through a transperitoneal approach. Pathological analysis identified a retroperitoneal mucinous borderline tumor adherent to the kidney.
Case Presentation
A 78-year-old Caucasian woman presented to her general practitioner with symptoms of weight loss, severe fatigue, knee pain, and tingling sensations. Her medical history included hypercholesterolemia, asthma, and osteopenia, all managed pharmacologically. The general practitioner ordered an MRI of the lumbar spine, which revealed a previously undiagnosed Grade IV hydronephrosis on the right side. Laboratory results showed mildly impaired renal function. Sonography confirmed the hydronephrosis and additionally revealed a large mass not delimitable from to the kidney. Subsequent CT imaging of the abdomen suggested a high likelihood of right-sided renal cell carcinoma (Figure 1(A-D)). The mass measured approximately 9 x 7.7 x 8.8 cm, appeared heterogeneous with arterial contrast enhancement, and contained calcifications, causing Grade IV hydronephrosis due to compression of the renal collecting system. No intraabdominal metastases were detected.
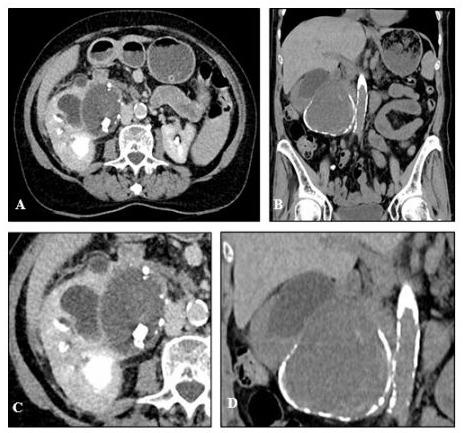
Figure 1: Contrast-Enhanced Computed Tomography (CT) of the Abdomen: In the axial (A and C) and coronal plane (B and D), a peripherally calcified, inhomogeneous mass measuring approximately 9 x 7.7 x 8.8 cm was observed, originating from the pars intermedia of the right kidney. The mass exhibited arterial contrast enhancement. Calcifications up to 2 cm thick were detected in the upper part of the lesion. Due to external compression of the renal pelvis and calyceal system, the mass caused grade 3 hydronephrosis on the right side.
A CT scan of the chest also revealed a poorly defined 10 x 8 x 4 mm consolidation in the right lower lobe, suggestive of either adenocarcinoma of the lung or an inflammatory lesion, though not considered likely metastatic (Figure 2A,B).
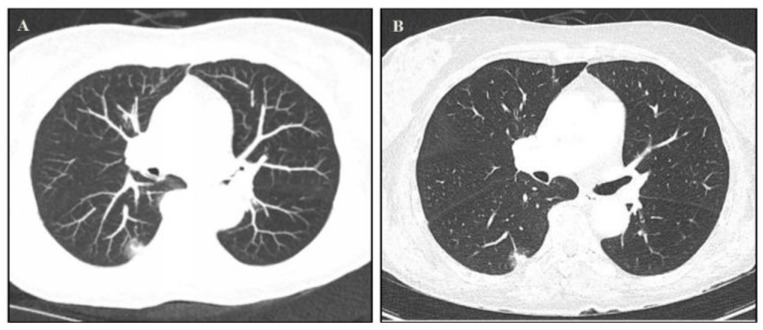
Figure 2(A,B): Contrast-Enhanced Computed Tomography (CT) of the Thorax: Indistinctly marginated consolidation in the right lower lobe with broad-based pleural contact and surrounding ground-glass opacity (10 x 8 x 4 mm). Differential diagnoses included neoplasia, such as bronchial adenocarcinoma, and inflammatory etiology. Hypervascularized metastases from renal cell carcinoma could also present with this morphology.
The patient was referred to the urology department, where interdisciplinary tumor board recommended tumor resection by open radical nephrectomy. A follow-up CT for the pulmonary lesion was advised in three months. Intraoperative findings included a large tumor mass in the area of the caudal part of the kidney with pronounced adhesions between the tumor and the omentum, liver, duodenum, and vena cava, necessitating extensive adhesiolysis. Otherwise, the operation proceeded without complications, and the kidney and tumor were removed in its entirety (Figure 3A,B).
