Periareolar Lifting and Glandular-Duplication After Implant Removal and Total Intact Capsulectomy in Patients with Prior Breast Augmentation
by Christina Irene Günter*
Clinic for Plastic Surgery and Hand Surgery, Klinikum rechts der Isar, Technical University Munich Ismaninger Str. 22, 81675 Munich, Germany
*Corresponding author: Christina Irene Günter, Clinic for Plastic Surgery and Hand Surgery, Klinikum rechts der Isar, Technical University Munich Ismaninger Str. 22, 81675 Munich, Germany
Received Date: 16 September 2025
Accepted Date: 22 September 2025
Published Date: 25 September 2025
Citation: Günter CI (2025) Periareolar Lifting and Glandular-Duplication After Implant Removal and Total Intact Capsulectomy in Patients with Prior Breast Augmentation J Surg 10: 11451 https://doi.org/10.29011/2575-9760.011451
Abstract
Breast implant removal without replacement becomes increasingly popular, due to growing concern about breast implant-associated complications, such as Breast Implant Illness and Large Cell Lymphoma (BIA-ALCL). Breast implant removal without replacement leaves an empty and stretched skin/tissue envelope. The challenge is to maintain breast aesthetics following implant removal. A disadvantage of most surgical techniques are obvious and well visible scars. We present the periareolar lifting and glandular duplication after total intact capsulectomy and implant removal as a safe and reliable alternative causing minimal scarring. We present 102 patients between 09.2020 and 12.2024 on whom the procedure was performed and who gave informed consent to scientific publishing.
Complications: 1 post-operative bleeding, 1 infection, 6 seromata, 4 scar treatments. There was no postoperative ptosis, majority of patients were satisfied with the outcome. There is no defined treatment approach for patients who want a total complete removal of breast implants. Since there are no clear guidelines basic principles of breast revision surgery can be applied. Attempts to minimize scarring have resulted in techniques that produce a vertical scar. These vertical scars are often not acceptable to many patients, due to visibility. Periareolar lifting and glandular duplication yields safe surgical technique and yields safe and aesthetic results with reduced scarring and high patient satisfaction.
Results of this report provide a starting point for further high-quality investigations.
Keywords: BIA-ALCL; Breast Augmentation; Breast Implant Removal; Glandular Duplication; Periareolar Lifting; Total Intact Capsulectomy
Introduction
Breast augmentation will remain one of the most popular cosmetic procedures, with more than 1.6 million procedures worldwide in 2022. 80% of breast augmentation procedures are for aesthetic augmentation, with the remaining 20% used for reconstructive procedures (tumor reconstruction, post-trauma, congenital malformations) [1,2] implant removal and total capsulectomy ASPS 1). This trend reflects growing public concern about breast implant-associated complications such as BIA-ALCL and other diseases and complications associated with breast implants, as well as changes in fashion brought about by beauty and beauty trends [3-5]. As a result, there is a growing number of patients, both reconstructive and cosmetic, who are for breast implant removal, often with a specific request for “en bloc” or total intact capsulectomy [6,7]. In both populations, the main concerns are the safe and complete removal of the capsule and implant and the aesthetic outcome in terms of the shape and appearance of the breast after implant removal. Breast implant removal without replacement leaves an empty and stretched skin/tissue envelope. The size of this will depend on a number of factors including: the size of the implants, the time since the first operation and the position of the implant pocket. Lifestyle, weight or hormonal and pregnancy-related changes in the breast during this time can also affect the size of the breast, the quality of the skin of the breast, the quality of the skin and the position of the nipple.
It is therefore not surprising that these breasts are often ptotic and often require mastopexy after explantation. Routinely available mastopexy procedures are challenging in these cases, and the resulting skin and tissue resections can further compromise breast size [8]. For the cosmetic patient presenting for explantation, the main challenge is to maintain breast aesthetics following implant removal with or without total (intact) capsulectomy. The immediate expansion of the overlying tissue due to implant insertion is followed by tissue thinning and subsequent weight and volume loss. In addition, the associated forces stretch the breast skin/tissue envelope. The stretching effects depend on individual predisposition, time, weight, breast volume in relation to the implant and the position of the breast implant pocket. This applies to sub pectoral, double plane and sub glandular implant placements. For implants of the same size and over the same period of time, tissue stretching is seen more in the sub glandular pocket than in the submuscular pocket, and heavier implants cause more stretching regardless of the pocket used [9,10]. In addition, implant placement above the pectoralis results in pronounced glandular atrophy [11].
