Post-Operative Incisional Hernias Associated with Conditions that Requires Tissue Procedures
by Daniel Ioan Mihalache1*, Niculae Iordache2,3
1Department of General Surgery, Dr. Constantin Andreoiu County Emergency Hospital, Ploiesti, Romania
2Carol Davila University of Medicine and Pharmacy, Strada Dionisie Lupu 37, 020021, Bucharest, Romania
3Department of General Surgery, St. Ioan Emergency Clinical Hospital, Vitan Barzesti 13 Street, 042122, Bucharest, Romania
*Corresponding author: Daniel Ioan Mihalache, Department of General Surgery, Dr. Constantin Andreoiu County Emergency Hospital, Ploiesti, Romania.
Received Date: 18 April 2025
Accepted Date: 25 April 2025
Published Date: 14 May 2025
Citation: Mihalache DI, Iordache N (2025) Post-Operative Incisional Hernias Associated with Conditions that Requires Tissue Procedures. J Surg 10: 11313 https://doi.org/10.29011/2575-9760.011313
Abstract
Background: In the case of repairing the abdominal wall without the prosthesis material, the pathological conditions that require tissue closure have been identified. This study aims to present practical recommendations regarding abdominal wall repair without using prosthetic material, for special cases.
Material and method: The retrospective study carried out concerned the repair situations of the abdominal wall by tissue procedures in 384 patients out of a total of 1130 interventions of this kind, in a general surgery section of the Dr. Constantin Andreoiu County Emergency Hospital, Ploiesti, Romania, during January 2018 - December 2022. Patients who underwent tissue procedures to repair the abdominal wall after incisional hernias presented pathological conditions that claimed the non-use of allografts. From the set of pathological conditions identified in the 384 cases, the following was found: strangulation of the intestinal loop with borderline loop or perforation, peritonitis, acute lithic cholecystitis, entero-mesenteric infarction, neoplasms (peritoneal carcinoma, tumor occlusions, etc.), digestive hemorrhages that required intervention on the digestive tract, small-diameter eventration associated with important comorbidities such as heart failure, diabetes, liver cirrhosis, obesity, hypertension. These pathological conditions were identified singly or in different combinations. The surgical technique used in the given conditions varied depending on the case. In this sense, chelotomies, viscerolysis, partial or extensive resections, with or without anastomosis, tumorectomies, clean-up of septic foci, etc. were performed. In certain cases, it was necessary to perform gastrotomies and hemostasis in situ. The approach to parietal restoration was made taking into account the modern general principles: separation of components, reduction of parietal tension through relaxation incisions, extirpation of granulomas, careful hemostasis, restoration of the white line as much as possible in the case of median IH. Guarantee good muscle relaxation by the anesthetist team. The suture is made in anatomical planes, with separate, non-absorbable threads. In most cases, peritoneal drainage and sometimes supra-aponeurotic drainage were used.
Results: From the studied group of 1130 HIs, 384 cases representing 33.98% were identified and were solved by tissue procedures, without prosthesis. The ratio of men: to women was on average 1:4 and from the perspective of age, the average age of men was 68 years while the average age of women was 65 years. From the set of pathological conditions, type (I) strangulation of the intestinal loop with the borderline or perforated loop represented 11.36% (128 patients), respectively type (II) peritonitis, represented 5.2% (59 patients) ), the other pathologies having an average value of 2.27%. The average length of hospitalization was 12 days. Post-operative monitoring was carried out in 1 month and 6 months, considering that the operations occurred in an emergency hospital. A case study of a 74-year-old patient followed oncologically, with metachronic neoplasm of the splenic angle of the colon and post-operative pan gastric eventration, returned after 5 years, was presented. After performing a complex intervention including viscerolysis, left hemicolectomy, splenectomy, corporeal-caudal pancreatectomy, colo - colo - Termino - Terminal anastomosis, the components were separated, relaxation incisions, and restoration of the white line. 6 months after the last hospitalization, the patient did not present a recurrence of the eventration.
Conclusions: In some situations, abdominal surgical conditions do not allow the per primum prosthesis of the abdominal wall. Pathological conditions that occur in IH that require the use of tissue procedures to repair the abdominal wall were also mentioned.
The surgical techniques used included a combination of the principles of separating the components, restoring the white line in the case of median HI, ensuring a parietal tension close to the physiological one through myofascial relaxation incisions, ensuring good muscle relaxation through adequate anesthesia, closing the abdominal wall, the intermittent use of an elastic belt for a maximum period of 45 days after the operation.
