Perforated Left Colon Tumors: A Series of 5 Cases
by Fathillah El Karim Maaroufi*, Mohamed Boulatar*, Soumaya Jamil, Wafa Aitbelaid, Tariq Ahbala, Khalid Rabbani, Abdelouahed Louzi
Department of General Surgery, ARRAZI Hospital, Mohammed VI University Hospital Center, Faculty of Medicine and Pharmacy, Cadi Ayad University, Marrakech, Morocco
*Corresponding author: Fathillah el karim MAAROUFI , ARRAZI Hospital, Mohammed VI University Hospital Center, Faculty of Medicine and Pharmacy, Cadi Ayad University, Marrakech, Morocco; Mohamed BOULATAR, Department of General Surgery Department, ARRAZI Hospital, Mohammed VI University Hospital Center, Faculty of Medicine and Pharmacy, Cadi Ayad University, Marrakech, Morocco
Received Date: 11 December 2025
Accepted Date: 16 Decemner 2025
Published Date: 18 December2025
Citation: Keating Coffey T, Coffey JC, Fleming CA (2025) Perforated Left Colon Tumors: A Series of 5 Cases. J Surg 10:11516 https://doi.org/10.29011/2575-9760.011516
Abstract
Perforation of left colon tumors is a rare complication of colon tumors; it is a surgical emergency because it leads to fecal peritonitis, which can be fatal, hence the importance of immediate treatment. We conducted a retrospective study at the general surgery department of Mohammed VI University Hospital in Marrakech, focusing on 5 cases (n=5) of perforated left colon tumors. In this series of cases, we studied the characteristics and surgical strategy for left colon tumors with perforation. with the goal of demonstrating the importance of rapid and multidisciplinary care.
Keywords: Left Colon; Perforation; Tumors
Introduction
Perforation of the colon is rare and usually requires emergent surgery. It is associated with a high mortality and high morbidity [1]. It’s a therapeutic emergency and requires careful multidisciplinary care, involving the surgeon, radiologist, and anesthesiologist-resuscitator. Laparoscopic colonic resection remains the ideal choice in the absence of any contraindications.
Method
This is a retrospective study conducted over a one-year period from January 2025 to December 2025 at the General Surgery Department of Mohammed VI University Hospital in Marrakech, which included all perforated sigmoid tumors.A total of 5 cases of perforated sigmoid tumor. For all our patients, the diagnosis was suspected on clinical, biological, and radiological findings and confirmed by surgery. All other causes of sigmoid perforations were excluded.A reference sheet was used to collect data from the archived records at the Mohammed VI University of Marrakech. We have specified the epidemiological, clinical, biological, and radiological characteristics for each case. We also compiled the results and methods over a one-year period within the general surgery department of the hospital's abdominal cavity exploration center, as well as the evolutionary aspects after treatment.
Result
|
Case 1 |
Case 2 |
Case 3 |
Case 4 |
Case 5 |
|
|
Age |
35 |
64 |
34 |
48 |
50 |
|
Sex |
F |
M |
F |
M |
M |
|
Socio-economic level |
Low |
Low |
Medium |
Medium |
Medium |
|
Health coverage |
- |
- |
+ |
+ |
+ |
|
Medical history |
Treatment for his tumor |
- |
Treatment for his tumor |
- |
- |
|
Beginning of symptoms |
1 day |
2 days |
7 days |
10 days |
6 days |
|
Functional signs |
|||||
|
Abdominal pain |
+++ |
+++ |
+++ |
+++ |
+++ |
|
Vomiting |
- |
+ |
- |
- |
+ |
|
Others |
- |
- |
- |
Fever |
- |
|
Clinical signs |
|||||
|
Hemodynamic instability |
- |
- |
- |
- |
- |
|
Abdominal defense |
Pelvic |
Generalized |
Pelvic |
Generalized |
Generalized |
|
Digital Rectal Exam |
Normal |
Normal |
Normal |
Normal |
Normal |
|
biology result |
|||||
|
infectious syndrome |
+ |
+ |
+ |
+ |
+ |
|
impact assessment |
Normal |
Normal |
Normal |
Normal |
Normal |
|
CT abdominal and pelvic result |
|||||
|
Circumferential and irregular thickening |
+ |
+ |
+ |
+ |
+ |
|
Peritoneal effusion |
+ |
+ |
+ |
+ |
+ |
|
Collection |
- |
- |
- |
+ |
+ |
|
Pneumoperitoneum bubbles |
+ |
+ |
+ |
- |
- |
|
Localisation |
Sigmoid loop |
Sigmoid loop |
Rectosigmoid junction |
Sigmoid loop |
Descending colon |
|
Treatment |
|||||
|
Colic resection and Hartmann colostomy |
Sigmoid resection |
Sigmoid resection |
Anterior rectal resection |
Sigmoid resection |
Left colectomy |
|
Washing and drainage |
+ |
+ |
+ |
+ |
+ |
|
Antibiotic |
+ |
+ |
+ |
+ |
+ |
The age range of our patients varied between 34 and 64 years with an average of 46 years. A predominance of males was noted, 3H/2F. 40% of the patients were from a low socioeconomic level and had no medical coverage. 2 patients were already being followed in oncology for a sigmoid tumor.The duration between the onset of symptoms and admission varied from one to ten days, with an average of 5,2 days. The major sign in all our patients was sudden onset abdominal pain (100%), vomiting was present in 40% of cases (n=2/5), and fever in one patient, or 20%.All patients were hemodynamically stable; abdominal guarding was observed in all patients, 60% of which was general and 40% was pelvic; digital rectal examination was normal.A biological infectious syndrome was present in all our patients with a normal biological impact assessment. Abdominal and pelvic CT confirmed circumferential and irregular thickening of the left colon with peritoneal effusion in all patients, two of them also had a collection and three had pneumoperitoneum bubbles.Surgical exploration confirmed the diagnosis and revealed tumor perforation with purulent effusion in all 5 patients. The perforation tumor located in the descending colon, the rectosigmoid junction, and 3 in the sigmoid loop.

