Predictors of In-Hospital Length of Stay among Cardiac Patients: A Machine Learning Approach
by Alice Constance Mensah1*, Lydia Sarponmaa Asante2, Ebenezer Darkoh1
1Applied Mathematics and Statistics Department, Accra Technical University, Ghana
2Department of Public Health, Catholic University of Ghana
*Corresponding author: Alice Constance Mensah, Applied Mathematics and Statistics Department, Accra Technical University, Ghana
Received Date: 14 September, 2025
Accepted Date: 22 September, 2025
Published Date: 26 September, 2025
Citation: Mensah AC, Asante LS, Darkoh E (2025) Predictors of In-Hospital Length of Stay among Cardiac Patients: A Machine Learning Approach. J Community Med Public Health 9: 535. https://doi.org/10.29011/2577-2228.100535
Abstract
Purpose: Cardiovascular diseases remain a major cause of morbidity and mortality and are currently a significant strain on the healthcare system. Knowledge of the predictors of LoS is important to streamline care, resource utilization and the outcomes of the patients. The purpose of this study was to determine socio-demographic factors that could be used to predict LoS among patients with heart-related conditions in the Greater Accra Region in Ghana using machine learning methods. Methods: A retrospective study was done through the hospital records of patients with heart related diseases admitted between January 1st 2022 and December 31st, 2023 from the District Health Information Management System (DHIMS2). Three predictive models, the Decision Tree, Random Forest, and the Linear Regression, were used to assess the determinants of the LoS. Results: The average LoS was 5.5 days. The highest prevalence of diagnoses was hypertensive heart disease (56%) and heart failure (31%) in both genders. Age, educational attainment, and occupational status were found important determinants of LoS. Tertiary-educated and formally employed patients had the longest admissions. Interaction effects showed lower LoS in younger employed patients, and highly educated in the informal economy. The decision tree model yielded the best prediction (R2 = 37.97%). Conclusion: Decision trees may serve as an effective machine learning model to point at the complicated and non-linear predictors of LoS of cardiac patients. These results stress the significance of developing a resource planning and discharge plan based on the socio-demographical characteristics of the patients.
Keywords: Cardiovascular diseases; Length of Stay; Machine Learning; Age; Educational Attainment; Occupation
Introduction
Cardiovascular Diseases (CVDs) refer to a set of heart and blood vessel conditions. They are: coronary heart diseases, cerebrovascular diseases, peripheral arterial diseases, rheumatic heart diseases; congenital heart diseases; deep vein thrombosis and pulmonary embolism [1-4]. CVDs are the primary cause of death worldwide and it is estimated that 17.9 million individuals died due to CVD in 2019, constituting 32 percent of all global mortalities. Among them, 85 percent was attributed to heart attack and stroke and that more than three quarters of CVD deaths occur in low- and middle-income countries [1].
In Ghana, both Korle-bu Teaching Hospital (KBTH) and Komfo Anokye Teaching Hospital (KATH) have reported that CVD and risk factors including hypertension, diabetes and obesity are on the rise, particularly in middle-aged Ghanaians [5]. A systematic review conducted by Doku et al (2024) [6], a Pooled Prevalence of 10.34% for CVD and Compelling interventions to prevent and manage the high burden of CVD and its risk factors were reported. Hypertension is a major public health problem in Ghana and it represents the main cause of hospitalization and fatalities in Ghana [7,8]. CVD hospitalization like any other health condition causes direct healthcare cost since such a condition will require the use of clinical resources to deal with the condition and quality of care.
Length of stay (LoS) refers to the number of days an inpatient will remain in the hospital in a single admission event, or the time between admission and discharge (i.e., total bed-days of patient stay). LOS is the time spent in a hospitalization event and varies according to various factors, both inside and outside the hospital, which are connected to capacity management and resource planning [9-13]. The metric is therefore regarded as a significant indicator used to measure quality of care, which is important in measuring the use of resources in hospitals and the performance of the hospitals. LoS may be applied to difficult to measure study endpoints like mortality and illness severity [14,15]. LoS is also significant in a patient flow that describes the way a patient moves through a sequence of procedures [16,17]. Although CVD is increasingly becoming a burden and economically significant in developing nations such as Ghana, limited or disparate data are available on the LOS and its factors among patients. When considering an intervention to minimize the LOS of hospitalized patients with heart diseases, it is important to consider the risk factors of the individual patients with prolonged LOS and begin with addressing those risk factors. Several studies have found that a wide range of factors affect LoS, such as socio-demographic, medical, social, and institutional ones [18-23]. It can also assist in making accurate predictions that can aid in determining patients that might need extended hospital stays so that the necessary action can be taken to help improve patient care. Consequently, the LoS of hospitalized patients with a specific disease contributes to the morbidity and mortality of the disease in the population.
The benefit of machine learning algorithms is the availability of a highly flexible predictive tool based on a large volume of Electronic Health Records (EHR) [24,25]. Over the past few years, models of machine learning such as the decision tree (DT), logistic regression (LR), random forest (RF), Naive Bayes (NB) and support vector machine (SVM) models have been found to equally perform in the disease prediction [26-27] and in the LOS prediction in hospitals [10, 28-31].