Keywords: Abdominal wall without prosthesis; Combined procedures; Incisional hernia; Pathological conditions; Tissue procedures
Abbreviations: IH: Incisional Hernia; CS: Component Separation
Introduction
Incisional hernia is a frequent complication after abdominal surgery [1], Modern surgical treatment involves the use of prosthetic materials in most cases. Based on various studies and meta-analyses carried out in different periods [2-5] it was observed that the incidence of incisional hernias manifests itself more intensively in the first two years after the intervention, the recurrence being 9.8% at 21 months, respectively 12.8% at 24 months, but it can also occur after this interval. In addition, the detailed evaluation of the causes highlighted the fact that there is a triad of main categories that contribute to the increase of the risk of incisional hernias: the surgical method for both opening and closing, the clinical situation of the preoperative patient, the surgeon through personal expertise [6,7].
The development of remarkable surgical techniques such as laparoscopy, and robotic surgery together with various medical devices (allografts, polymeric surgical thread) have as their cumulative goal the performance of a surgical act to prevent the occurrence of incisional hernias, respectively to allow the repair of IH when they occur [8,9]. The development of these techniques is guided by concepts such as reducing post-operative pain, improving the quality of life [10], rapid socio-professional reinsertion, minimally invasive repairs [11], restoring some resistance structures of the abdominal wall [12,13] using some techniques minimally invasive (laparoscopy, robotic surgery). The introduction of allografts as a mechanical support in abdominal parietal defectology has reduced the recurrences in HI, developing guidelines for restoring the defective abdominal wall [14]. However, there are cases in which the use of allograft is not indicated, the conditions for which surgical intervention was performed, claiming the restoration of the wall without being prosthetic. In this study, the pathological conditions that call for repair of the abdominal wall without prosthesis are indicated, together with the surgical techniques used to reduce recurrence and improve the quality of life. A case study with complications treated using tissue repair of the abdominal wall is mentioned.
Materials and Methods
The present study is based on a retrospective of the 5-year activity of the surgery service within the Dr. C. Andreoiu County Emergency Hospital, Ploiești. From January 2018 to December 2022, 1130 abdominal wall (IH) repair procedures were performed, of which 384 procedures were resolved with tissue intervention. The decision to use tissue procedures was based on the experience of the surgical team, based on inclusion criteria.
Inclusion Criteria
Decisions to repair the abdominal wall by tissue procedures were based on the set of pathological conditions that were identified singly or in different ways of simultaneous combination:
- Intestinal loop strangulation with border loop or perforation.
- Peritonitis
- Acute lithiasis cholecystitis
- Entero mesenteric infarction
- Neoplasms (peritoneal carcinomatous, tumor occlusions, etc.)
- Digestive hemorrhages that required intervention on the digestive tract.
Small-diameter herniation and important comorbidities: heart failure, diabetes, liver cirrhosis, obesity, hypertension. The percentage distribution of these pathological conditions is graphically represented in Figure 1.
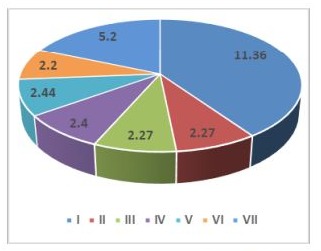
Figure 1: Graphical representation of weights for pathological conditions requiring repair by tissue closure.
The presence of comorbidities such as grade III obesity, CI Cr, HTN generate problems regarding prosthetic closure.
Surgical Technique
Under the given conditions, chelotomies, viscerolysis, partial or extensive resections, with or without anastomosis, tumorectomies, clean-up of septic foci, etc., were performed. In certain cases, it was necessary to perform gastrotomies and hemostasis in situ. The approach to parietal restoration was made taking into account the modern general principles: separation of components, reduction of parietal tension through relaxation incisions, extirpation of granulomas, careful hemostasis, restoration of the white line as much as possible in the case of median HI. The suture is made in anatomical planes, with separate, non-absorbable threads. In most cases, peritoneal drainage and sometimes supra-aponeurotic drainage were used.
Statistical Analysis
Data analysis was performed using the MINITAB version 18 statistical analysis program. Continuous variables were presented as means with standard deviations, and categorical variables were presented as numbers.
Result
In this study, based on inclusion criteria, 384 cases representing 33.98% of the study group of 1,130 IH were identified and resolved by non-prosthetic tissue procedures. The distribution of patients by gender in terms of pathologies listed in the inclusion rules is graphically depicted in Figure 2.
