Peripancreatic Collection Surrounding the Portal Vein Extending to the Gallbladder in Acute-On-Chronic Pancreatitis: A Case report of a Rare Presentation of a Common Disease
by André E1, Ksontini R.1, Piazza G1,2*
1Surgical Department, Hospital Riviera-Chablais Vaud Valais, Rennaz, Switzerland
2University of Lausanne (UNIL), Lausanne, Switzerland
Corresponding author: Piazza G, Surgical Department, Hospital Riviera-Chablais Vaud Valais, Rennaz, Switzerland
Received Date: 1 August 2024
Accepted Date: 14 August 2024
Published Date: 16 August 2024
Citation: André E, Ksontini R, Piazza G (2024) Peripancreatic Collection Surrounding the Portal Vein Extending to the Gallbladder in Acute-On-Chronic Pancreatitis: A Case report of a Rare Presentation of a Common Disease. J Dig Dis Hepatol 9: 212. https://doi.org/10.29011/2574-3511.100212
Abstract
Peripancreatic collections are common complications of acute pancreatitis and generally, they are located around the pancreas. Their occurrence in extra-pancreatic locations is rare. We report the case of a 68-year-old female that was admitted with an acute-on-chronic pancreatitis that developed a peripancreatic collection ascending along the portal vein and extending around the gallbladder. Initial diagnosis was suggested by MRI imaging and a percutaneous drainage confirmed the diagnosis. The patient recovered well postprocedure, with a 12-month follow-up showing no signs of recurrence.
This case highlights a rare extra-pancreatic presentation of peripancreatic collections in pancreatitis, emphasizing the importance of imaging in diagnosis and the efficacy of percutaneous drainage in management.
Keywords: Pancreatic fluid collection; Drainage; Acute-onchronic pancreatitis
Introduction
Peripancreatic collections are a common complication following acute pancreatitis. According to the Atlanta criteria, these collections are classified as pseudocysts if they persist for more than four weeks [1]. They typically arise after an episode of acute pancreatitis due to a leakage from the pancreatic duct, allowing digestive enzymes to accumulate in surrounding tissues [2].
The prevalence of peripancreatic collections varies with the severity of the pancreatitis and the population studied. These collections are more commonly associated with alcoholic pancreatitis rather than biliary pancreatitis with an incidence approximatively of 2130% vs. 8-18% respectively [3-5].
In general, complications occur more frequently in cases of chronic pancreatitis. This increased prevalence is attributed to the recurrent and persistent nature of pancreatic inflammation, which promotes the development of fluid collection and pseudocyst. Kim and al [6] reported that pancreatic pseudocyst develop in 14% of acute pancreatitis cases compared to 42% of acute-on-chronic pancreatitis.
While these complications, particularly peripancreatic collections, typically occur in close proximity to the pancreas, they can occasionally develop in more distant structures, such as the mediastinum [7,8], pelvis [9] and perihepatic spaces [10-13].
The case study presents a 68-year-old female with a history of alcoholic chronic pancreatitis who experienced an acute episode characterized by a collection ascending along the portal vein and extending around the gallbladder.
According to recent reviews of literature, the case of this 68-yearold patient was selected for its atypical and unique presentation.
Case presentation
A 68-year-old woman known for alcohol-related chronic pancreatitis, with a history of wall of necrosis (WON) which had been drained Endoscopically twice three years earlier, presented to the emergency department complaining of abdominal pain persisting for several days.
The patient was hemodynamically stable and presented a soft, depressible abdomen with tenderness to epigastric palpation with no sign of peritonism. Biological workup carried out in the emergency department confirmed a recurrence of pancreatitis with a lipase elevation of 1607 U/l and a CRP of 21 without leukocytosis or disturbance of liver function tests.
An abdominal CT scan shows an area of necrosis at the corporocephalic junction with a single collection in contact with the pancreas’ tail as well as a suspicion of incipient cholecystitis. An ultrasound revealed a single 3 mm lithiasis with signs of acute cholecystitis, associated with the appearance of multiple fluid collections in the vesicular bed.
In this case, conservative treatment with antibiotic is started.
