Personal Experiences of UK and US Consultant Vascular Surgeons in Gaza
by Kaji Sritharan1*, Morgan McMonagle2, Bara Zuhaili3, Shadman Baig4, Junaid Sultan5
1Consultant Vascular Surgeon, York & Scarborough Teaching Hospitals NHS Foundation Trust, York, UK
2Consultant Vascular, Trauma Surgeon & Humanitarian Surgeon, St. Mary’s Hospital & Imperial College Healthcare, London, W2 1NY, UK
3Consultant Vascular Surgeon, Center for Humanitarian Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States.
4Consultant Vascular Surgeon, Division of Vascular and Endovascular Surgery, Department of Surgery, University of Texas Southwestern Medical Center, Dallas, TX, USA
5Consultant Vascular Surgeon, Hull University Teaching Hospitals NHS Trust, Hull, UK
*Corresponding author: Kaji Sritharan, Consultant Vascular Surgeon, York & Scarborough Teaching Hospitals NHS Foundation Trust, York, UK
Received Date: 07 August 2025
Accepted Date: 13 August 2025
Published Date: 15 August 2025
Citation: Sritharan K, McMonagle M, Zuhaili B, Baig S, Sultan J, et al. (2025) Personal Experiences of UK and US Consultant Vascular Surgeons in Gaza. J Surg 10: 11412 https://doi.org/10.29011/2575-9760.011412
Background
For over 22 months, western media have been denied entry to independently report on the conflict in Gaza. International emergency medical teams therefore have a moral obligation to not only advocate for the humanitarian crisis but to also bear witness. With over now 242 journalists killed in Gaza, the testaments of healthcare workers have become increasingly more important. The authors have decades of experience between them as Consultant Vascular Surgeons in the UK NHS and USA. We have worked in Gaza intermittently since 7 October 2023 and this editorial is an account of our personal experiences and the types of injuries we have observed and treated.
Destruction of Healthcare Systems & Attacks on Civilians within Hospital Grounds
Despite article 18 of the Geneva Convention IV (1949) specifically addressing the protection of hospitals during conflict and Rule 25 of Customary International Humanitarian Law (ICRC) protecting medical personnel, all hospitals in Gaza without exception have been targeted in this war and over 1,400 healthcare professionals have been killed (Figure 1). There have also been multiple confirmed attacks by the Israeli Forces on alleged ‘suspected militants’, unarmed at the time, whilst with their families in tents within the vicinity of hospitals. One such drone attack on a tent within the boundaries of Al-Aqsa Hospital in Deir Balah, in 2024, resulted in the immediate death of 4 unknown humans, 2 children of unknown age, and 1 female in her 40s. Eight people were also seriously injured and required surgery - they were all women and children under the age of 12. This attack, one of hundreds, almost all confirmed by the Israeli Forces as successful elimination of suspected militants, make no mention of the terrible loss of civilian life.

Figure 1: Bombed out surgical wing (A) and orthopaedic and plastic surgery wings (B) of Al Shifa Hospital, Gaza.
Restriction of Humanitarian Aid into the Gaza Strip, Displacement and Death
The passage of food, essential medical equipment and medicines into Gaza has been severely restricted since the start of the war, resulting in a humanitarian crisis of unimaginable proportions. At the time of writing this article, the United Nations estimated that 100,000 Palestinian women and children were facing severe malnutrition, with a third of the 2.1 million population not having eaten in days. All the doctors and allied healthcare professionals we worked with had been displaced more than once. Most lived in tents no more than 4m x 4m in size. An ED consultant told us how he lost his wife and 4 children to an airstrike in November 2023. He was at work when his neighbours were bought to ED after their house was bombed. He rushed home to find his entire family dead. An orthopaedic doctor called Abu Malik reported to work at Naseer Hospital on 11 June 2024, one day after he buried his father, mother, wife, and 3 kids aged 12, 8 and 6 years old. This is a familiar story in Gaza. Everyone has lost someone in this war and typically multiple family members. At the time of writing, over 61,000 people had been killed in Gaza; nearly 1 in 3 were children. These figures however do not include those still buried under the rubble. Nor do they include those who have died of other conditions, which could have been treated if Israel had not prevented the entry of medications and other essential medical equipment into Gaza or destroyed healthcare infra-structure. Over 151,000 Palestinians have been injured in this conflict.
Types of Injuries Witnessed
The patient names in this editorial are made-up but their stories are very real. They lay bare the brutalities of this conflict. The necessary permissions have been sought.
Blast Injuries
Most blast injuries we witnessed were catastrophic and nonsurvivable. There were daily mass casualty scenarios which would overwhelm the ED, with patients arriving by donkey and cart, private transportation or children being carried in - scenes which could only be described as apocalyptic. Wave after wave of dead children, killed in the most violent of circumstances. We witnessed decapitated bodies of children and adults, mangled extremities, non-survivable burns, body parts and evisceration. Military grade weapons used against the most helpless, who are already starving and living in tents with little or no protection from blast (Figure 2).