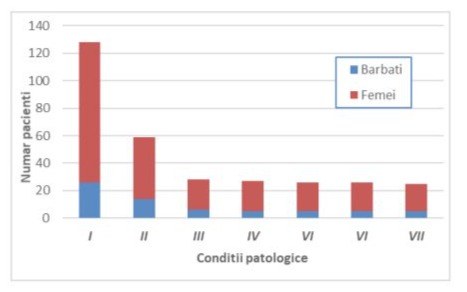
Figure 2: Distribution of the number of patients by gender according to the identified pathological conditions.
Types of Pathologies
Following the review of the case studies encountered, some typical cases for the activity of a surgery department in an emergency hospital were selected and presented for exemplification in Table 1.
|
Case examples |
Description IH |
|
Recurrent ovarian neoplasm, bilateral ureterohydronephrosis |
multisaccular, with incarceration of the great omentum |
|
Liver cirrhosis, ascites, splenomegaly with hypersplenism, Mallory-Weiss syndrome, acute gastroduodenitis |
multisaccular, with incarceration of the great omentum |
|
Small diameter IH (3 cm) |
incarceration of the great omentum |
|
Loop strangulation, occlusion, covered perforation |
|
|
Strangulation of iliac loop, left iliac fossa |
|
|
Ideal loop choke |
|
|
Side pinching of the loop, occlusion. Erysipelas in treatment |
|
|
Intestinal loop incarceration. Bowel obstruction. Large and bulky hydroelectrolytic imbalances |
|
|
Entero-mesenteric infarction |
|
|
Colecistită acută litiazică. |
incarceration of the great omentum |
|
Voluminous tumor with a genital starting point, with invasion of the urinary bladder, transverse mesocolon and pulmonary ventilation disorders |
Table 1: Examples of cases of incisional hernias solved by tissue procedures.
Duration of Surgery
From the analysis of the records regarding the duration of the surgical operations for the resolution of the cases, the average value of the operation time was 66 minutes. Because the surgical complexity associated with abdominal wall reconstruction varies, operative times ranking is not relevant for parietal reconstruction techniques evaluation.
Duration of Hospitalization
The average duration of hospitalization was 12.2 days ± 4.7 days, mentioning that this depended mostly on the basic or main condition.
Discussion
In reconstructive surgery, complex abdominal defects represent a challenge in the case of the association of intra-abdominal pathologies (oncological, traumatic, and infectious) [15]. When repairing incisional hernias in these complicated cases requiring tissue intervention, recurrence rates range from 23 to 50%, with each subsequent failure of repair increasing complication and recurrence rates [16]. In a meta-analysis including more than 14,000 patients, a weighted incidence of 12.8% IH was reported 2 years after a midline incision, it was shown that one-third of patients with IH undergo surgical repair [4]. In the case of parietal defects, regardless of their size, the expansion of knowledge of anatomy, biomechanics, and anatomy-pathology as well as advanced clinical experience [15,17], have led to an enhancement in surgical techniques, developing new approaches. One of the considerable improvements in abdominal wall repair surgery is the technique of separating the CS components. This CS technique allows the approach based on modern principles of abdominal wall reconstruction, with an impact on the primary closure of the defects and the restoration of the white line under physiological tension [18]. Following a literature study on changes in the abdominal wall after CS, Daes, and team [19] reached the following conclusions regarding CS techniques:
(a) after the anterior CS, the external oblique muscle is significantly laterally displaced; after posterior CS, the transversus abdominis undergoes minor displacement, both techniques generally do not affect muscle trophism. These findings are consistent for both open and minimally invasive CS.
(b) Abdominal wall muscle anatomy and physiology is preserved mainly by muscle overlap function and their ability to exhibit compensatory trophism after midline restoration (reloading).
(c) Well-performed CS techniques have a low risk of producing convex and lunate line hernias.
(d) Anterior and posterior CS techniques likely have different mechanisms of action.
(e) Studies of how nutrition coupled with postoperative conditioning may alter changes in the abdominal wall after CS are ongoing.