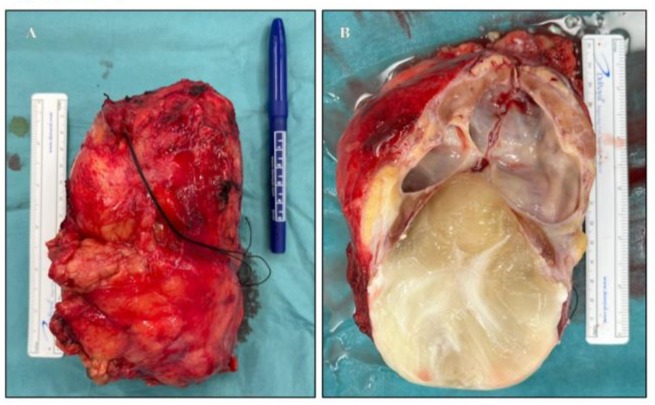
Figure 3(A,B): Intraoperative specimen of the excised kidney measuring 13.7 × 10.5 × 6.5 cm. A completely encapsulated mass measuring 10.3 × 9.5 × 8.5 cm. The cut surface revealed a unilocular cyst with mucinous content. The renal pelvicalyceal system was dilated. Calcifications were identifiable in the capsular region.
The inital postoperative course was otherwise uncomplicated, and the patient was discharged on time for rehabilitation. The patient later developed recurrent nausea and vomiting and was readmitted with paralytic ileus and electrolyte imbalance, which resolved after six days of conservative therapy, allowing discharge in good condition. Histopathological examination revealed a retroperitoneal mucinous borderline tumor (diameter 10.3 cm) located perirenally in the pelvic fat tissue, compressing the renal pelvis and calyces, resulting in chronic active, localized, abscess-forming, destructive pyelonephritis. The epithelial cells express CK7, CK20, and CDX2, without any invasive growth into the capsule (Figures 4,5).
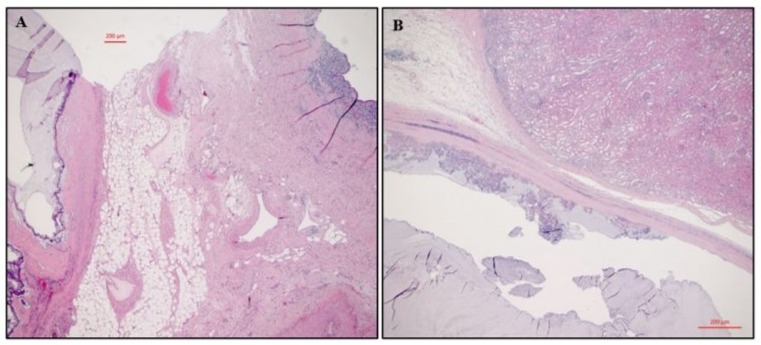
Figure 4: A: Hematoxylin and Eosin Stain (HE) stain shows the renal pelvis (right) and adherent to the pelvic fat a cystic mucinous tumor (left) with focally enlarged and pseudostratified nuclei; B: HE stain with the kidney (upper part) and adherent to its capsule an encapsulated cystic mucinous tumor (lower part) with a papillary, atypical epithelium having enlarged and pseudostratified nuclei.
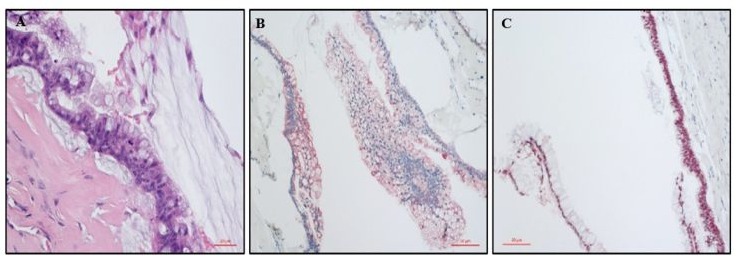
Figure 5: A: Higher magnification demonstrates the atypical mucinous epithelium with enlarged, pseudostratified nuclei and a mitotic figure in the center indicating proliferation (HE); B: Cytokeratin 20 stain shows cytoplasmic positivity in the mucinous epithelium, compatible with intestinal differentiation (immunohistochemistry); C: CDX2 stains the nuclei and indicates intestinal differentiation of the mucinous cells (immunohistochemistry). Of note is the typical spectrum of the nuclei in borderline tumors, ranging from small basally in the cell located nuclei (left) to moderately atypical, enlarged and pseudostratified nuclei (right).
Follow-up CT of the chest showed persistence of the previously described lesion, prompting a lung segmentectomy based on tumor board recommendations. Pathology confirmed in-situ adenocarcinoma of the lung (pTis, pN0 (0/27), R0).