Despite the growing burden and economic impact of CVD in developing countries including Ghana, overall studies on LoS based on a general and entire hospital population are rare. The main gap in the literature is that most methods focus on predicting the LoS only for specific condition or restrict their analysis to data from specific hospitals. Daghistani, et al., Corrà, et al. and Hachesu, et al., developed a machine learning model to predict length of stay for cardiac patients; a meta-analysis of existing literature on factors influencing length of stay of cardiac surgery patients was studied [32]; other studies, [30, 33 - 35] were on the assessment of factors influencing hospitalization length of admissions due to hypertension and heart failure, and another study looked at the LoS at medical wards, [36]. Mostly, LoS is unknown at the time of admission and there is the need to investigate the prediction of the patients’ LoS from variables collected at the time of admission to build a predictive model through machine learning techniques. Providing an intervention to reduce the LOS of hospitalized patients with heart diseases identifying and targeting the individual patients’ risk factors for LOS is the beginning and it would provide data for clinicians on which factors they should target in reducing the LOS of their patients. Therefore, this study was conducted to explore the application of ML techniques for classifying the LOS of patients with various and freely available data on cardiovascular diseases into socio-demographic categories and to account for interaction effects, not just main effects, in accurately analyzing and modeling LOS. The authors employed Random Forest, decision tree and linear regression models on a data-set obtained from the DHIMS2 in the Greater Accra region.
Methodology and Data Processing Study setting and sampling
This is a descriptive retrospective study on patients admitted between January 1st, 2022 and December 31st, 2023 with confirmed heart related conditions admitted to various health facilities in the Greater Accra region of Ghana. The study employed data from District Health Information Management System (DHIMS2) of the Ghana Health Service which is the nation’s most comprehensive database on routine health data. The DHIMS2 data-set contains, among other items, the facility name, year of admission, date admitted and discharged, age of patient, gender, educational level, occupation, principal diagnosis, additional diagnosis, insurance status, and outcome of admission (discharged or death). The length of stay variable was obtained as a result of subtracting admitted date from the discharged date.
Study variables
Dependent variable
Length of hospital stay (days) was the dependent variable and described as the duration of a single episode of hospitalization, calculated by subtracting the date of admission from the date of discharge or death.
Independent variables
The independent variables were the patients’ Socio-demographic variables: Age, occupation, gender, educational level, diagnosis, and insurance status. Morbidity and diagnosis are represented by the chapters of the International Statistical Classification of Diseases (ICD) and Related Health Problems created by the World Health Organization (WHO) to universally standardize diseases.
Performance Measures
To assess the performance of the models, diverse evaluation metrics were employed, such as R-squared (R2), for classification tasks, Mean Absolute Error (MAE), Mean Squared Error (MSE), and Root Mean Squared Error (RMSE) for regression tasks. MAE evaluates the average absolute deviation between actual and predicted data, the MSE measures the average squared variance between observed data and predicted data as seen in equation 2. Whiles R2 quantifies the proportion of total variance in the dependent variable that is attributable to the independent variables. The RMSE metric quantifies the degree of agreement between predicted values and actual results.

Let yi represent the predicted value for the ith observation and ˆyi represent the actual value. Considering N observations with mean observed value ̄y,


According to Géron, the RMSE is the performance metric generally used for regression models; however, in some contexts, it is preferable to use the MAE due to its low sensitivity for atypical data. It is also noteworthy the predominance of the use of R2 in articles that perform the LOS-P prediction [37].
Statistical analysis
Descriptive statistics were conducted for all the variables, both
independents and dependent. Frequency distribution in the form of count and percentages were recorded for the categorical dependent variable. Mean, standard deviation, skewness and histograms were computed and built for the continuous variables. Furthermore, regression tree model was developed for the prediction of length of hospital stay for heart-related patients. Root Mean Square Error (RMSE), Mean Absolute Error (MAE), Mean Squared Error (MSE), and R-Square values were used to access the performance of the regression tree and compared them with traditional regression model and random forest model. The statistical analysis in this study were done using the statistical environment R version 4.5.0 and R-Studio version 2024.12.1+563.
Results
Socio-demographic information for all the participants is shown in Table 1. Out of all the patients who were hospitalized, women formed 51.1% and men 48.9%. This balance helps to justify the gender neutrality of the study sample and allows genderbased, comparative analysis of results. A large percentage of the participants have no formal education 40.7% and only 9% having tertiary education. The majority of the participants were retirees 33.2%, as well as those with healthcare insurance, 67.2%. Such distribution implies that the population consists of older people or economically inactive people, which might affect the healthcare usage and stay.
|
|
|
Frequency N = 1044 |
Percentage (%) |
|
Occupation |
Formal Workers |
68 |
6.5 |
|
|
Informal Workers |
237 |
22.7 |
|
|
Pupil/Child |
87 |
8.3 |
|
|
Retired |
347 |
33.2 |
|
|
Student |
11 |
1.1 |
|
|
Unemployed |
84 |
8.0 |
|
|
Unspecified |
210 |
20.1 |
|
Gender |
Male |
511 |
48.9 |
|
|
Female |
533 |
51.1 |
|
Educational Level |
Basic School |
230 |
22 |
|
|
JHS/Middle School |
104 |
10 |
|
|
None |
425 |
40.7 |
|
|
Senior High Sch |
164 |
15.7 |
|
|
Technical/Vocational |
26 |
2.5 |
|
|
Tertiary |
95 |
9.1 |
|
Insurance Status |
Insured |
702 |
67.2 |
|
|
Not Insured |
342 |
32.8 |
Table 1: Descriptive Characteristics of the Study Participants.