In Majumder's [20] clinical anatomy and physiology of the abdominal wall, more in-depth clinical findings and their implications for hernia repair and linea alba restoration are presented, among others. The white line is the formation resulting from the fusion, in the median plane, of the aponeuroses of the lateral muscle groups. Due to the three-layered architecture of the aponeurotic fiber tracts and courses, they form the basis for the direction-dependent elastic properties (anisotropy) and for the functional integrity and compliance of the abdominal wall [21]. In the paper [21] Hellinger and team mentioned that the principle of abdominal wall hernia surgery is based on the anatomical and functional reconstruction of the abdominal wall itself and, therefore, of the white line. When the tension is considered to be high during hernia repair, reducing the tension to physiological values can be achieved by myofascial release. A study targeting the clinical application of abdominal wall tension measurements conducted by Bilezikian et al. [22] highlighted the limited aspects of quantitative information. At the same time, it was highlighted that the concept of "tension-free" hernia repair is well understood and appreciated by surgeons. Intraoperative techniques such as myofascial release can reduce tension to physiological levels if tension is considered too high during hernia repair. Myofascial release through relaxation incisions is practiced at the level of the aponeurosis of the external oblique muscle and/or the sheath of the rectus abdominis muscles, to release the tension from the sutures at the level of the abdominal incisions [23].
In the case of large parietal defects with muscle contraction, surgeons tend to close only the integument if a prosthesis cannot be used due to certain intra-abdominal diseases or comorbidities. Over time, the size of the defect increases due to muscle contractions, difficulty breathing, and discomfort, affecting quality of life. Also, repairing the wall later is more difficult. In the cases treated and presented here, abdominal wall closure was used.
In a group of 384 patients who had abdominal wall repair performed by tissue surgery, the average male-to-female ratio was 1:4. The average age of the men was 68 years old, and the average age of the women was 68 years old.
In the analysis carried out regarding the restoration of the abdominal wall through tissue procedures, for the group of 384 patients, a set of pathological conditions was identified. These pathologies were present either singly or in different ways of simultaneous combination. All these pathologies corroborated with important comorbidities such as heart failure, diabetes, liver cirrhosis, obesity, and arterial hypertension, imposed the approach of repair in the absence of a prosthetic material (allograft). It is worth noting that from the set of pathological conditions, type (I) intestinal loop strangulation with borderline or perforated loop represented 11.36% (128 patients), respectively type (II) peritonitis, represented 5, 2% (59 patients). For the other five types of pathological conditions, types III-VII, the weighted mean value was 2.27% ± 0.089%. The percentages of patients per type of pathological condition were calculated relative to the total number of 1130 abdominal wall repair interventions, performed between January 2018 and December 2022.
The analysis of incisional hernia descriptions for case examples (see Table 1), indicates the presence of multisaccular eventrations, with incarceration of the great omentum or intestinal loop. For solving IH, combined procedures were used based on component separation, linea alba repair, and myofascial release techniques. This approach is based on the experience of a team of surgeons trained in emergency, oncologic, and parietal defect surgery. In addition, the patient's postoperative recovery period included intermittent use of an elastic belt for 30 to 45 days. An important role in the smooth running of the surgical act was the provision of good muscle relaxation on the part of the anesthetic team, to obtain the best results for the patient [24,25]. In conditions given by cases specific to an emergency hospital, the average duration of hospitalization was 12 days. Monitoring of operated patients was carried out between 1 month and 6 months.
Case Study
The case of a 74-year-old patient hospitalized with adenocarcinoma of the splenic angle of the colon, stenotic, with invasion of the tail of the pancreas, and adenopathy in the hilum of the spleen is presented as an example. The patient also had a pangastric incisional hernia (see Figure 4).
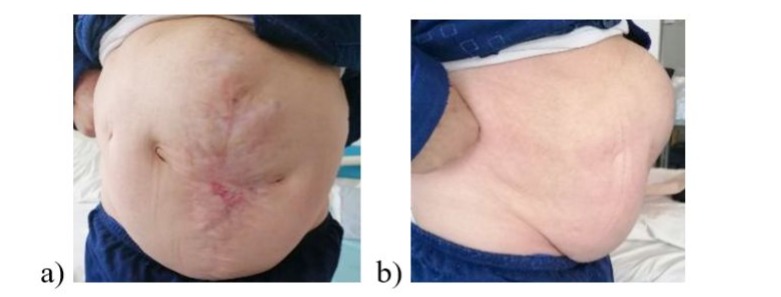
Figure 4: The preoperative appearance in orthostatism: a) frontal view, b) profile.
In the personal pathological antecedents, it is important to mention that, 5 years ago, he also presented himself in the emergency room in emergency service with a sigmoid tumor (carcinoma) with necrobiosis and neighboring phlegmon fused on the iliopsoas, at the level of the left thigh. Rectosigmoid resection with rectal end closure and terminal stg iliac colostomy, pus evacuation, and lavage were completed. This was followed by incision, evacuation, excision of necrotic tissue, debridement, and dressing of the open wound in the thigh. After healing the wound on the thigh, the patient underwent chemotherapy treatment, 7 days after the first intervention, he intervened again. 6 months after this intervention, the patient was re-hospitalized for successful reintegration.