Following a lack of improvement and the persistent inflammatory syndrome and the emergence of cholestasis, an abdominal CT scan was repeated, showing persistent signs of pancreatitis and increased fluid collections around the gallbladder, extending along the hepatic hilum and around the portal vein to the pancreas. These findings suggested the presence of an abscess or an increase of the already known peripancreatic collection. For this reason, we decided to perform a cholangio-IRM to clarify the diagnosis. The cholangio-IRM suggested the presence of peri-pancreatic collection according to the Atlanta criteria (Figure 1 and 2).
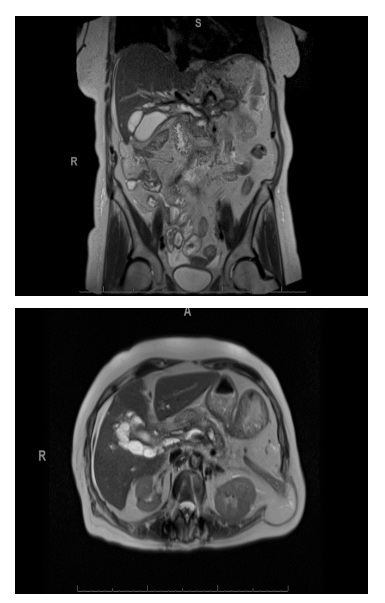
Figure 1 and 2: T2-weighted MRI of the abdomen in coronal and transverse sections showing acute fluid collections distributed in the anterior and posterior peripancreatic regions, extending around the gallbladder and the portal vein.
In the light of this atypical situation, radiological drainage was carried out and a lipase test on the fluid confirmed the diagnosis. Subsequently, with a good clinical-biological improvement, the patient was discharged after 6 days post-drainage without any drain, which was removed on the day of discharge. The patient did not develop any recurrence after 12 months of follow-up.
Discussion
The occurrence of extra-pancreatic collections is uncommon and can lead to potential diagnostic delays. These collections can migrate to various locations, including the mediastinum and hepatic regions [8,11,12]. The etiology of such migrations is not well understood, but possible mechanisms include anatomical proximity allowing the collection to erode adjacent structures, the ability to fistulize into other structures [14], and the presence of preexisting anatomical spaces that facilitate migration, such as the esophageal hiatus for mediastinal involvement [12]. Hepatic propagation may occur along gastrohepatic ligament into the liver or through the hepatoduodenal ligament [10,15], potentially leading to complications due to compression. Since the 1970s, there have been only about sixty reported cases of intrahepatic collections or pseudocysts, with a higher frequency in the left lobe of the liver [12,13].
Our patient presents a unique case of a collection following acute-on-chronic pancreatitis that extends from the pancreas to the region around the gallbladder, ascending along the portal vein. This specific presentation has not been documented in the literature before. The location of the collection leads to significant challenges, particularly concerning the compression of adjacent structures. In terms of diagnostic modalities, both CT and MRI were instrumental in guiding the diagnosis. The absence of diffusion restriction on imaging suggested a pseudocyst rather than an abscess. The definitive diagnosis was confirmed through fluid analysis, providing a conclusive result.
Most peripancreatic collection, approximately 70%, resolve spontaneously and do not necessitate specific treatment. Following pseudocyst formation, spontaneous resolution is 25-40%, depending on the study [5,16]. Intervention is warranted when there is a mass effect on adjacent structures, when patients are symptomatic, or in the presence of complications such as infection, hemorrhage, or rupture [17].
In our case, an extra-pancreatic collection in the periportal region was associated with biliary duct dilatation and early cholestasis, presenting in a symptomatic patient. Various therapeutic approaches have been delineated in the literature for managing these extrapancreatic locations, including surgical drainage, endoscopic ultrasound-guided (EUS) drainage, and percutaneous drainage. No stringent and definitive guidelines have been established for the management of pseudocysts and collections [18,19].
Based on findings in the literature regarding intrahepatic pseudocysts, percutaneous drainage was proposed as treatment option. The patient experienced a positive outcome, with no recurrence observed during the 12-month follow-up period.