Figure 1 presents a comparative analysis of the distribution of heart-related diagnoses across male and female patients, expressed as percentages. It illustrates that Hypertensive Heart Disease (I11.9) is the most prevalent condition in both genders, accounting for 57.4% of diagnoses among females and 54.6% among males, indicating a slightly higher burden among women. Heart Failure (I50.9), Acyanotic Congenital Heart Disease (Q24.9) and Disease Rheumatic Heart (I09.9) show slightly higher percentages among males compared to females. This result indicated in figure 1 suggests hypertensive and heart failure conditions dominate the diagnostic landscape for both genders and subtle gender differences in the prevalence of less common heart conditions. This pattern or realization underscores the need for gender-sensitive approaches in cardiovascular disease prevention and management.
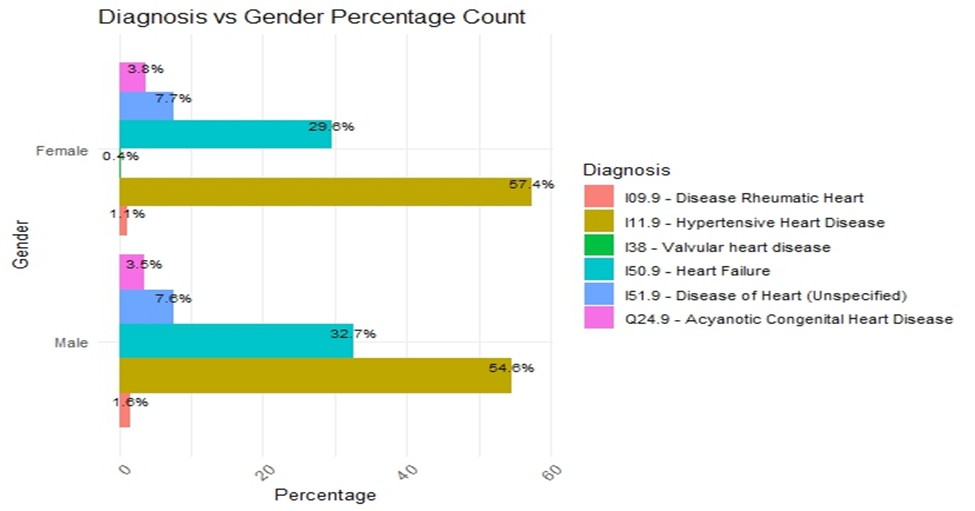
Figure 1: Gender-based Distribution of Heart Disease Diagnoses.
The violin plot in figure 2 presents the distribution of patient age across various heart-related diagnoses, integrating density curves with embedded boxplots to convey both the spread and central tendency of age within each diagnostic group. It shows that age distribution varies considerably by condition and underscores age as a significant factor differentiating the burden and nature of cardiovascular conditions, offering visual insight into age-related trends in disease presentation. For instance, Q24.9 – Acyanotic Congenital Heart Disease is strongly associated with younger patients, whereas I11.9 – Hypertensive Heart Disease and I50.9 – Heart Failure affect older individuals. Furthermore, I38 – Valvular Heart Disease is seen to affect those in the middle age.
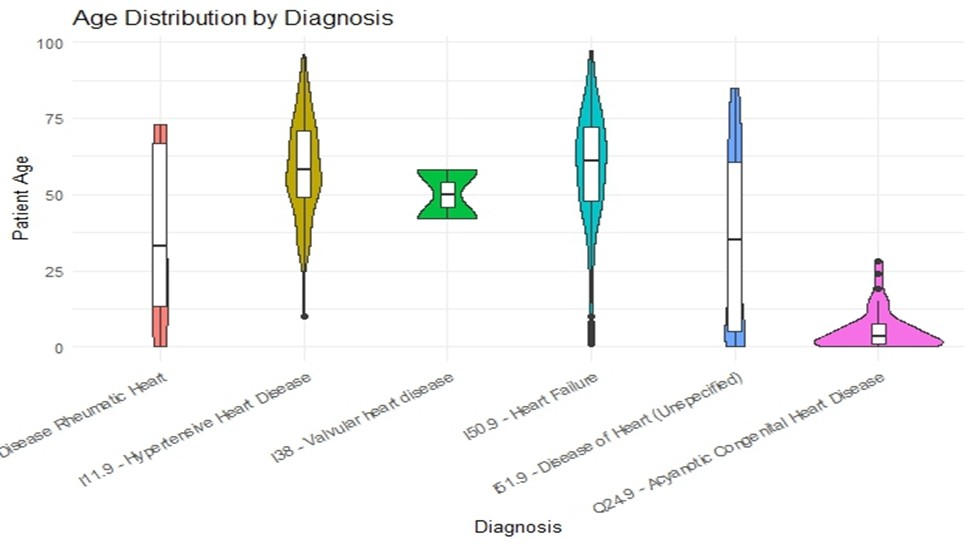
Figure 2: Age Distribution Patterns across Heart Disease Diagnoses.
From figure 3, heart-related patient had a mean age of approximately 54.53 years (S.D.±21.67), indicating a moderate spread around the mean age. The age distribution exhibited a slight negative skewness = -0.79, suggesting that while most patients were middle-aged to older adults, there were some younger patients who pulled the distribution slightly to the left. Length of hospital stay demonstrated a mean of 5.54 days (S.D.± 8.92), reflecting a wide variation in stay duration among patients. The skewness was 5.38, indicating a highly positively skewed distribution. This suggests that while the majority of patients had short hospital stays, a small number experienced much longer stays, significantly stretching the distribution to the right.