Oncological treatment continued. After 5 years, the patient returned with a metachromic neoplasm of the splenic angle of the colon and the aforementioned pangastric eventration. Practiced: viscerolysis, left hemicolectomy, splenectomy, corporeo-caudal pancreatectomy, colo - colo - Termino - Terminala anastomosis. The analysis of the mentioned oncological situation accompanied by the complexity of the intervention led to the evaluation of the variants regarding the solution of the eventration:
a) closing only the integument: the defect would have increased over time, the discomfort and breathing difficulties would have increased
b) wall prosthesis: exclusion due to the risk of infection of the prosthesis,
c) tissue procedure: separation of components, relaxation incisions, restoration of the white line.
Option c) of surgical solution of the eventration was chosen, the patient's evolution being satisfactory. Figure 5 shows an intraoperative stage in which the tension level of the suture is checked.
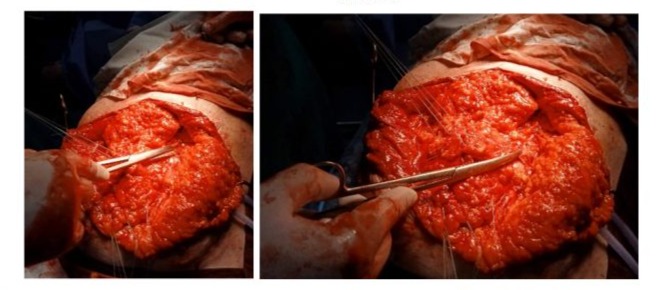
Figure 5: Intraoperative aspect: relaxation incisions where it was considered that the suture is in tension.
Complementarily, the elastic belt was used during the first two weeks after the intervention. The patient developed patchy skin necrosis 9 days after the procedure, which was excised and healed over the next 8 days.

Figure 6: Patchy integumentary necrosis and the postoperative appearance in orthostatic position.
After 6 months of the last hospitalization, the patient did not have a recurrence of the eventration. Even if it does happen, it will be smaller in dimensions, and easier to bear and repair. The patient continues the treatment with cytostatics, being in the oncological records.
Conclusions
In some situations, abdominal surgical conditions do not allow the per primum prosthesis of the abdominal wall. In an analysis from January 2018 to December 2022, out of 1130 interventions to abdominal wall repair in an emergency hospital setting, 384 interventions were solved by tissue procedures. The pathological conditions manifested singly or in different ways of combinations, which required the solution using tissue procedures to repair the abdominal wall, were identified. Among the pathological conditions included are intestinal loop strangulation, peritonitis, acute lithiasis cholecystitis, entero mesenteric infarct, neoplasms, digestive hemorrhages that require intervention on the digestive tract, small-diameter enteritis, and important comorbidities. This surgical technique was based on the combined application of the principles of component separation, repair of the linea alba at the central IH, and ensuring near-physiological parietal tension through a fascial relaxing incision. In cases of large parietal defects, abdominal wall closure was chosen. In conditions given by cases specific to an emergency hospital, the average duration of hospitalization was 12 days. Patients undergoing abdominal wall repair surgery by tissue procedures were monitored for 1 to 6 months.
A case study of a 74-year-old patient with pangastrotomy hernia in the background of stenotic adenocarcinoma of the colonosplenic angle with pancreatic tail invasion and lymphadenopathy of the splenic hilum is presented. Following the evaluation of the situation, after the necessary surgical interventions (viscerolysis, left hemicolectomy, splenectomy, corporeo-caudal pancreatectomy, colo-colo-Termino-Terminal anastomosis), the tissue procedure was chosen to repair the abdominal wall. 6 months after the last hospitalization, the patient did not present a recurrence of the eventration.
Reference
- Deerenberg BA, Henriksen NA, Antoniou GA (2022) Updated guideline for closure of abdominal wall incisions from the European and American Hernia Societies. British Journal of Surgery 109: 1239-1250.
- Shukla VK, Mongha R, Gupta N, Chauhan Puneet VS (2005) Incisional hernia—comparison of mesh repair with Cardiff repair:an university hospital experience. Hernia 9: 238-241.
- Bhaskaran A, Ambikavathy M (2013) Incisional Hernia: A Review of Etiopathogenesis, Clinical Presentation, Complications and Management. J Clin Biomed Sci 3: 1-11.