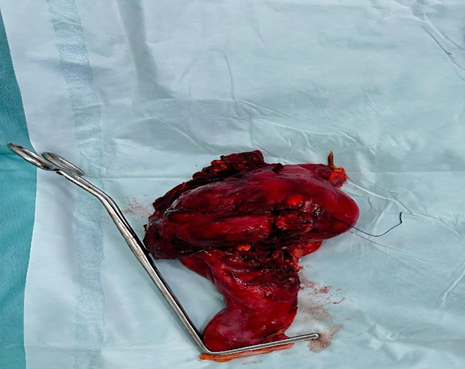
Figure 1 and 2: Perforated tumor of the sigmoid.

Figure 3: Rectosigmoid junction perforated tumor.
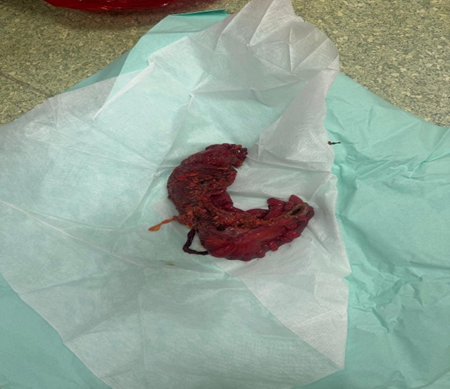
Figure 4: Perforated descending colon tumor.
A colon resection and Hartmann's stoma construction associated washing and drainage, with antibiotic therapy, were performed on all patients. The therapeutic evolution was favorable in all patients with return home on the 4th postoperative day. All pathology results supported the diagnosis of adenocarcinoma.
Discussion
About 2 to 12% of patient with colorectal disease present with perforation making it the second most common emergency presentation of colorectal cancer patients [2,3]. The causes of perforation include malignancy (36%), spontaneous perforation (20%), iatrogenic perforation (20%) and diverticulum (19%) among others [1] , [4]. all of our patients had spontaneous perforations.For patients with colon cancer, colonic perforation is not a common complication, and the incidence ranges from 2.6 to 10% [1,5]. the most frequent perforation site is the sigmoid colon [1,66]. In our case series, sigmoid perforation was the most common.There are two mechanisms underlying colorectal cancer perforation; perforation at the cancer site because of tumor necrosis, and perforation induced by blowing out of the distended proximal colon due to tumor obstruction [1]. A number of studies have shown that perforation proximal to the cancer site carries a poorer prognosis than cancer site perforation. In our series, all patients had a perforation at the tumor site [5,7,8]. In our series, all patients had a perforation at the tumor site.Perforation of colon cancer usually requires emergent surgery. The patients are predominantly aged, and their condition may be poor due to sepsis and accompanying diseases [1]. In our series the patients were young and all of them were the good condition.The optimum surgical treatment of colonic perforation with cancer remains controversial. There is no standardized protocol for the management of patients with colonic perforation, and the treatment strategy depends on the patient’s general condition and the experience of the primary surgeon [1]. Discontinuity resection, such as Hartmann’s procedure, is performed in most patients with perforation of left-sided colon cancers [9,10].
