Paediatric Nondisplaced Comminuted Talar Neck Fracture – A Case Report
by Sofie Berggreen Jensen, Lise Langeland Larsen, Daniel Wæver*
Department of Orthopaedic Surgery, Randers Regional Hospital, Denmark
*Corresponding author: Daniel Wæver, Department of Orthopedic Surgery, Randers Regional Hospital, Skovlyvej 15, 8930 Randers, Denmark
Received Date: 01 May, 2025
Accepted Date: 14 May, 2025
Published Date: 16 May, 2025
Citation: Sofie Berggreen Jensen, Lise Langeland Larsen, Daniel Wæver (2025) Paediatric Nondisplaced Comminuted Talar Neck Fracture – A Case Report. J Orthop Res Ther 10: 1384. https://doi.org/10.29011/2575-8241.001384
Abstract
Paediatric talus fractures are extremely rare, particularly in children under 12 years of age, with an annual incidence of 0.010.08%. The intricate vascularity and anatomy of the talus makes it susceptible to serious complications. Talus fractures and potential complications, such as avascular necrosis, osteoarthritis and non- or malunion are well-documented in adults, and the severity of complications typically correlates with the severity of the fracture. The literature discusses whether children experience complications from talus fractures similarly to adults and examines the possibility that children may be more susceptible to severe outcomes, even in cases of less severe fractures and lower-energy trauma.
We present the case of a four-year-old boy with a comminuted, non-displaced talar neck fracture after a fall from two meters treated conservatively with a walking boot for four weeks. The first 10 days without weightbearing followed by partial weightbearing. We found no complications at follow-up with normal radiographs.
Although it can be challenging to recognize these fracturs in children it is important to identify these fractures early due to the possible complications, such as avascular necrosis, post-traumatic arthritis and non-union. Current literature indicates that non-displaced fractures in paediatric patients may occur following minimal trauma and even these fractures can lead to serious complications. Initial use of computer tomography is recommended to enhance diagnostic accuracy.
Keywords: Talus fracture, Orthopaedic, Children, Avascular necrosis, Trauma,
Introduction
Paediatric talus fractures are rare with a reported annual incidence of 0.01-0.08%. In childhood, there is a high proportion of cartilage in the talus, which provides greater resistance and flexibility [1]. This combined with the lower frequency of high-energy trauma, such as motor vehicle accidents and falls from heights, results in the low incidence of paediatric talar fractures [2]. The trauma mechanism is often extensive axial loading and dorsiflexion of the foot.
The vascularity of the talus is complex, and the injury pattern and complications correlate to the involved anatomy [3]. The head of the talus is vascularized by branches of the dorsalis pedis artery [3]. The main blood supply to the talar body derives from an anastomosis below the talar neck, formed by the artery of the tarsal canal (from the posterior tibial artery) and the artery of the tarsal sinus (from the perforating branch of the peroneal artery) [3]. The location and the retrograde blood flow to the talus makes it vulnerable to trauma [3,4]. Therefore, reduction and alignment of the fracture in the neck of the talus is necessary to restore reperfusion to the talar body to avoid compromised blood flow and the risk of complications such as avascular necrosis (AVN) in the talus [5].
Talar neck fractures in both children and adults can be classified according to the Hawkin’s classification into four types depending on displacement and involvement of surrounding joints [3,5,6]. Type I is a nondisplaced talar neck fracture, type II is a displaced fracture with subtalar dislocation or subluxation, type III is a displaced neck fracture with dislocation/subluxation of both tibiotalar and subtalar joints and type IV is a displaced neck fracture with dislocation/subluxation of the talonavicular, tibiotalar and subtalar joints [7]. Hawkin’s type I is considered the most common type of talus fracture [4,6].
In non-displaced fractures, conservative management with immobilization for six to eight weeks is generally sufficient and is considered the first line of treatment in children [3,5]. However, in more comminuted and displaced fractures with potential disruption of blood flow, urgent reduction and surgical intervention are required to minimize the risk of complications [8]. Fixation is most commonly performed either through open reduction and internal fixation using plate and/or screws, or percutaneously with Kirschner wires or external fixation, depending on the age, trauma and fracture type [1,4,8].
The most commonly reported complications following talar neck fractures in adults are AVN, non- or mal-union and osteoarthritis which generally correlate with the severity of the injury [5,7,8]. The existing literature now suggests that these possible complications may also occur in children, particularly in cases involving severe injuries [3,4,6]. Complications have primarily been studied in children over the age of 12, hence the complication rate for younger children remains unclear.