In slim patients, following capsulectomy, the skin flaps often resemble nipple-sparing mastectomy flaps with restricted blood supply primarily through the subdermal plexus [12]. Previous publications have revealed possible shortcomings associated with lifting the breast following complete (intact) capsulectomy and implant removal, as well as nipple-sparing mastectomy. Davies et al. described that peri areolar incisions had less wound healing complications versus Wise and vertical patterns [13]. Santanelli and di Pompeo et al. used a double-mirrored omega pattern after skin-sparing mastectomy with reduced rates of skin necrosis versus a Wise-pattern incision [14]. Single cranially omega lift incision have been described after implant removal and total capsulectomy in prior breast augmentation with minimal complication rates [15]. The common disadvantage of all above described incisions are obvious and well visible scars. Which are often not acceptable for the patients who have a high demand regarding the aesthetic outcome. We therefor present the periareolar lifting and glandular duplication as a safe and reliable alternative with improved aesthetic outcomes due to reduced scaring and, as additional aesthetic benefit, moderate auto augmentation and shaping due to the glandular duplication.
Material and Methods
Patient Population
The described surgical procedure was performed on 102 patients who presented between 09.2020 and 12.2024 in our clinic and who opted for periareolar lifting and glandular-duplication after implant removal and total intact capsulectomy. In advance these patients gave informed consent for anonymized data evaluation for scientific purposes. For this publication a specific approval of the ethics committee was not necessary by German law.
Markings and Technique
Breast marking was performed in the standing position. Measurements of Suprasternal Notch (STN) to Nipple Areolar Complex (NAC), and NAC to Inframammary Crease (IMC) were taken. The peri areolar lifting and glandular duplication can be performed alone See (Figure 1), which shows preoperative (left) and postoperative 12 month (right) photographs of a patient undergoing implant removal and total capsulectomy with periareolar lifting and glandular duplication without new implant placement.)

Figure 1: Round implants, Mentor 380 cc, duale plane position, implanted for 20 years, capsular fibrosis Baker III on both sides
Markings for glandula-duplication and inferior mastopexy were selected on the basis of the NAC to IMC distance. The IMC was marked all along its width, and a midline was marked between the STN and xiphisternum. The incision for the glandula-dublication was designed along the IMC (Figure 2).
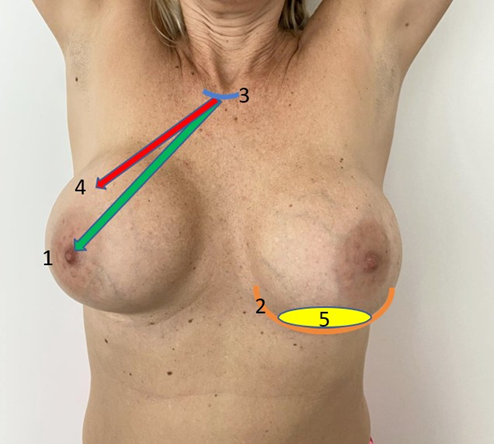
Figure 2: Markings and reference points. 1: MAC (mammilla areola complex); 2: IMC (infra mammary crest); 3: Incisory jugular; 4: Neo-Mac; 5: Glandular duplication.
The area of de-epithelialization is measured and planed in advance on the standing patient. The post-operative position on the NAC = neo-NAC was measured and marked in advance on the standing patient. The neo-NAC was marked on the breast meridian line, using the IMC as the reference. A 3.8-4.2cm nipple marker was used to mark the neo-NAC, depending on the expected postexplantation breast seize. These markings were always checked and adjusted as necessary before and after explantation for safe and tension-free closure. Following total capsulectomy, tailor tacking was performed and skin excess resected superior to the nippleareola complex such that the breast envelope and nipple-areola complex were appropriately positioned on the chest wall. The skin within the superior and inferior incisions was deepithelialized for auto augmentation of the upper and lower poles. In addition, we position a Binelli suture around the NAC, to stabilize the lifting effect. We recommend the placement of quilting sutures between the breast and the thorax wall, To prevent NAC migration to control postoperative ptosis and minimize risk of seroma formation. Drains were used in case of the implant ruptures. Closure was performed in layers using 3-0 and 4-0 Monocryl for subcutaneous and intradermal closure, respectively. Complete intact capsulectomy was performed in Grade II - IV capsules presenting in the sub glandular pocket and complete intact, complete or close to complete intact capsulectomy was performed in submuscular pockets. Capsules were sent for histopathology, and where necessary or excess fluid was present, samples were taken for CD30 analysis [16].