However, Hartmann’s operation carries a disadvantage of morbidity associated with the stoma and the need for a second operation to close the stoma and perform reconstruction, which may not be easy. All our patients underwent a colon resection with Hartmann's stoma creation.Many investigators have found that resection and primary anastomosis may be performed in selected patients. An abscess or fecal peritonitis is not a contraindication for anastomosis, but the presence of a major comorbidity, such as diabetes, renal failure, cardiovascular disease, compromised immunity, malnutrition or a high ASA score, is associated with a risk of leakage [11,12]. Furthermore, many reports have shown that single-stage resection with primary anastomosis and intraoperative colonic lavage carry almost the same rates of morbidity and mortality as multistage procedures [13,14]. The surgical approach for perforated colon cancer should be an oncologically curative operation for uncomplicated colon cancer. Showed that the pathway of complicated cancer is similar to that of uncomplicated cancer [15]. In our series all the patients had an an oncologically curative operation.Laparoscopy can be a useful approach for diagnosing the cause of an acute abdomen and help determine whether the laparotomy incision should be made at the upper or lower abdomen. In some cases, treatment can be completely performed laparoscopically without laparotomy [1]. A laparoscopic approach to perforated colon cancer may be difficult due to poor visibility and frail inflamed tissue. laparoscopic surgery for perforated colon cancer can be attempted by trained surgeons. A laparotomy was performed on all our patients.The morbidity and mortality rates after emergent surgery to treat perforation of colorectal cancer remain unclear, with mortality rates ranging from 5 to 40% [15,16]. all of our patients are still alive and receiving adjuvant chemotherapy.
Conclusion
colon cancer with perforation is associated with a high mortality and morbidity. The prognosis depends on the general condition and comorbidities of the patients. laparoscopic surgery should be performed when possible.
Conflicts of interest
The authors declare no conflicts of interest.
Authors contributions
All authors contributed to this work. Patient care: Fathiallah el karim MAAROUFI, Mohamed BOULATAR, Soumaya JAMIL; data collection and manuscript writing Fathiallah el karim MAAROUFI, Mohamed BOULATAR; manuscript revision: Fathiallah el karim MAAROUFI, Tariq AHBALA, Wafa AIT BELAID, Khalid RABBANI, Abdelouahed LOUZI. All authors have read and approved the final version of the manuscript.
References
- Otani K, Kawai K, Hata K, Tanaka T, Nishikawa T, et al. (2019) Colon cancer with perforation. Surgery Today 49: 15‑20.
- Tzivanakis A, Moran BJ (2020) Perforated Colorectal Cancer. Clinics in Colon and Rectal Surgery 33: 247‑252.
- Baer C, Menon R, Bastawrous S, Bastawrous A (2017) Emergency Presentations of Colorectal Cancer. The Surgical Clinics of North America 97: 529‑545.
- Shinkawa H, Yasuhara H, Naka S, Yanagie H, Nojiri T, et al. (2003) Factors affecting the early mortality of patients with nontraumatic colorectal perforation. Surgery Today 33: 13‑17.
- Tan KK, Hong CC, Zhang J, Liu JZ, Sim R (2010) Surgery for perforated colorectal malignancy in an Asian population : An institution’s experience over 5 years. International Journal of Colorectal Disease 25: 989‑995.
- Facteurs prédictifs de l’évolution après une intervention chirurgicale pour perforation colique : Expérience d’un établissement sur 6 ans—PubMed. (s. d.). Consulté 7 décembre 2025, à l’adresse
- Obstruction et perforation dans l’adénocarcinome colorectal : Analyse du pronostic et des tendances actuelles—PubMed. (s. d.). Consulté 7 décembre 2025, à l’adresse
- Alvarez JA, Baldonedo RF, Bear IG, Truán N, Pire G, Alvarez P (2005) Presentation, treatment, and multivariate analysis of risk factors for obstructive and perforative colorectal carcinoma. American Journal of Surgery, 190: 376‑382.
- Perforated colorectal carcinomas—PubMed. (s. d.). Consulté 7 décembre 2025, à l’adresse
- Runkel NS, Hinz U, Lehnert T, Buhr HJ, Herfarth C (1998). Improved outcome after emergency surgery for cancer of the large intestine. The British Journal of Surgery 85: 1260‑1265.
- Mulherin JL, Sawyers JL (1975) Evaluation of three methods for managing penetrating colon injuries. The Journal of Trauma 15: 580‑587.
- Gonzalez R, Smith CD, Ritter EM, Mason E, Duncan T, et al. (2005) Laparoscopic palliative surgery for complicated colorectal cancer. Surgical Endoscopy 19: 43‑46.
- Radcliffe AG, Dudley HA (1983) Intraoperative antegrade irrigation of the large intestine. Surgery, Gynecology & Obstetrics 156: 721‑723.
- Kim J, Lee GJ, Baek JH, Lee WS (2014) Comparison of the surgical outcomes of laparoscopic versus open surgery for colon perforation during colonoscopy. Annals of Surgical Treatment and Research 87: 139‑143.
- Lee IK, Sung NY, Lee YS, Lee SC, Kang WK, et al. (2007) The survival rate and prognostic factors in 26 perforated colorectal cancer patients. International Journal of Colorectal Disease 22: 467‑473.
- Crowder VH, Cohn I (1967) Perforation in cancer of the colon and rectum. Diseases of the Colon and Rectum 10: 415‑420.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.