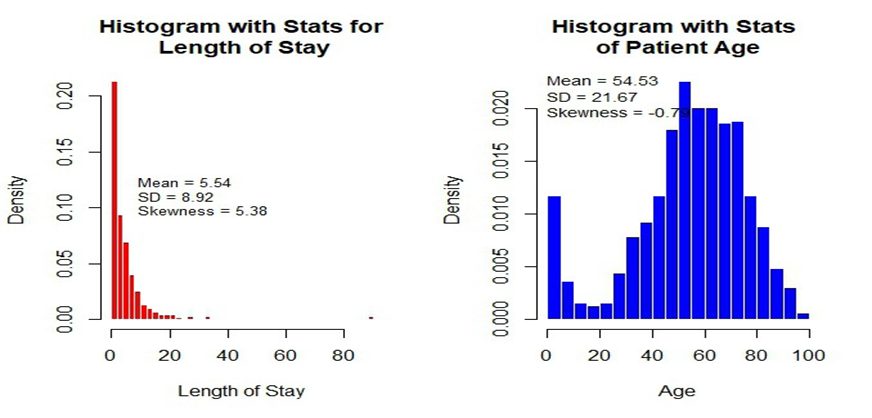
Figure 3: Distribution of Patient’s Hospital Length Stay and Age.
A heat-map visualization in figure 4 demonstrates the average length of stay (LoS) in hospital by different educational attainment level and different cardiac diagnoses combinations. Gradient of color indicates an average LoS, whereas the color shades of deeper red indicate considerable periods of hospitalization duration. The analysis shows high LoS heterogeneity across stratification in education, patients with tertiary education had the highest mean LoS of 13.5days among I51.9 - Heart disease (unspecified). Conversely, individuals with less formal education (those with no schooling and basic education) consistently exhibited shorter hospitalization periods across the majority of cardiac diagnoses examined. These disparities may reflect variations in health literacy levels, care-seeking behaviors, treatment adherence, or differential access to comprehensive cardiac management protocols. This pattern deserves consideration of underlying mechanisms that may influence care utilization and clinical outcomes, and may inform targeted interventions to optimize care delivery across diverse educational populations.
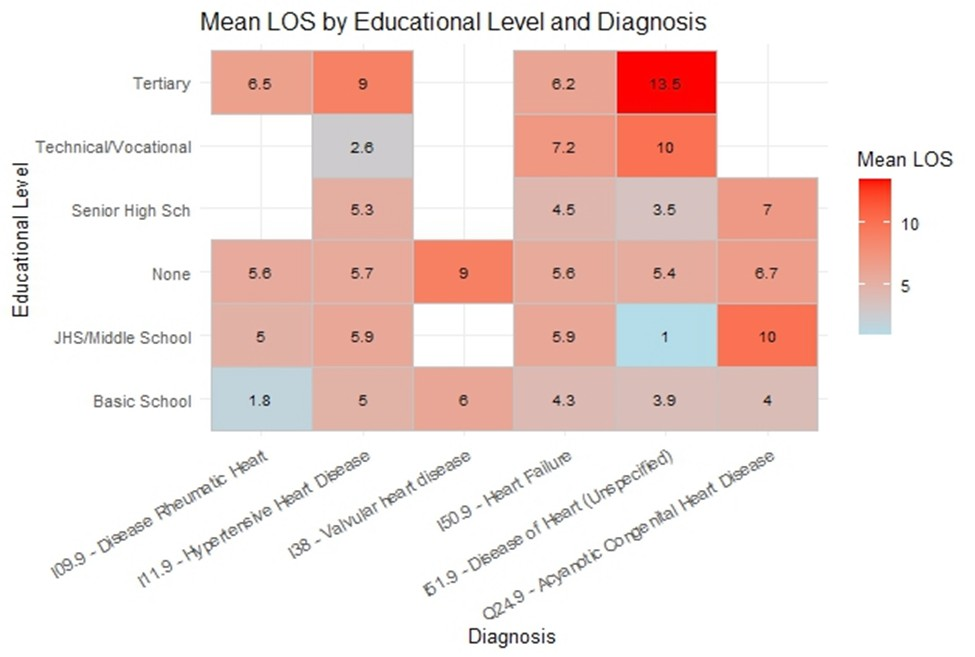
Figure 4: Mean Length of Stay by Educational Level and Diagnosis.
The results from figure 5 indicates that formal workers exhibited the longest mean stays across several diagnostic categories, peaking at 12.5 days for patients diagnosed with I51.9 - Heart disease (unspecified). Retirees also experienced prolonged hospitalizations, especially in I09.9 rheumatic heart and I51.9 - Heart disease (unspecified), with stays of 8.5 and 7.1 days respectively, likely reflecting age-related vulnerabilities. In contrast, unemployed and Pupil/Child groups tend to have shorter average stays, with minimum duration as low as 1 day for Q24.9 – Acyanotic Congenital Heart Disease among the Unemployed. The relatively brief stays in these groups may reflect either milder disease presentations or differences in healthcare access and admission thresholds. Overall, occupation is associated with hospital length of stay among patients with heart-related diagnoses. These patterns highlight the need to consider socioeconomic and demographic factors when planning healthcare resource allocation and discharge planning.