Results
Between 09.2020 and 12.2024 a total of 102 patients, who gave informed consent for scientific Publishing, had their implants removed and opted for periareolar lifting and glandular-duplication after implant removal in our clinic. All patients were routinely followed up for at least six months to two years. There was no postoperative ptosis observed. Major complications which needed an intervention: No patient experienced intra-operative Bleeding, one post-operative bleeding (no transfusion necessary), one Infection (intervention necessary), 6 patients experienced seroma, there was no wound breakdown or nipple necrosis, 4 patients received additional scar treatment (Needeling) (Table 1). Peri- and
Postoperative Complications
|
Complication |
Number of Patients |
|
Post-operative bleeding |
1 |
|
Wound Infection |
1 |
|
Seroma |
6 |
|
Hyperthrophic Scarring |
4 |
Table 1: Number of complications
Discussion
As the debate about the safety of breast implants continues, the high number of patients seeking explantation after cosmetic and reconstructive breast augmentation with implants will remain unchanged or increase. The decision to undergo periareolar lift and glandular duplication should ideally be an informed consent process to address these patients’ concerns about potential complications. Patients should be adequately counseled prior to surgery regarding the indications and contraindications, the risks involved, the financial implications and the postoperative appearance. Loss of feminine silhouette and changes in breast shape or volume following non-replacement explantation may not be acceptable to every patient and therefore need to be addressed appropriately. The decision to explantation can be challenging because mastopexy combined with skin envelope resection further reduces breast volume and results in well visible dominant scars. This may be even more in the case of prior axillary augmentation. Explantation alone may leave patients with empty breasts and worsen breast ptosis. Several authors have reported surgical approaches to overcome this challenge. Netscher published a review of the records and outcomes of aesthetic and reconstructive patients who have undergone implant removal. Netscher concludes: This study allows us to be optimistic about postoperative outcomes after breast implant removal. We have started to advise selected patients that implant removal combined with mastopexy offers a more pleasing aesthetic outcome than implant removal alone [17,18].
Khan presented a case series which presents an option of breast volume preservation and reshaping during mastopexy after breast implant removal that can be offered to selected patients. In the current case series, de-epithelialised dermo glandular flap mastopexy was used as an autologous tissue for breast reshaping and remodeling [8]. Attempts to minimize scarring have resulted in several publications describing techniques that produce a vertical scar. The advantages of the technique presented here are that it minimizes the skin scar in cases of vertical mammoplasty. In cases where vertical mammoplasty techniques are used and optimizes the breast shape after breast implant removal in patients who do not want a new implant [19]. However, these vertical scars are often not acceptable to many patients as they are still very visible and create an additional scar. A safe option was presented by Miller especially addressing implant removal by means of total capsulectomy in the sub glandular augmentation patient. This presents a technical challenge because of the profound effects of the implant on both the gland and overlying skin envelope. A complication of skin flap necrosis is devastating in any patient but can be distinctly so in the cosmetic patient population. The omega lift has been validated in the setting of breast reconstruction in high-risk patients [12]. But also, here the patients will have to face a well visible new scar.
To avoid additional scars for implant removal and capsulectomy after primary breast augmentation using the axillary approach an endoscopic approach was presented by Yu et al and Li et al. Endoscopic trans axillary capsulectomy can be completed through the axillary incision. The technique successfully removed the fibrous capsule, eliminated the needed for an incision on the breast, and created an incision far from the breast for completion of the procedure [20,21]. Both publications lack a solution for postoperative exacerbating breast ptosis. Implant explantation procedures can be performed alone or in combination with other techniques to restore volume. Depending on the native volume, the shape and the elasticity of the remaining breast tissue, implant removal can be also associated with mastopexy, auto-augmentation mammoplasty or fat graft. Mangialardi presented an article which portrays his series of combined mastopexy and lipofilling after implant explantation for revising unsatisfactory outcomes of breast augmentation [22]. Implant removal by means of total intact capsulectomy in breast augmentation patient presents a technical challenge because of the profound effects of the implant on the overlying tissues (muscle, glandular and fat tissue and skin) and the position and characteristics of the capsule. As a result, we can find a variety of publications describing possible surgical approaches. Some including a variety of approaches regarding the capsules. Including total capsulectomy and sole implant extraction leaving the complete capsule inside the patient. In addition, the aesthetic results can vary greatly [23].