Case Presentation
A four-year-old boy with no previous injury to his feet or ankles was referred to the emergency department due to pain in his right foot and knee after a fall from approximately two meters. He had no other complaints. He was unable to bear weight on his foot. The patient suffered from traumatic brain oedema at birth with subsequent hearing loss but was otherwise healthy.
Clinically, there was no swelling or discoloration of the extremity. On palpation, there was soreness on the plantar aspect of the midfoot. No pain was noted dorsally or at the lateral or medial malleolus. There was no indirect pain in the first or second toes or metatarsals. The patient had fairly good range of motion in the ankle and normal function of the toes. The neurovascular status was intact.
Radiographs of the foot (Figure 1 & 2), reviewed by an orthopaedic surgeon and a radiologist, were described as normal, with no suspicion of fractures. Due to severe pain and lack of weightbearing the patient was treated with a walking boot.
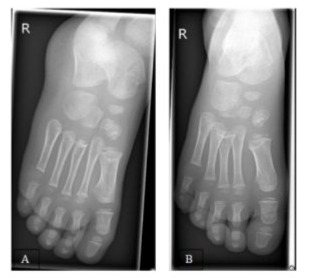
Figure 1: Initial (A) Mortise and (B) anterior-posterior radiographs of the right foot in the emergency department.

Figure 2: Initial lateral radiograph of the right foot in the emergency department demonstrating a cortical disruption in the talar neck.
The radiographs were re-evaluated the following day, and a non-displaced Hawkin’s type I talar neck fracture was identified (Figure 1 & 2). The parents were informed, and the patient was advised to avoid weight bearing until radiological follow-up 10 days post injury. At the 10-day follow-up, the patient reported no significant pain, and radiographs (Figure 3 & 4) demonstrated no displacement of the fracture. He was permitted to bear weight on the foot up to the pain threshold.
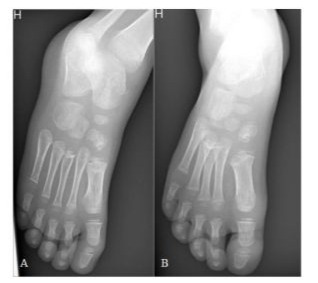
Figure 3: (A) Mortise and (B) anterior-posterior radiographs of the right foot at 10 days follow-up.

Figure 4: Lateral radiographs of the right foot at 10 days followup.
At the final follow-up four weeks later, there was no swelling. As expected, reduced motion of the ankle was noted due to immobilization. Radiographs (Figure 5 & 6) showed signs of healing and the walking boot was removed. He was now able to walk without any discomfort. There have been no new contacts to the hospital six months after the trauma. Further follow-up is not planned.
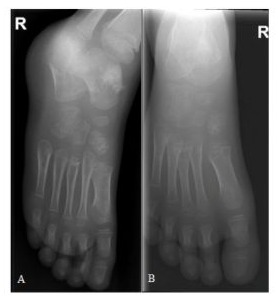
Figure 5: (A) Mortise and (B) anterior-posterior radiographs of the right foot at four weeks follow-up.
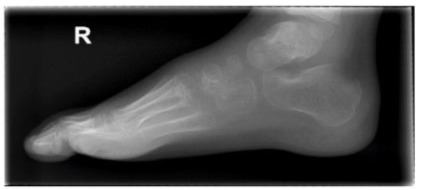
Figure 6: Lateral radiograph of the right foot at four weeks followup.
Discussion
Talus fractures are rare but can lead to potentially critical outcomes if not recognized due to its crucial role in foot mobility and its central involvement in the three major joints of the hindfoot [4]. We present a rare case report of a four-year old boy with a nondisplaced talar neck fracture following minimal trauma, treated non-operatively without complications at the four-week follow-up.
While complications such as AVN, posttraumatic osteoarthritis and persistent pain have been extensively documented in adults, the outcomes of talus fractures in children are less understood [7]. However, similar complications have also been reported in paediatric cases [4,5].
A more recent review from 2022 by Waseem et al. [6] included 31 studies and a total of 73 paediatric talar neck fractures. 23 fractures were described as Hawkin’s type I fractures, similar to the one in our case. Only one patient underwent surgery, while the remaining cases were treated with immobilization in a cast for an average of six weeks. There was a 100% union rate, but two cases of AVN (5.7%) in a five- and six-year-old boy, a similar age to our case. However, the diagnosis of AVN was confirmed two years after the trauma due to persistent pain. Three cases of osteoarthritis were reported, and one patient underwent arthrodesis of the ankle joints following external fixation after an open fracture, indicating a higher degree of severity. This could suggest the need for a longer follow-up in cases of even minimally displaced fractures or increased attention to these patients if they present new symptoms in the foot, as there is a risk of late complications. The overall rate of AVN in talar neck fractures was found to be 15.4% with the majority (53.5%) diagnosed following Hawkin’s type III talar neck fracture. Whether a higher grade of AVN occurs in children is difficult to determine due to the limited number of cases. Jordan et al. [7] investigated talar fractures in adults and found similar rates of AVN in Hawkin’s type I and II fractures, but a lower incidence of AVN in type III fractures (38.9%). Although they studied a noteworthy larger population of adults compared to the paediatric cohort in Waseem et al. [6], it is discussed whether the immature talus is less resistant to trauma and disruption of blood flow. Furthermore, this highlights the increased risk of AVN in more severe talar neck fractures in children.