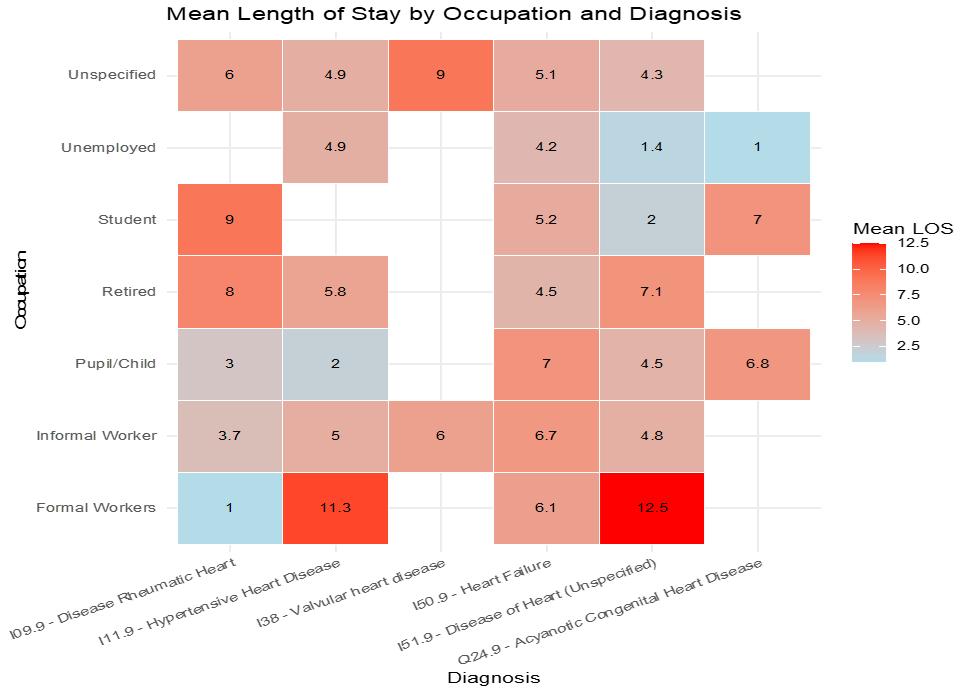
Figure 5: Mean Length of Stay by Occupation and Diagnosis.
The regression decision tree model identifies key factors associated with the length of hospital stay (LoS) among patients admitted with heart-related conditions. The most significant predictor at the root of the tree was occupation, which separated patients into two groups: informal workers (including pupils, children, retired individuals, students, unemployed, and unspecified occupations) and formal workers (Figure 6).
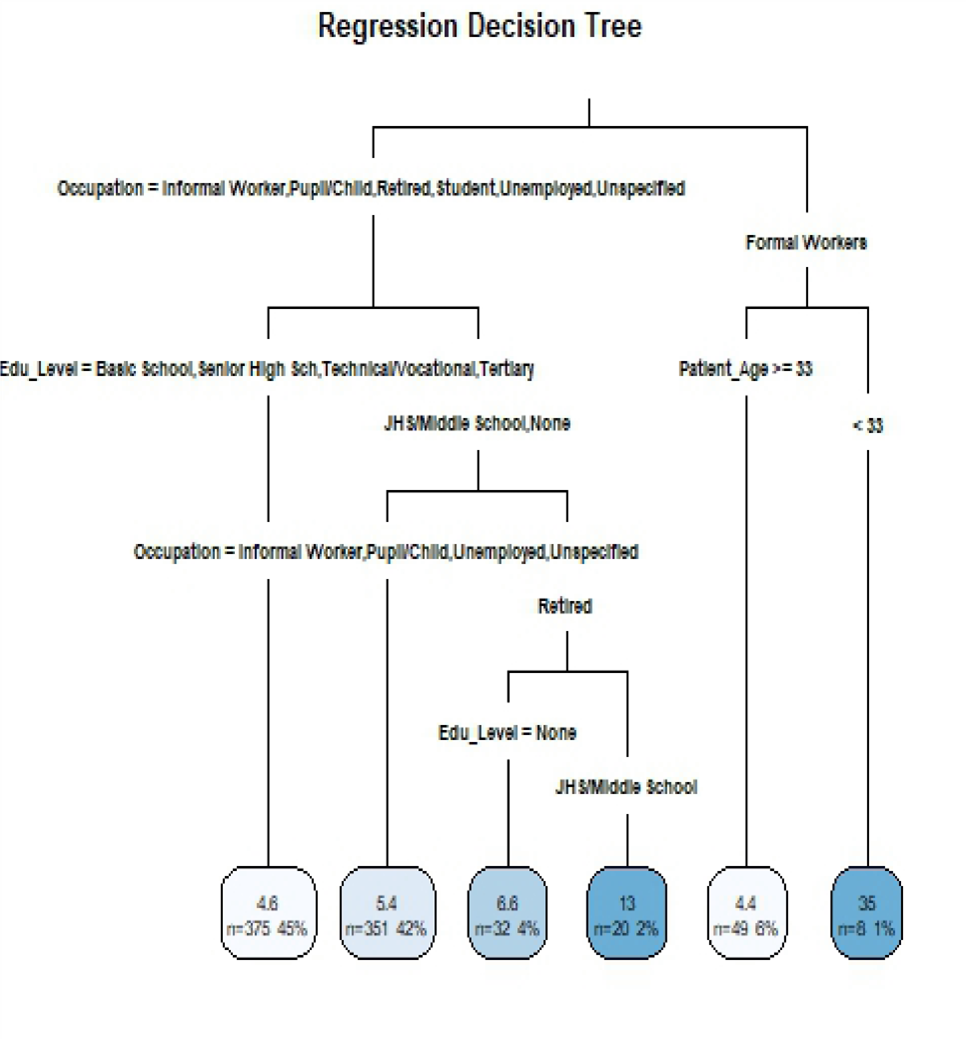
Figure 6: Regression Tree for Heart-Related Patient Hospital Length of Stay.