Conclusion
In conclusion, this case underscores a rare complication of a commonly encountered medical condition. These observations expand the differential diagnosis, leading to enhanced patient management. Percutaneous drainage can be an effective firstline, minimally invasive treatment for peripancreatic collections, offering both diagnostic and therapeutic benefits while being welltolerated by patients.
References
- Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, et al. (2013) Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 62: 102‑111.
- Habashi S, Draganov PV (2009) Pancreatic pseudocyst. World J Gastroenterol 15: 38‑47.
- Cho JH, Kim TN, Kim SB (2015) Comparison of clinical course and outcome of acute pancreatitis according to the two main etiologies: alcohol and gallstone. BMC Gastroenterol 15: 87.
- Maringhini A, Uomo G, Patti R, Rabitti P, Termini A, et al. (1999) Pseudocysts in Acute Nonalcoholic Pancreatitis (Incidence and Natural History). Dig Dis Sci 44:1669‑1673.
- Cui ML, Kim KH, Kim HG, Han J, Kim H, et al. (2014) Incidence, Risk Factors and Clinical Course of Pancreatic Fluid Collections in Acute Pancreatitis. Dig Dis Sci 59: 1055‑1062.
- Kim KO, Kim TN (2012) Acute Pancreatic Pseudocyst: Incidence, Risk Factors, and Clinical Outcomes. Pancreas 41: 577.
- Dryazhenkov GI, Dryazhenkov IG, Balnykov SI, Kalashyan EV, Stepankov AA (2022) Mediastinal pancreatobiliary pseudocysts. Khirurgiia (Mosk) 3: 56‑63.
- Parihar PH, Gulve SS (2021) Mediastinal Extension of Pancreatic Pseudocyst – A Case Report. J Evol Med Dent Sci 10 :316‑318.
- Oshima N, Wada M, Takahashi H, Tamura R, Hosotani R, et al. (2010) Huge Pancreatic Pseudocyst Presenting With a Specific Morphology, Which Expanded to the Pelvic Space: A Case Report. Pancreas. 39: 700.
- Hamm B, Franzen N (2008) Atypisch lokalisierte Pankreaspseudozysten in Leber, Milz, Magenwand und Mediastinum: CT‑Diagnostik. RöFo ‑ Fortschritte Auf Dem Geb Röntgenstrahlen Bildgeb Verfahr. 159: 522‑527.
- Siegelman SS, Copeland BE, Saba GP, Cameron JL, Sanders RC, et al. (1980) CT of fluid collection sassociated with pancreatitis. AJR Am J Roentgenol 134: 1121‑1232.
- Demeusy A, Hosseini M, Sill AM, Cunningham SC (2016) Intrahepatic pancreatic pseudocyst: A review of the world literature. World J Hepatol 8: 1576‑1583.
- Nadia N, Moideen Sheriff S, Fewajesuyan A, Emmanuel S, Nguty Nkeng E, et al. (2023) An Infected Intrahepatic Pancreatic Pseudocyst and Calcified Pancreas: A Rare Complication of Chronic Pancreatitis. Cureus 15: e35384.
- Eccles J, Wiebe E, D’Souza P, Sandha G (2019) Pancreatic pseudocyst‑portal vein fistula with refractory hepatic pseudocyst: Two cases treated with EUS cyst‑gastrostomy and review of the literature. Endosc Int Open 7: E83‑E86.
- Al‑Ani R, Ramadan K, Abu‑Zidan FM (2009) Intrahepatic pancreatic pseudocyst. N Z Med J 122: 75‑77.
- Cheruvu CVN, Clarke MG, Prentice M, Eyre‑Brook IA (2003) Conservative treatment as an option in the management of pancreatic pseudocyst. Ann R Coll Surg Engl 85:313‑316.
- Dumonceau JM, Delhaye M, Tringali A, Dominguez‑Munoz JE, Poley JW, et al (2012) Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 44: 784‑800.
- Gurusamy KS, Pallari E, Hawkins N, Pereira SP, Davidson BR (2016) Management strategies for pancreatic pseudocysts 4: CD011392.
- Teoh AYB, Dhir V, Jin ZD, Kida M, Seo DW, et al. (2016) Systematic review comparing endoscopic, percutaneous and surgical pancreatic pseudocyst drainage. World J Gastrointest Endosc 8: 310‑318.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.