Waseem et al. [6] reported the highest incidence of AVN after talar neck fracture in the age group 6–10-year-olds. In contrast, Kruppa et al. [4] and Eberl et al. [5] reported the highest incidence of AVN in adolescents rather than in children younger than 12 years (16–18-year-olds and over 12 years of age, respectively). This is discussed to be due to a link between high-energy trauma and severity of fractures in older age groups. In contrast, 75% of fractures in children under 12 years of age were caused by lowenergy trauma, also noted by Eberl et al. [5].
Waseem et al. [6] found no significant age difference between Hawkin’s type I and II–IV fractures, highlighting conflicting evidence regarding trauma severity and age.
Another case report by Byrne et al. [9] described a seven-yearold girl with a non-displaced comminuted talar neck fracture following a fall from a height similar to that in our case, with approximately the same treatment and outcome. This further supports the evidence, that non-displaced talar neck fractures can occur after low-energy trauma in children.
With the literature suggesting potentially critical outcomes for children with talar neck fractures, it is important to look into the initial assessment of the paediatric foot trauma cases. In adult talus fractures a CT scan is indicated to detect and characterize the fracture. It is also useful to detect other potential damages in the foot, since talus fractures often are accompanied by concomitant injuries, but the scan is also useful for pre-operative assessment [4,8].
In children under 12 years of age, the ossification of the talus has not yet fully occurred, making the diagnostics more challenging as seen in our case, where the initial diagnosis was overlooked [6]. Therefore, it could be suggested to use CT scans more routinely in younger children if the trauma and clinical presentation suggest talus fractures with potentially critical complications later in life. However, the use of excess radiation always has to be considered.
Conclusion
This case illustrates a rare occurrence of a paediatric talar neck fracture. Although talar neck fractures are uncommon in children, existing literature indicates that complications may arise even in non-displaced fractures. Even though study populations are limited, early recognition of these fractures is essential to prevent both early and late complications.
Acknowledges
None
Conflict of Interest
The authors declare no conflict of interest
Author contribution
SBJ drafted the report. DW assisted with the case and both DW and LLL drafted and edited the report. All authors approved the report.
Consent
Written and verbal consent from the patient’s parents were obtained.
References
- Rammelt S, Godoy-Santos AL, Schneiders W, Fitze G, Zwipp H, et al. (2016) Foot and ankle fractures during childhood: review of the literature and scientific evidence for appropriate treatment. Rev Bras Ortop 51: 630-639.
- Russell TG, Byerly DW (2025) Talus Fracture. StatPearls Publishing Copyright © 2025, StatPearls Publishing LLC, USA.
- Buza JA 3rd & Leucht P (2018) Fractures of the talus: Current concepts and new developments. Foot Ankle Surg 24: 282-290.
- Kruppa C, Tyler Snoap, Debra L Sietsema, Thomas A Schildhauer, Marcel Dudda (2018) Is the Midterm Progress of Pediatric and Adolescent Talus Fractures Stratified by Age? J Foot Ankle Surg 57: 471-477.
- Eberl R, Singer G, Schalamon J, Hausbrandt P, Hoellwarth ME (2010) Fractures of the talus-differences between children and adolescents. J Trauma 68: 126-130.
- Waseem S, Nayar SK, Vemulapalli K (2022) Paediatric talus fractures: A guide to management based on a review of the literature. Injury 53: 1029-1037.
- Jordan RK, Bafna KR, Liu J, Ebraheim NA (2017) Complications of Talar Neck Fractures by Hawkins Classification: A Systematic Review. J Foot Ankle Surg 56: 817-821.
- Fournier A (2012) Total talar fracture - long-term results of internal fixation of talar fractures. A multicentric study of 114 cases. Orthop Traumatol Surg Res 98: S48-55.
- Byrne AM, Stephens M (2012) Paediatric talus fracture. BMJ Case Rep 2012:bcr1020115028.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.