Among informal workers, educational level further differentiated LoS outcomes. Patients with at least senior high school education had a mean LoS of approximately 4.6 days, whiles those with basic or no formal education had longer mean LoS of 5.4 days. Within this group, retired individuals were particularly notable; retired patients with no formal education had an average LoS of 6.6 days, while those with junior high/middle school education experienced the longest hospitalizations, averaging 13 days.
Although gender and insurance status were included during model development, they did not emerge as significant splitting variables in the final tree structure, suggesting they were not primary determinants of hospital LoS in this cohort.
The results in table 2 reveals interesting differences in performance across the various metrics, where for all the measures, Decision Tree model always performs better than the Linear Regression and the Random Forest models. Notable amongst them is the Decision Tree model best explained the variance of Length of Stay (R2 = 37.97%), by far outweighing the explanatory capacity of both the Random Forest (R2 = 16.55%) and Linear Regression (R2 = 3.81%). Combined these results indicate that the Decision Tree can not only most accurately predict the outcome but it also characterizes the underlying variability in Length of Stay better than the other models.
|
Model |
MAE |
MSE |
RMSE |
R-squared |
|
Linear Regression |
4.719968 |
72.63925 |
8.522866 |
0.038109 |
|
Decision Tree |
4.446082 |
56.47933 |
7.515273 |
0.379699 |
|
Random Forest |
4.628285 |
65.99046 |
8.123451 |
0.165495 |
Table 2: Comparison of Model Performance.
In this study, segmented analysis was conducted across the three variables found to be most significant in predicting Length of Stay (LoS) among heart-related admissions: Age, Occupation, and Educational Level. By analyzing these variables individually and in combination, it helps to reveal important patterns in patient hospitalization duration. Focusing on RMSE, which quantifies the average magnitude of prediction errors, the lower RMSE suggests that the factors influencing Length of Stay for individuals in this category are more consistent and better captured in the data-set, allowing for more accurate predictions.
Educational Level Specific Segmented Model Performance Using RMSE
From figure 7, those with basic level of education shows the lowest RMSE, indicating better model performance for this education level than the Tertiary group which exhibits the highest RMSE, signalling the model’s poor performance in predicting Length of Stay for individuals with tertiary education.
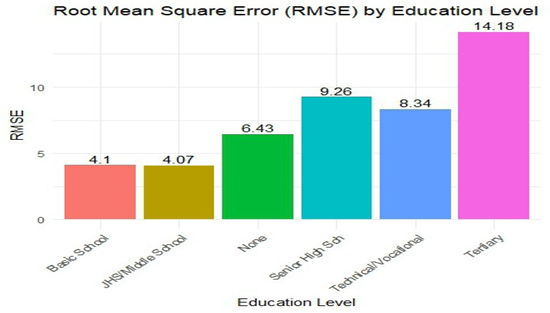
Figure 7: Root Mean Square Distribution of Education Specific Segmented Model Performance.
Age Specific Segmented Model Performance Using RMSE
The RMSE values across different age groups show notable variations in the model performance in figure 8. The least (4.38) and the highest (10.58) RMSE in the age category was in the 70+ and the 30-49 age groups respectively. Thus, the model provides the most accurate predictions for individuals in above 70 age group as against the 30-49 age group.
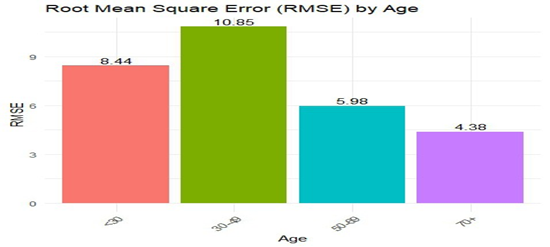
Figure 8: Root Mean Square Distribution of Age Specific Segmented Model Performance.
Occupation Specific Segmented Model Performance Using RMSE
Figure 9 presents the Root Mean Square Error (RMSE) values of predictions stratified by occupation categories. Among all occupational groups, the prediction error is highest for formal workers, with an RMSE of 20.71, significantly higher than any other category. Overall, figure 9 highlights the importance of occupation as a stratifying factor in model accuracy and suggests that more attention may be needed in modeling for formal workers.
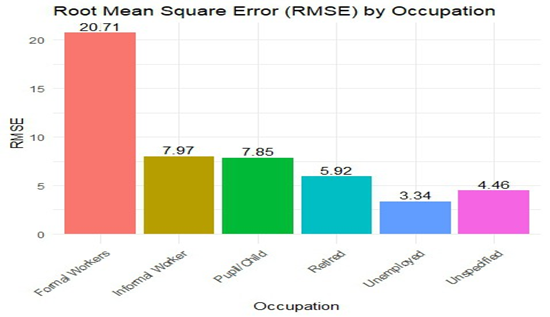
Figure 9: Root Mean Square Distribution of Occupation Specific Segmented Model Performance.
Discussion
This study focused on patients diagnosed of heart related diseases and have been hospitalized. Despite the increase in CVDs and a growing burden on the health care systems, very few studies have attempted to identify the factors associated with longer lengths of hospital stay, across all ages, occupation and educational level. This discussion is based on studies aimed at factors influencing LoS whether for a specific disease or admission department.