- Bosanquet DC, Ansell J, Abdelrahman T (2015) Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14 618 patients. PLoS One 10: e0138745.
- Stabilini C, Garcia-Urena M, Berrevoet F (2022) An evidence map and synthesis review with meta-analysis on the risk of incisional hernia in colorectal surgery with standard closure. Hernia 26: 411-436.
- MacDonald S, Johnson PM (2021) Wide variation in surgical techniques to repair incisional hernias: a survey of practice patterns among general surgeons. BMC Surg 21: 259-264.
- Henriksen NA, Friis-Andersen H, Jorgensen LN, Helgstrand F (2021) Open versus laparoscopic incisional hernia repair: nationwide database study. BJS Open 5: 1-8.
- Muñoz Delgado GE, Lastra Santiago MA (2023) Open abdomen: a comprehensive review, International. Surgery Journal Delgado GEM et al. Int Surg J 10: 814-817.
- Bittner R, Bain K, Bansal VK (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias. (International Endohernia Society (IEHS))—Part A. Surg Endosc 33: 3069-3139.
- Whalen A, Holla S, Renshaw S (2024) Outcomes and quality of life of frail patients following elective ventral hernia repair: Retrospective review of a national hernia collaborative. Am J Surg 15: S0002-9610(24)00099-0.
- Henriksen NA, Friis-Andersen H, Jorgensen LN, Helgstrand (2021) Open versus laparoscopic incisional hernia repair: nationwide database study. BJS Open 5: zraa010.
- Daes J, Telem D (2019) The principled approach to ventral hernia repair. Rev Colomb. Cir 34: 25-28.
- Daes J, Oma E, Jorgensen LN (2022) Changes in the abdominal wall after anterior, posterior, and combined component separation. Hernia 26: 17-27.
- Deerenberg EB, Henriksen NA, Antoniou GA (2022) Updated guideline for closure of abdominal wall incisions from the European and American Hernia Societies. Br J Surg 109: 1239-1250.
- Garcia Ureña MÁ, López-Monclús J, Hernando LAB (2024) Narbenhernien: offene Operationsverfahren und Ergebnisse einer Kohortenstudie mit 343 Patienten [Incisional hernia: open abdominal wall reconstruction. Current state of the technique and results]. Chirurgie (Heidelb) 95: 10-19.
- Holihan JL, Alawadi Z, Martindale RG (2015) Adverse events after ventral hernia repair: the vicious cycle of complications. J Am Coll Surg 221: 478-485.
- Lopez-Monclus J, Muñoz-Rodríguez J, San Miguel C (2020) Combining anterior and posterior component separation for extreme cases of abdominal wall reconstruction. Hernia 24: 369-379.
- Jensen KK, Munim K, Kjaer M, Jorgensen LN (2017) Abdominal wall reconstruction for incisional hernia optimizes truncal function and quality of life: a prospective controlled study. Ann Surg 265: 1235-1240.
- Daes J, Oma E, Jorgensen LN (2022) Changes in the abdominal wall after anterior, posterior, and combined component separation. Hernia 26: 17-27.
- Majumder A (2016) Clinical Anatomy and Physiology of the Abdominal Wall. In: Novitsky, Y. (eds) Hernia Surgery. Springer 2016: 1-13.
- Hellinger A, Roth I, Biber FC, Frenken M, Witzleb S, et al. (2016) Chirurgische Anatomie der Bauchdecke [Surgical anatomy of the abdominal wall]. Chirurg 87: 724-730.
- Bilezikian JA, Faulkner JD, Fox SS, Hooks WB, Hope WW (2019) Clinical Application of the Measurement of Abdominal Wall Tension. in Hernia Repair. Surg Technol Int 35: 129-134.
- Gavrilas F (2010) Tratamentul chirurgical. In: Gavrilas F, Oprea V, editors. Chirurgia peretelui abdominal. Hernia inghinala recidivata. Hernia incizionala.Cluj-Napoca: Editura Medicala Universitara "Iuliu Hatieganu" 2010: 221-318.
- Ledowski T (2015) Muscle Relaxation in Laparoscopic Surgery: What is the Evidence for Improved Operating Conditions and Patient Outcome? A Brief Review of the Literature. Surg Laparosc Endosc Percutan Tech 25: 281-285.
- Boon M, Martini C, Dahan A (2018) Recent advances in neuromuscular block during anesthesia. F1000Res 7: 167-175.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.