There is currently no defined treatment approach for aesthetic patients who request the removal of their implants, particularly with regard to the treatment of the capsule. It is unclear whether a complete capsulectomy, a complete intact capsulectomy or a “en bloc” capsulectomy is necessary in these patients, as in patients with BIA-ALCL. Since there are no clear guidelines on how to treat the capsule in asymptomatic patients, the basic principles of breast revision surgery can be applied to these patients [24]. Recent clinical and histopathologic evidence suggests that uneventful resolution of the remaining capsule is not always the case, and several potential problems may arise from retained capsules after removal of the implant. Retained implant capsules may result in a spiculate mass suspicious for carcinoma, dense calcifications that obscure neighboring breast tissue on subsequent imaging studies, and cystic masses due to persistent serous effusion, expansile hematoma, or encapsulated silicone filled cysts. Furthermore, retained capsules are a reservoir of implant-related foreign material in the case of silicone gel-filled implants and textured or polyurethane coated implants promoting tissue ingrowth. To avoid complications from retained capsules, total capsulectomy or postoperative surveillance should be offered to patients [4]. Colobrace in addition introduce an evidence-based algorithm for the management of the explantation patient. In his review with a focus on the rationale, planning, and management of patients with an uncomplicated, asymptomatic textured implants [25]. In addition to a secure, evidence-based approach towards implant and capsule removal, we focus on the aesthetic needs and demands of our patients. So far, we could not find a publication offering a safe and reliable surgical technique for replacement-less implant removal with minimal additional scarring and aesthetic results combined with high patient satisfaction, as described in this paper. This paper is the result of our literature research and the innovative surgical approach developed by us.
Limitations
The presented results are solely based on clinical routine procedures which are evidence based. Therefore, this report lacks of systematic data collection and statistics or any other high-quality data collection and analysis. Although most patients were satisfied with the outcome, no patient satisfaction rating was performed.
Conclusion
Periareolar lifting and glandular duplication yields safe and aesthetic results, for patients with prior breast augmentation. Periareolar lifting and glandular duplication offers safe and reliable results in patients with atrophic glandular tissue as well as for patients with sufficient autologous tissues. Periareolar lifting and glandular duplication yields a safe surgical technique and superior overview during the challenging surgical procedure of total intact capsulectomy, total capsulectomy or near-total capsulectomy.
The results of this report provide a starting point for further investigations such as retrospective and prospective studies, with appropriate statistic evaluations using validated methods.
Acknowledgments: We thank Mrs. Holle Nester (www.hnmarcomundtext.de), for critically reviewing the manuscript with regard to grammar and spelling. We thank the Munich Study Center (BMBF-funded; No. of grant: 01KN1104) for their excellent and critical reviewing the manuscript.
Ethics Committee: This evaluation did not need approval of the ethics committees by German law.
Disclosure: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Pötschke J, Thamm O, Von Fritschen U, Fricke A, Richter-Heine I, et al. (2023) Brustimplantat-assoziierte Erkrankungen. Plastische Chirurgie 23: 42-51
- American Society of Plastic Surgeons (2024) national plastic surgery statistics 2024.
- Rohrich RJ, Kaplan J, Dayan E (2019) Silicone implant illness: Science versus myth? Plast Reconstr Surg 144: 98-109.
- Hardt NS, Yu L, LaTorre G, Steinbach B (1995) Complications related to retained breast implant capsules. Plastic sug 95: 364-371.
- Jong WH, Panagiotakos D, Proykova A, Samaras T, Clemens MW, et al. (2021) Final opinion on the safety of breast implants in relation to anaplastic large cell lymphoma: Report of the scientific committee on health, emerging and environmental risks (SCHEER), Regulatory Toxicology and Pharmacology 125: 104982.