The descriptive results revealed a mean age of approximately 54.53 years and the overall mean duration of hospital Length of stay was 5.54 days. Hypertensive Heart Disease is the most prevalent condition in both genders, accounting for 57.4% and 54.6% of diagnoses among females and males, followed by Heart failure with 32.7% of male and 29.8% of female patients affected. However, gender did not emerge as significant splitting variable in the final tree structure, suggesting they were not primary determinants of hospital LoS in this cohort. This result is consistent [23], but inconsistent with [14,19,21]. The results found that, age as a significant factor [22,23] and a differentiator in the burden and nature of cardiovascular conditions. For instance, Acyanotic Congenital Heart Disease is strongly associated with younger patients, in contrast, hypertensive Heart Disease and Heart Failure affect older individuals.
LoS is heterogeneous across education level, with highest mean LoS of 13.5days among patients with tertiary qualification and diagnosed of Heart disease.
The application of decision tree model to the data set found age, occupation and educational level as significant factors that are related to the length of stay in the health facilities in the Greater Accra Region. The analysis on interaction effects employed machine learning algorithms among age, education and occupation showed that among informal workers, patients with at least senior high school education had a mean LoS (4.5) less than those with basic or no formal education (5.4) days. Retired patients with no formal education had an average LoS less than those with junior high/middle school education. Patients aged less than 33years and in formal employment exhibited mean LOS of 3.5 days as against 4.6 days for patients aged 33 years and above and also in formal employment. This means LoS increases with advancement in age, [19,21-23,28].
Among the 3 models, Decision Tree model always performs better than the Linear Regression model and the Random Forest model. The Decision Tree had smallest Mean Absolute Error, the lowest Mean Squared Error and the best Root Mean Squared Error. In addition, the Decision Tree model best explained the highest variance of Length of Stay (R2 = 37.97%), signifying that the Decision Tree can not only most accurately predict the outcome but it also characterizes the underlying variability in Length of Stay better than the other models. Linear Regression performed the worst with the highest RMSE and the lowest R2, depicting a very insufficient fit of the data and that the fundamental patterns are not well transferred into the linear assumptions.
Conclusion
Demographic factors such as age, occupation and level of education were important factors that needed to be considered to reduce the length of stay of patients diagnosed of heart related diseases. It is possible to formulate a machine learning model to predict the anticipated length of stay in the hospital for each patient. Among the three models evaluated, the Decision Tree model demonstrated superior performance and is therefore recommended for predicting the target variable. Its relatively higher explanatory power and lower prediction errors make it the most suitable model for this analysis. Further model optimization and cross-validation may enhance predictive accuracy. This can be used in clinical bed management and resources allocation.
In terms of policy, prioritize early discharge planning and followup care for patients with predictors of longer LoS (e.g., elderly, highly educated and formal employment). Introduce age- and education-sensitive interventions, such as counseling, social support, youth-friendly health services etc. there is also the need to leverage the regression tree model for hospital resource planning and patient risk stratification.
Ethical Considerations
The use of the data for the study was approved by the Ghana Health Services Ethical Review Committee.
Competing Interests
The authors declare that they have no financial or personal relationships that might have inappropriately influenced them in writing this article.
Funding
This study was conducted without any external funding. All resources utilized for the study were self-funded by the authors.
Authors’ Contributions
All authors contributed to this project and article equally. All authors read and approved the final manuscript.
Acknowledgements
We express gratitude to the research department of the Ghana Health Services, Greater Accra Region for facilitating the implementation of this study by providing the data and administrative authorization.
References
- World Health Organization (2021) Cardiovascular diseases (CVDs).
- Angaw DA, Ali R, Tadele A, Shumet S (2021) The prevalence of cardiovascular disease in Ethiopia: a systematic review and meta-analysis of institutional and community-based studies. BMC Cardiovasc Disord 21: 37.
- Regassa LD, Tola A, Ayele Y (2021) Prevalence of cardiovascular disease and associated factors among type 2 diabetes patients in selected hospitals of Harari region, eastern Ethiopia. Front Public Health 8: 532719.
- Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, et al. (2018) Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 137: e67-e492.
- Abban HA, Harrison OA, Vuvor F, Samuel O-N, Asiedu MS (2021) Risk Factors for Cardiovascular Diseases in Ghana. Sci Dev J 5: 1-11.
- Doku A, Tuglo LS, Boima V, Agyekum F, Aovare P, et al. (2024) Prevalence of Cardiovascular Disease and Risk Factors in Ghana: A Systematic Review and Meta-analysis. Glob Heart 19: 21.
- Bosu WK, Bosu DK (2021) Prevalence, awareness, and control of hypertension in Ghana: A systematic review and meta-analysis. PLoS One 16: e0248137.
- Atibila F, Hoor GT, Donkoh ET, Wahab AA, Kok G (2021) Prevalence of hypertension in Ghanaian society: a systematic review, meta-analysis, and GRADE assessment. Syst Rev 10: 220.
- Hautz WE, Kämmer JE, Hautz SC, Sauter TC, Zwaan L, et al. (2019) Diagnostic error increases mortality and length of hospital stay in patients presenting through the emergency room. Scand J Trauma Resusc Emerg 27: 54.
- Daghistani TA, Elshawi R, Sakr S, Ahmed AM, Al-Thwayee A, et al. (2019) Predictors of in-Hospital Length of Stay among Cardiac Patients: A MachineLearning Approach. Int J Cardiol 288: 140-147.
- Turgeman L, May JH, Sciulli R (2017) Insights from a machine learning model for predicting the hospital Length of Stay (LOS) at the time of admission. Expert Syst Appl 78: 376-385.
- Bueno H, Ross JS, Wang Y, Chen J, Vidán MT, et al. (2010) Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA 303: 2141-2147.