Discussion
Primary retroperitoneal mucinous tumors with borderline malignancy are exceedingly rare malignancies. To our knowledge, including this case, only 35 case reports have been published [3,4]. Of all reported cases, 29 involved female and 6 involved male patients (82.9% to 17.1%). The median age for female patients is 42.4 years, making PRMTs a potential differential diagnosis for young women with retroperitoneal masses. These tumors are often located laterally [5]. The exact pathogenesis and genetic factors remain unclear due to the rarity of these cases [1]. Clinical presentation varies; some patients are asymptomatic, with incidental imaging findings leading to diagnosis, while others present with abdominal or pelvic pain, fatigue, and, in cases of large tumors, palpable masses. Symptoms may include digestive disturbances, flank pain, and urinary obstruction caused by compression of other organs [3]. Preoperative diagnosis is challenging due to the rarity and lack of established radiological criteria. Relevant differential diagnoses include ovarian carcinoma, gastrointestinal tumors, renal cell carcinoma, and metastases [6]. In some cases, elevations of tumor markers, such as carcinoembryonic antigen, cancer antigen 125, and carbohydrate antigen 19-9, have been reported [3], though these were not measured in our case. Surgery was initially pursued due to the suspicion of renal cell carcinoma. Fineneedle aspiration is not useful for such primarily cystic lesions with minimal solid components [6].
Complete tumor resection with curative intent appears to be the most important therapeutic approach [7]. Depending on tumor location, size, and patient-specific factors, this may be performed minimally invasively or via open surgery, with care taken to avoid intraoperative spillage of mucinous fluid, which may contain malignant cells [7,8]. For definitive diagnosis histopathological examination is mandatory. There is no standardized follow-up protocol [6]. In our patient’s case, the interdisciplinary tumor board recommended a personalized follow-up, including abdominal sonography six months postoperatively and an abdominal CT scan twelve months postoperatively. Wolf et al. published the largest meta-analysis of primary retroperitoneal mucinous tumors in 2017, reporting a 5-year survival rate of 100% after complete resection for mucinous cystadenomas and mucinous borderline tumors, but only 68% for mucinous carcinomas [1]. Thus, adjuvant therapy plays a marginal role in the treatment regime of PRMTs with borderline malignancy compared to mucinous cystadenocarcinomas [5,6].
Conclusions
Primary retroperitoneal mucinous tumors are rare but represent a potential differential diagnosis for cystic retroperitoneal tumors. Definitive diagnosis is exclusively by histopathological examination. After complete surgical resection, the benign and low grade-malignant subtypes (mucinous cystadenomas and mucinous borderline tumors) carry an excellent prognosis. Publication of individual cases is crucial for improving diagnostic attention to and understanding of this rare disease over time.
References
- Wolf B, Kunert C, Horn LC, Einenkel J (2017) Management of Primary Retroperitoneal Mucinous Tumors: A Retrospective MetaAnalysis. International journal of gynecological cancer: official journal of the International Gynecological Cancer Society 27: 1064-1071.
- Roma AA, Malpica A (2009) Primary retroperitoneal mucinous tumors: a clinicopathologic study of 18 cases. The American journal of surgical pathology 33: 526-533.
- Son SM, Woo CG, Yun SJ, Lee OJ (2023) Primary retroperitoneal mucinous cystic neoplasm of borderline malignancy with KRAS and GNAS co-mutation: a case report. The Journal of international medical research 51: 3000605231172469.
- Zhang J, Zeng Q, Kang J, Chen J, Luo G, et al. (2023) Primary retroperitoneal mucinous cystic tumour of borderline malignancy mimicking kidney duplicate: cases report and literature review. BMC urology 23: 32.
- Dayan D, Abu-Abeid S, Klausner JM, Sagie B (2016) Primary Retroperitoneal Mucinous Cystic Neoplasm: Authors’ Experience and Review of the Literature. American journal of clinical oncology 39: 433440.
- Kavanagh TR, Nwaoduah N, Richard SD, Bowne WB, Rosenblum NG (2022) Surgical resection of a rare primary retroperitoneal mucinous borderline tumor of Müllerian Origin: A case report. Gynecologic oncology reports 44: 101104.
- Manrai M, Takesita N, Ishida H, Takashima A, Adachi T, et al. (2015) Primary retroperitoneal mucinous cystic tumors with borderline malignancy: a case report and literature review. Clinics and practice 5: 722.
- Chaves MM, Castro R, Mota-Vieira L, Carneiro V (2019) A rare case of a primary retroperitoneal mucinous cystic tumour with borderline malignancy and literature review. BMJ case reports 12: e230708.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.