Figure 2A: Mangled extremity following bombing in a marketplace in Khan Younis, Gaza. This young man underwent guillotine amputation. Figure 2B: 12 year old boy following a blast. Foley catheters have been used as tourniquets to prevent bleeding. He underwent bilateral above knee guillotine amputation. Figure 2C: Non-survivable burns in a young man after bombing of a residential
Injuries from Shrapnel
Those not killed instantly by the blast wave, suffered devastating injuries from shrapnel. Shrapnel resulted in transection of the common, external and internal carotid arteries in Bahir, a10-yearold boy, resulting in a dense hemiplegia. Mariam is a 5-year-old girl with complete left sided paralysis from a penetrating traumatic brain injury caused by shrapnel. She also required a laparotomy, splenectomy and had extensive small bowel injuries (Figure 3). Fazia is an 11-year-old girl. Her tent was hit by a drone strike. Her father was left a bilateral amputee. She suffered a lung injury and pneumothorax, as well as a grade 4 splenic injury and required splenectomy. The family of five she shared a tent with - 2 adults and their 3 children were killed. Their remains are shown in Figure 4. They had no ability to defend themselves. Ahmed is a fiveyear-old boy with devastating cardiac, lung, liver and small bowel injuries caused by shrapnel. Unfortunately, despite a clamshell thoracotomy to repair the heart and laparotomy for massive liver bleeding, he died shortly after surgery (Figure 5). Maryam is a 9 month old girl with complete right sided paralysis from shrapnel injury to her left brain. She also had shrapnel injuries to her trachea and oesophagus and has a tracheostomy (Figure 6). And so, the list goes on.

Figure 3: A 5 year old girl with complete paralysis down her left side from shrapnel penetrating traumatic brain injury to the left brain. She has also undergone a laparotomy and splenectomy and had extensive small bowel injury.

Figure 4: The remains of a family of 5 seen at the mortuary at Nasser Hospital, Khan Younis, Gaza.

Figure 5: A 5 year old boy who has undergone a clamshell thoracotomy and laparotomy due to severe shrapnel injury. He had extensive cardiac, lung, liver and small bowel injury. He died shortly after surgery.

Figure 6: A 9 month old girl with complete paralysis down her right side from shrapnel injury to left brain. She also had shrapnel injury to her trachea and oesophagus (repaired) and has a tracheostomy.
Infected Wounds
Even if shrapnel injuries do not require immediate surgical attention, shrapnel lodged within soft tissues, in the context of a lack of basic wound care supplies, poor sterile conditions and malnutrition, produces a wound care dilemma; since these patients usually present later with significant morbidity due to infection and sepsis, with delayed mortalities. A child who required debridement of his wounds caused by shrapnel told us in theatre that he was worried about the ‘worms.’ He’s wound was infested with maggots (Figure 7). He was only 10 years old. Many patients return with devastating infectious wounds from shrapnel, especially around the perineum, and often with necrotising fasciitis. Others return with giant mycotic pseudoaneurysms around a vessel, requiring repair. Jamal is a 26 year old man with a pseudoaneurysm of the aorta. He underwent aortic interposition graft repair but died days afterwards (Figure 8).