- Abdul-Afeez SO, Omoniyi OK, Akinyemi OO, Obembe TA, Adeniji FI (2017) What factors influence the average length of stay among stroke patients in a Nigerian tertiary hospital? Pan Afr Med J 26: 228.
- Lim A, Tongkumchum P (2009) Methods for analyzing hospital length of stay with application to inpatients dying in Southern Thailand. Global J Health Sci 1: 27.
- Chang K-C, Tseng M-C, Weng H-H, Lin Y-H, Liou C-W, et al. (2002) Prediction of length of stay of first-ever ischemic stroke. Stroke 33: 2670-2674.
- Awad A, Bader–El–Den M, McNicholas J (2017) Patient length of stay and mortality prediction: a survey. Health Serv Manage Res 30: 105120.
- Chaou CH, Chen HH, Chang SH, Tang P, Pan SL, et al. (2017) Predicting length of stay among patients discharged from the emergency department—using an accelerated failure time model. PLoS One 12: e0165756.
- Mailani F, Simandalahi T, Sari AP (2025) Analysis of factors influencing length of stay in the emergency department in public hospital, Padang, Indonesia. Med J Armed Forces India 81: 52-57.
- Alnahari A, A’aqoulah A (2024) Influence of demographic factors on prolonged length of stay in an emergency department. PLoS One 19: e0298598.
- Zaboli R, Bahadori M, Jafari H, Mousavi SM, Bahariniya S, et al. (2023) A study of factors affecting the length of hospital stay (LOS) of COVID-19 patients: A qualitative evidence in Iranian hospital. J Educ Health Promot 12: 403.
- Corrà U, Giordano A, Gnemmi M, Gambarin FI, Marcassa C, et al. (2022) Cardiovascular disease patients and predictors of length of stay of residential of cardiac rehabilitation. A specific rehabilitation is mandatory in very old patients? Monaldi Arch Chest Dis 92.
- Zhang XM, Wu XJ, Cao J, Guo N, Bo HX, et al. (2022) Investigating factors affecting the length of patients’ stay in hospitals. Journal of Integrative Nursing and Palliative Care 3: 26-30.
- Sariyer G, Ataman MG, Kiziloglu I (2020) Factors affecting length of stay in the emergency department: a research from an operational viewpoint. International Journal of Healthcare Management 13: 173182.
- Li C, Zhang Z, Ren Y, Nie H, Lei Y, et al. (2021) Machine learning based early mortality prediction in the emergency department. Int J Med Inform 155: 104570.
- Rajkomar A, Oren E, Chen K, Dai AM, Hajaj N, et al. (2018) Scalable and accurate deep learning with electronic health records. NPJ Digit Med 1: 18.
- Bashir S, Khan ZS, Khan FH, Anjum A, Bashir K (2019) Improving heart disease prediction using feature selection approaches. Proceedings of the 2019 16th International Bhurban Conference on Applied Sciences and Technology (IBCAST), January 2019, Islamabad, Pakistan, 619623.
- Aleem A, Prateek G, Kumar N, Woungang I, Dhurandher SK, et al. (2022) Improving heart disease prediction using feature selection through genetic algorithm. Advanced Network Technologies and Intelligent Computing ANTIC, 2021, Springer, Berlin, Germany, 765776.
- Lee H, Kim S, Moon HW, Lee HY, Kim K, et al. (2024) Hospital length of stay prediction for planned admissions using observational medical outcomes partnership common data model: retrospective study. J Med Internet Res 26: e59260.
- Jaotombo F, Pauly V, Fond G, Orleans V, Auquier P, et al. (2023) Machine-Learning Prediction for Hospital Length of Stay Using a French Medico-Administrative Database. J Mark Access Health Policy 11: 2149318.
- Afetor M, Harris E, Der JB, Narh CT (2023) Using routine healthcare data to determine the factors associated with hospital length of stay for hypertensive inpatients in Ghana, 2012-2017. BMJ Open 13: e066457.
- Hachesu PR, Ahmadi M, Alizadeh S, Sadoughi F (2013) Use of data mining techniques to determine and predict length of stay of cardiac patients. Healthc Inform Res 19: 121-129.
- Almashrafi A, Elmontsri M, Aylin P (2016) Systematic review of factors influencing length of stay in ICU after adult cardiac surgery. BMC Health Serv Res 16: 318.
- Mitani H, Funakubo M, Sato N, Murayama H, Rached R, et al. (2020) In-hospital resource utilization, worsening heart failure, and factors associated with length of hospital stay in patients with hospitalized heart failure: A Japanese database cohort study. J Cardiol 76: 342349.
- Tirfe M, Nedi T, Mekonnen D, Berha AB (2020) Treatment outcome and its predictors among patients of acute heart failure at a tertiary care hospital in Ethiopia: a prospective observational study. BMC Cardiovasc Disord 20: 16.
- Moriyama H, Kohno T, Kohsaka S, Shiraishi Y, Fukuoka R, et al. (2019) Length of hospital stay and its impact on subsequent early readmission in patients with acute heart failure: a report from the WETHF Registry. Heart Vessels 34: 1777-1788.
- Sarfo P, Keney G, Achampong EK (2017) A Retrospective Study of the Average Length of Hospital Stay of Patients on the Medical Wards in the Cape Coast Teaching Hospital. International Journal of Business Innovation and Technology 4: 1-13.
- Géron A (2022) Hands-on machine learning with Scikit-Learn, Keras, and TensorFlow. “O’Reilly Media, Inc.”.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.