Primary Orbital Rhabdomyosarcoma in Adults
by Khatib N1*, Pieters BR2,4, Tromp J3, Kloos R1, Saeed P1
1Orbital Center, Department of Ophthalmology, Amsterdam University Medical Centers, the Netherlands.
2Department of Radiation Oncology, Amsterdam University Medical Centers, the Netherlands.
3Department of Medical Oncology, Amsterdam University Medical Centers, the Netherlands.
4Cancer Center Amsterdam, Cancer Treatment and Quality of life, Amsterdam, The Netherlands.
*Corresponding author: Nur Khatib, Orbital Center, Department of Ophthalmology, Amsterdam University Medical Centers, the Netherlands.
Received Date: 05 October, 2024
Accepted Date: 16 October, 2024
Published Date: 18 October, 2024
Citation: Khatib N, Pieters BR, Tromp J, Kloos R, Saeed P (2024) Primary Orbital Rhabdomyosarcoma in Adults. Ann med clin Oncol 7: 167. https://doi.org/10.29011/2833-3497.000167
Introduction
Rhabdomyosarcoma (RMS) is a malignancy originating from primitive mesenchymal tissue. RMS is the most common soft tissue sarcoma in the pediatric population, but very rare in adults, it represents less than 1% of all solid malignant orbital tumors, which accounts for less than 4% of adult sarcomas [1,2]. Head and neck RMS(HNRMS) in adults have a poor prognosis with 5-years overall survival (OS) of 36 % [3] and nearly 50 % of adult patients already have regional or distant metastases at the time of diagnosis [4]. Case reports on treatment of orbital RMS in adults are few, [5] and case series usually consist of a mixture of different subtypes of rhabdomyosarcoma [6]. We hereby report clinical, treatment and pathological features of three adult with diagnosis of primary embryonal orbital RMS treated in our center.
Keywords: Rhabdomyosarcoma; Orbit; Sarcoma; Head and neck Rhabdomyosacoma.
Case 1:
A twenty-two-year-old female presented with unpainful left lower eyelid swelling and double vision in the last 3 months before hospital admission. On examination her right eye Best Corrected Visual Acuity (BCVA) was 1.25 and 1.0 on the left, with left restricted eye movements in up-gaze direction, swelling of her left lower eyelid and chemosis. Optic nerve function and neuroophthalmological evaluation were normal. Computer topography scan of the orbit (CT) was performed at presentation showed a noncalcified, solid extra and intraconal mass with largest tumor diameter of 4 cm in the inferior half of the left orbit, with upward displacement of the globe. There was no evidence of intracranial invasion (Figure 1). Incisional biopsy histopathology showed embryonal rhabdomyosarcoma, spindle cell type with high degree of malignancy. Microscopically the tumor consisted of small spindle shaped cells to round rhabdoblast, immunohistochemistry tests were positive for desmin, myogenin, vimentin and myoD1.
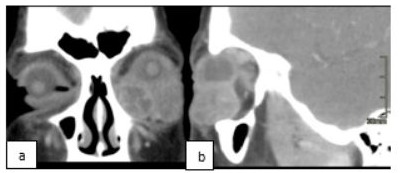
Figure 1: CT, Coronal (a) and Sagittal (b) Section, before treatment (descrpition above).
The patient was referred to the medical oncology department. After staging, local disease was diagnosed with no metastasis and she started with chemotherapy consisting of 4 cycles of ifosfamide, vincristine and actinomycin (IVA) according to Pediatric RMS regiment. After three IVA cycles, follow-up imaging magnetic resonance imaging (MRI) was evaluated which demonstrated diffuse orbital unresectable lesion. External Beam Radiotherapy (EBRT) was started with a total dose of 45 Gy, administered in 1.8 Gy doses, with continuation of the IVA chemotherapy treatment to 10 cycles in total. Good clinical and radiologically response was noted with reduction in lid swelling, conjunctival redness and radiologically stable residual imaging enhancement over a long follow-up period of 13 years with full remission. (Figure 2) At last, follow up visit (13 years) ophthalmological evaluation showed; BCVA 0.8 (at tumor side), mild dry eye according to Schirmer test evaluation, facial asymmetry due to left enophthalmos and upper eyelid hollowness, and left eye elevation limitation due to inferior oblique muscle paresis. The main patient complaints are facial asymmetry with esthetical complaints, double vision (solved by prisms) and mild photophobia due to dry eyes. The patient was treated with local lubricants and planned for reconstructive orbital surgery with 3D printed implant and fat graft injection to fix the asymmetric enophthalmos matter.
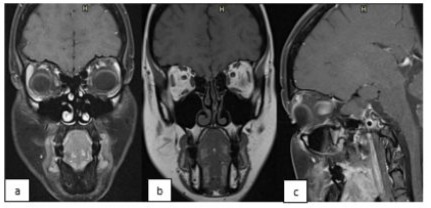
Figure 2: MRI, Coronal T1(a), Coronal T2(b) and Sagittal sections, at last follow up showing minimal residual enhancement and minimal orbital asymmetry.