Figure 7: Soft tissue ‘peppering’ of the skin of a 10 year old boy from shrapnel. The wound from shrapnel is infested with maggots.
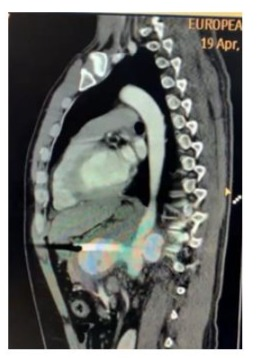
Figure 8: Pseudoaneurysm of the aorta in a 26 year old man following shrapnel injury. He underwent open repair with interposition graft but died a few days afterwards.
Sniper Injuries
Snipers typically targeted young men or children with ‘kill shots’ to the head or chest. Other shots were aimed at major blood vessels. These included the carotid, axillary, brachial, superficial femoral, popliteal arteries (Figure 9) and aorta. The most common target appeared to be the superficial femoral artery. Patients would then either exsanguinate at the scene or if they survived to hospital, would need complex repair of the nerve, vein and artery with fasciotomies. Ahmed is a 14-year-old boy who is an orphan. Whilst walking in the market he was hit by a sniper. The bullet missed his iliac vessels but resulted in 7 enterotomies of his small bowel. The entry and exit wounds of the bullet are shown in Figure 10. Mohammad gives a similar story of walking along the street with his 2 cousins. They were killed by sniper shots. His superficial femoral artery was transected (Figure 11) and he underwent interposition vein graft repair and fasciotomies. He survived.

Figure 9: 38 year old man with a sniper shot into the popliteal fossa (A), resulting in a venous, arterial and nerve injury which required surgical reconstruction. The bullet was retrieved and is shown (B).
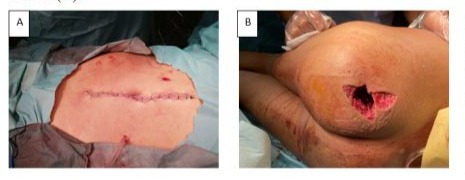
Figure 10: 14-year-old orphan with GSW from a sniper. The entry wound is seen in the RUQ (A). The exit wound is in the left buttock (B). The bullet misses his iliac vessels. He has 7 enterotomies to the small bowel.
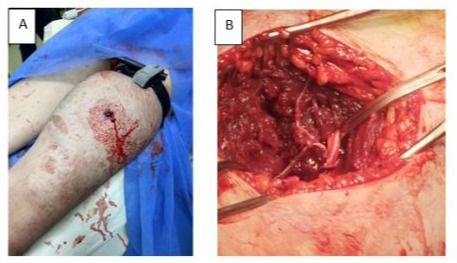
Figure 11: GSW from a sniper into the left thigh resulting in SFA transection (B). This was treated with a vein interposition graft with GSV and fasciotomies. The image demonstrates the entry wound (A).
Drone and Quadcopter Injuries
Other causes of gun shot wounds come form drones and quadcopters that constantly roam over the skies of Gaza. The buzzing hum of these drones are incessant. Malak is an 11-yearold girl. Her family were evacuating Rafah under order and were targeted by an Apache helicopter (as per ambulance personnel who transported them). Her mother suffered relatively minor injuries, but her two younger siblings (aged 4 and 5 years old) were dead on arrival. Her father had devastating injuries and died a number of hours after admission. Malak had very targeted high velocity penetrating injuries to both her legs and upper limbs with massive skeletal and soft tissue injury. We repaired her left brachial artery and externally fixed her left humerus and performed haemostasis of her lower limb wounds. She survived but is now a bilateral amputee. She is only eleven years old (Figure 12).