- Corinne WE (2020) Understanding Breast Implant Illness, Before and After Explantation: A Patient-Reported Outcomes Study. Annals of plastic surgery 85: S82-S86.
- Corinne WE, Joseph Y, Samuel B (2021) The objective effect of breast implant removal and capsulectomy on pulmonary function. Plastic and Reconstructive Surgery-Global Open 9: e3636.
- Khan UD, Naseem S, Rafiq S (2022) Mastopexy using de-epithelialised dermoglandular flaps: a case series for maximal volume conservation following breast implants removal. Eur J Med Res 27: 159.
- Khan UD (2012) Breast expansion in augmentation mammoplasty: comparative data analysis in submuscular and subglandular planes. J Muhammad Med Coll 3: 8-10.
- Khan UD (2018) Use of Nipple Areolar Complex to Inframammary Crease Measurements to Reduce Bottoming Out After Augmentation Mastopexy. In: Mugea TT, Schifmann MA, editors. Aesthetic Surgery of the Brest. Berlin Heidelberg: Springer-Verlag 2018.
- Roxo AC, Nahas FX, Salin R, de Castro CC, Aboudib JH, et al. (2016) Volumetric evaluation of the mammary gland and pectoralis major muscle following subglandular and submuscular breast augmentation. Plast Reconstr Surg 137: 62-69.
- Miller JE, Goodreau AM, Blanchet NP (2020) Omega Lift after Total Capsulectomy in Prior Breast Augmentation. Plast Reconstr Surg 146: 835e-836e.
- Davies K, Allan L, Roblin P, Ross D, Farhadi J (2011) Factors affecting post-operative complications following skin sparing mastectomy with immediate breast reconstruction. Breast 20: 21-25.
- Santanelli di Pompeo F, Sorotos M, Laporta R, Pagnoni M, Longo B (2018) Efficacy of double mirrored omega pattern for skin sparing mastectomy to reduce ischemic complications. J Plast Surg Hand Surg 52: 14-19.
- Jonathan E. Miller, Adam M. Goodreau, Nadia P. Blanchet (2020) Omega Lift after Total Capsulectomy in Prior Breast Augmentation. Plastic and Reconstructive Surgery 146: 835-836.
- Jones JL (2019) BIA-ALCL : an overview of presentation and pathogenesis and guidelines for pathological diagnosis and management. Histopathology 75: 787-796.
- Netscher DT, Sharma S, Thornby J, Peltier M, Lyos A, et al. (1997) Aesthetic outcome of breast implant removal in 85 consecutive patients. Plast Reconstr Surg 100: 206-219.
- Li Yu, Jian Wang, Bo Zhang, Chang Zhu (2006) Endoscopic Transaxillary Capsulectomy Aesthetic Plastic Surgery 30: 282-285.
- Hönig JF, Frey HP, Hasse FM, Hasselberg J (2010) Inferior pedicle autoaugmentation mastopexy after breast implant removal. Aesthetic Plast Surg 34: 447-454.
- Yu L, Wang J, Zhang B, Zhu C (2008) Endoscopic transaxillary capsular contracture treatment. Aesthetic Plast Surg 32: 329-332.
- Li Yu, Jian Wang, Bo Zhang, Chang Zhu (2012) Treatment of Breast Injection with Polyacrylamide Hydrogel with Infiltrated Fascia Capsule Removal: Report on 104 Cases. Aesthetic Plastic Surgery 36: 112011127.
- Mangialardi ML, Ozil C, Lepage C (2022) One-Stage Mastopexy– Lipofilling after Implant Removal in Cosmetic Breast Surgery. Aesth Plast Surg 46: 1542-1550.
- Tanna N, Calobrace MB, Clemens MW, Hammond DC, Nahabedian MY, et al. (2021) Not All Breast Explants Are Equal: Contemporary Strategies in Breast Explantation Surgery. Plast Reconstr Surg 147: 808-818.
- Gabriel A, O’Rorke E, Maxwell GP (2021) Applying Principles of Breast Revision to Managing Aesthetic Patients with Textured Implants. Plast Reconstr Surg 147: 24S-30S.
- Calobrace MB (2021) Elective Implant Removal and Replacement in Asymptomatic Aesthetic Patients with Textured Devices. Plast Reconstr Surg 147: 14S-23S.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.