Case 2:
A nineteen-year-old healthy male patient without a significant clinical history, presented with unpainful upper right progressive eyelid swelling increasing in size through several months before hospital admission. On examination his BCVA was 0.8 right eye and 1.0 left eye, full eye movements in all directions, swelling of his right upper eyelid. Optic nerve and neuroophthalmological function were normal. CT scan of orbit was performed at presentation and showed sharply delineated, noncalcified, solid extraconal mass with 2.4 cm of largest tumor diameter located in the medial half of right orbit, with lateral downward displacement of the globe without bone or intracranial invasion (Figure 3).
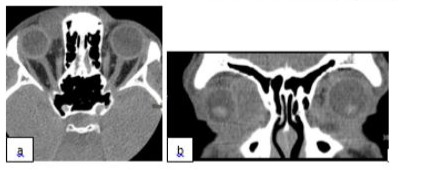
Figure 3: CT, Axial (a) and Coronal (b) Section, before treatment (description above).
Incisional biopsy histopathology showed embryonal rhabdomyosarcoma, spindle cell type with high degree of malignancy. Microscopically the tumor consisted of hyperchromatic round to spindle shaped cells to round rhabdoblast, immunohistochemistry tests were positive for desmin, myogenin, vimentin and myoD1. The patient was referred to the medical oncology department. After staging, local disease was diagnosed with no metastasis, and he started with chemotherapy consisting of 9 cycles of IVA. After three IVA cycles, good response was noted with reduction in lid swelling clinically and demonstrated localized orbital tumor shrinkage. Then EBRT 50.4 Gy administered in 1.8 Gy fractions was done. During 12 years of follow-up, imaging MRI showed stable residual enhancement (Figure 4) with complete tumor remission. Last ophthalmic evaluation was normal with BCVA 0.8 (at tumor side) and no complaints.
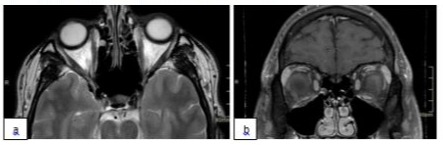
Figure 4: MRI, axial(a) and coronal(b) section, last follow up MRI after treatment showing minimal medial residual enhancement in T2 with contrast.
Discussion
We report two cases of primary orbital RMS in adults. RMS is rare among adults and considered as a disease of young children, which occurs at mean age of 8 years [7]. Orbital involvement is one of the most favorable locations in children, with high survival rate (>90%). Several large retrospective studies, comprising more than a hundred patients, have reported the prognosis of adult RMS, but the outcome of adult orbital RMS is still unclear because of its rarity [3]. A large single-institution study has demonstrated very poor outcome of head and neck RMS in adults, with a 5-year overall survival (OS) of only 36% [3]. This low rate among adults in comparison to pediatric can be explained by different facts. The fact of unfavorable histological subtype that may place adults at disadvantage in which adults have more alveolar subtype (3650%) in comparison to pediatric RMS (5-30%) in which affect the survival rate among adults [3,5]. More than 70% of pediatric patients with localized RMS can be cured because of the high sensitivity to chemotherapy and radiotherapy. In contrast, according to literature treatment of soft tissue sarcoma in adults is mostly based on surgery as well as on radiation and less sensitive to chemotherapy [3]. To date, some benefits resulting from adjuvant chemotherapy have been demonstrated in adults with RMS, but the effect is not as good as it is for children with RMS [1,2,4,8]. An adult could tolerate chemotherapy designed for children to a lesser extent, with more side effects that cause early treatment cessation with as result a suboptimal treatment. Most of the studies are retrospective and it is difficult to understand retrospectively a patient’s clinical status and feasibility for aggressive chemotherapy treatment [9]. This fact might have effect on lower survival rate among adults. Moreover, the clinical feature of adult RMS has higher metastasis in comparison to RMS in children, in which 46% of adult RMS have regional lymph node involvement versus 27% in children, and distance metastases at diagnosis is 30% vs 20% in adulthood and childhood respectively, [10].