Figure 12: An 11 year old girl shot by an Apache helicopter with all 4 limbs affected (A). She had an open compound fracture of the left elbow (B), soft tissue and vascular injuries (C). She underwent repair of left brachial artery with an external fixation device applied to the left upper limb. She has since had both lower limbs amputated.
Child Amputees & Psychological Impact
We witnessed children with mangled limbs requiring bilateral amputations, presenting to ED with a Foley catheter used as tourniquet due to lack of medical supplies. There were hands that required amputation after blast of a bomb disguised in Tuna food cans. Many children lost up to three limbs. In Al-Aqsa hospital, in January 2024, a blast injury victim came to ED. The blast was so severe that her 14 month old infant girl had died in her arms. The nature of the blast resulted in the infant ‘melting’ onto her mother’s elbow causing significant damage to the mother’s right arm. The only way to extract the body of the infant was to perform an above elbow amputation. The infant was subsequently buried together with her mother’s amputated arm. More than 1 in 5 (23%) of all amputates are children. Children also account for 26% of all spinal cord injuries, 33% of all traumatic brain injuries and 70% of burns cases in Gaza. Yet, there are no paediatric rehabilitation services in Gaza. Overall, nearly 30,000 trauma cases in Gaza require rehabilitation services. There are currently only 84 adult rehabilitation beds.
Despite many of the children with amputations surviving, there are very few to be seen on the streets or marketplace. One can only conclude, that due to the lack of resources for rehabilitation and mobility, they are now confined to whatever home space their parents have managed to scratch out from the rubble. Other more able-bodied children are seen outside gathering fuel, food and water to bring ‘home’.
Chronic Diseases
Since the start of this war 22 months ago, Israel has restricted the entry of medications required to manage chronic conditions, such as diabetes, renal failure and heart disease. This has undoubtedly led to avoidable deaths and morbidity.
Renal Access
Nearly half (41%) of patients requiring haemodialysis have died. The ‘new’ dialysis building at Nasser Hospital was destroyed by the Israeli Forces who had occupied it as a living space during the siege on the hospital in February and March 2024; it was set on fire when they abandoned it. We witnessed fistulas thrombose due to severe dehydration, lack of medications and trauma related injuries. Due to limited access to theatre due to the sheer volume of trauma-related emergency cases, new fistulas for access were not often created. Given this, the number of central lines for emergency dialysis increased exponentially with their inherent problems of infection and central vein stenosis. The lack of endovascular facilities and equipment meant the latter could not be treated resulting in inadequate or no access for haemodialysis. Even if patients did have access for haemodialysis, the destruction of dialysis facilities or roadblocks, bombing and sniper fire making travel impossible, meant these patients would die, with no palliative support. Moreover, since 7 Oct 2023, no immunotherapy medications have been allowed into Gaza. Consequently, patients with kidney transplants have also been left to die slow and painful deaths from uraemia.
Chronic Limb Threatening Ischaemia & Diabetic Foot Sepsis
Vascular reconstruction, either open or endovascular, is not an option for patients with CLTI in Gaza. We performed major amputations in patients with vascular disease in whom if it were not for the war, their limbs could have been salvaged. There were numerous cases of dry gangrene that progressed to necrotising fasciitis, cellulitis or wet gangrene (see Figure 13) necessitating major amputations. These patients often had poor diabetic control due to a lack of medications and typically presented late to ED as primary healthcare no longer exists in any meaningful way in Gaza. Other neglected surgical disease seen coming to the hospital regularly included obstructing cancers.

Figure 13: Neglected diabetic foot with extensive gangrene.
The Cruel Reality in Gaza
When we reflect on our time in Gaza, it is difficult to see how we could have made any tangible difference. The cruelty levelled at a vulnerable population, trapped inside a space roughly the same size of Manhattan, where 50% of the population is under 18 years old is horrifying. They are starving and under continuous military-grade bombardment, hospitals have run out of equipment and medications, and the workforce is exhausted. Moreover, the terrible and haunting reality is that many of those that we did ‘save’ will likely now be dead.
What next for Gaza?
This is a political problem, that can only be solved with a political solution. We call for a permanent ceasefire, an immediate meaningful increase in the number of supplies (food, fuel and medicines) entering via safe humanitarian corridors and the restoration of critical infrastructure to allow food distribution in addition to allowing hospitals and desalination plants to function. This is a starving population requiring immediate food aid.
In this devastation, global media hold a critical responsibility:
to break the silence, expose the ongoing suffering and to we have borne witness to this in Gaza. Whilst we stand by our place pressure on world leaders to take actions. The medical humanitarian principles to relieve suffering where we can; this war establishments including medical journals also have their part to has driven us to also advocate for the silenced who are now the play. There are no winners in war. Only tragedy and pain, and most desperate and vulnerable.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.