The use of exact chemotherapy guidelines has been major point of discussion and debate in adult RMS. Hawkins et al. have concluded that there is no evidence that chemotherapy provided any survival benefit for adult patients with RMS [11], on the other hand, a large series of Ferrari et al. showed a favorable outcome of adult RMS patients who were treated according to guidelines for pediatric RMS, with high chemotherapy sensitivity of 85% [12]. Also, Naamit et al. showed improvement in survival rate among adult patients with nonmetastatic disease treated by RMS children’s protocol [13]. These findings may provide some evidence that the principle of treatment for adult with RMS may follow the principle of paediatric RMS treatment. The treatment of our cases was according to pediatric treatment protocol at our center. patients were required to begin therapy with chemotherapy, radiation and /or surgery once the diagnosis is confirmed. Delayed surgery was recommended, after chemotherapy (ideally after 3-4 courses) if the tumor was resectable. Radiotherapy (fractionation doses of 1.8-2.0 Gy, and total doses - 50 to 60 Gy) was offered in all cases. The suggested doses of chemotherapy were: ifosfamide 3 g/m2 twice a day (twice a day), vincristine 1.5 mg/m2 (max 2 mg) once a day (once a day) and actinomycin-D 1.5 mg/m2 (max 2 mg) once a day. Chemotherapy was delivered in 9 to10 courses (administered every 3 weeks) [14,15]. Prognostic factors that affect survival rate of adult RMS are similar to children’s which include age, para- meningeal involvement, TNM staging, Intergroup RMS Study Group (IRSG) stage, and histological subtype [16]. The staging of RMS in our cases were in accordance with the staging system for children, which was based on the IRSG and TNM staging system. The two cases represented by us were non metastatic T1bN0M0 and IRS III group (incompletely resected tumour, primary incisional biopsy). The two cases had long term complete remission with no recurrence episodes, these results can be explained by: the good prognostic features of our reported cases, early malignancy treatment according to RMS children protocol and the close follow up by multidisplinary team involving the oncologist from early stage. Because of the absence of controlled, prospective trials, which is due to extreme rarity of the disease, our treatment approach was according to pediatric protocols. From our children RMS experience, orbital RMS are usually incompletely resected (group III), therefore it is necessary to treat with postoperative chemotherapy and radiotherapy. We consequently believe that adult RMS patients should always be considered at higher risk even in localized disease and the adult age per se should be seen as an important prognostic factor. A more appropriate use of standard therapies (pediatric protocols) may improve the outcome to some degree, but new adult tailored therapies are needed, and a better understanding of the biology of the disease will be crucial to improve the treatment outcome, and therefore prospective studies are needed to test this approach.
Reference
- Shields JA, Shields CL (2003) Rhabdomyosarcoma: review for the ophthalmologist. Surv ophthalmol 48: 39-57.
- Hawkins WG, Hoos A, Antonescu CR, Urist MJ, Leung DH, et al. (2001) Clinicopathologic analysis of patients with adult rhabdomyosarcoma. Cancer 91: 794-803.
- Wu Y, Li C, Zhong Y, Guo W, Ren G (2014) Head and Neck Rhabdomyosarcoma in Adults. Craniofacial Surg 25: 922-925.
- Wu TH, Huang JS, Wang HM, Wang CH, Yeh KY, et al. (2010) Long term survivors of adult rhabdomyosarcoma of maxillary sinus following multimodal therapy: case reports and literature reviews. Chang Gung Med J 33: 466-471.
- Liu W, Jiang L, Jin Y, Yang B, Lai TY (2016) alveolar rhabdomyosarcoma of the sphenoid sinus mimicking optic neuritis presenting with intermittent visual loss in an adult. OncoTargets and Therapy 9: 63336336.
- De Bree R, van der Waal I, de Bree E, Leemans CR (2010) Management of adult soft tissue sarcomas of the head and neck. Oral Oncol 46: 786-790.
- McDonough RL, Leib ML (1995) Atypical presentation of orbital rhabdomyosarcoma: A report of two cases. J Pediatr Ophthalmol Strabismus 32: 262-265.
- Yunteng Wu, Chaojun Li, Yi Zhong, Wei Guo, Guoxin Ren (2014) Head and Neck Rhabdomyosarcoma in Adults. J Craniofac Surg 3: 922-925.
- Prestidge BR, Donaldson SS (1989) Treatment results among adults with childhood tumors: a 20-year experience. Int J Radiat Oncol Biol Phys. 17: 507-514.
- Bergamaschi L, Bertulli R, Casanova M, Provenzano S, Chiaravalli S, et al. (2019) Rhabdomyosarcoma in adults: analysis of treatment modalities in a prospective single‐center series. Med Oncol 36: 59.
- Hawkins WG, Hoos A, Antonescu CR, Urist MJ, Leung DH, et al. (2001) Clinicopathologic analysis of patients with adult rhabdomyosarcoma. Cancer 91: 794-803.
- Ferrari A, Dileo P, Casanova M, Bertulli R, Meazza C, et al. (2003) Rhabdomyosarcoma in adults A retrospective analysis of 171 patients treated at a single institution. Cancer 98: 571-580.
- Gerber NK, Wexler LH, Singer S, Alektiar KM, Keohan ML, et al. (2013) Adult Rhabdomyosarcoma Survival Improved With Treatment on Multimodality Protocols. Int J Radiation Oncol Biol Phys 86: 58-63.
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, et al. (2000) New guidelines to evaluate the response to treatment in solid tumors (RECIST Guidelines). J Natl Cancer Inst 92: 205-216.
- Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, et 16. Liu YT, Wang CW, Hong RL, Kuo SH (2019) Prognostic Factors and al. (2009) New response evaluation criteria in solid tumors: revised Treatment Outcomes of Adult Patients With Rhabdomyosarcoma After RECIST guideline (version 1·1). Eur J Cancer 45: 228-247. Multimodality Treatment. Anticancer Res 39: 1355-1364.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.