Ovarian Neoplasm Versus Ovarian Lymphoma: A Literature Review with Focus on Radiology and Pathology Features
by Diana Donatello*
Radiologist, Indipendent Researcher Costa Contina Street 19, Vasto 66054, ITALY
*Corresponding author: Diana Donatello, MD, Radiologist, Indipendent Researcher Costa Contina Street 19, Vasto 66054, ITALY
Received Date: 27 December, 2023
Accepted Date: 02 January, 2024
Published Date: 05 January, 2024
Citation: Donatello D (2024) Ovarian Neoplasm Versus Ovarian Lymphoma: A Literature Review with Focus on Radiology and Pathology Features. Gynecol Obstet Open Acc 8: 176. https://doi.org/10.29011/2577-2236.100176
Introduction
Lymphomas are primary neoplasms of the immune system and arise within the lymphoid tissue with an incidence of approximately 8% of all neoplasms. They are divided into two groups represented by Hodgkin’s lymphomas, which owe their name to Thomas Hodgkin, an English doctor who discovered them in 1832, and the more heterogeneous group of non-Hodgkin’s lymphomas.
Hodgkin’s lymphomas, in addition to having a different histology compared to non-Hodgkin’s, generally present themselves as a nodal disease which continues to involve groups of adjacent lymph nodes, maintaining contiguity, with a low percentage of extranodal localizations which is between 2-5% of all Hodgkin lymphomas.
The areas most affected are the branches of the thoracic duct: supraclavicular, lateralcervical, mediastinal. Unlike nonHodgkin lymphomas, they do not maintain contiguity in their nodal presentation, but give rise to extranodal localizations with a frequency equal to 25-50% of all non-Hodgkin lymphomas and their spread is common.
They are divided into low- and high-level aggressive lymphomas. In non-Hodgkin lymphomas there is therefore a higher possibility of onset of the neoplastic pathology in precursors of lymphocytopoiesis that are located outside the secondary lymphoid organs, i.e. giving rise to extranodal manifestations.
By extranodal lymphoma we therefore mean either a lymphoma restricted to a single extranodal site and its regional lymph nodes, or a lymphoma which may be more widespread and in which an extranodal organ is the predominant site of the disease at which therapy may be primarily aimed [1] Virtually any organ may be affected by involvement extranodal, but the most commonly affected sites are the gastrointestinal tract, the skin, the central nervous system, the testis and a series of organs that are affected by the so-called lymphomas derived from the mucosaassociated lymphoid tissue (MALT) such as the stomach, salivary glands, the thyroid, the lung and the intestine.
Imaging techniques play a fundamental role in the noninvasive evaluation of patients with extranodal lymphoma, both for initial staging and during follow-up and in monitoring the response to treatment. In radiodiagnostics, the means most used in patients with lymphoma are ultrasound, CT, MRI and hybrid PET/CT.
In the past, evaluation and follow-up were mostly entrusted to CT alone, but nowadays hybrid PET/CT has proven to be the imaging tool with the highest sensitivity and specificity in the diagnosis, follow-up and restaging of lymphomas.
Lately, the use of Whole-Body Diffusion-Weighted MRI has been being tested in the evaluation of lymphoma and this technique, free of ionizing radiation, could become complementary to F18FDG PET/CT in the future, better safeguarding the patient’s health [1-4].
It is important to remember that the prevalence of lymphomas in the population is growing, consequently many more extranodal forms are observed in routine clinical practice, which is why it is important to make an early and most precise diagnosis of the neoplasm using the imaging techniques at our disposal [1]. This work specifically describes lymphomatous involvement of the ovary, which can present as primary or secondary in accordance with the definition of extranodal lymphoma.
Primary ovarian lymphoma is an extremely rare disease that occurs in 0.5% of all non-Hodgkin lymphomas and 1.5% of all ovarian cancers. Secondary lymphoma is generally the manifestation of disseminated lymphoma which occurs with a frequency of 7% of all lymphomas with systemic involvement [57].
On the other hand, although involvement of the genital tract by non-Hodgkin lymphoma is extremely rare, the ovary is the most frequently affected genital organ and secondary lymphoma at this site is the most common presentation. At the same time, information on the treatment and clinical figures of primary and secondary ovarian lymphoma is lacking [5-9]. As with all non-Hodgkin lymphomas, extranodal lymphoma with ovarian involvement can also be staged with the Ann Arbor classification (Table 1).
|
Stadio* |
Criteria |
|
I |
Only in one lymph node |
|
II |
In two or more lymph nodes on the same side of the diaphragm |
|
III |
In the lymph nodes, spleen, or both and on both sides of the diaphragm |
|
1 |
Above the renal vessels (e.g., spleen; splenic, hilar, celiac, and portal lymph nodes) |
|
2 |
In the lower abdominal region (lymph nodes) |
|
IV |
Extranodal involvement (eg, bone marrow, lung, liver) |
|
*Subclassification E indicates extranodal involvement adjacent to an involved lymph node (e.g., mediastinal lymph node disease and hilar adenopathy with adjacent pulmonary infiltration is classified as IIE). Stages can be further classified as A to indicate absence or B to indicate presence of constitutional symptoms (weight loss, fever, or night sweats). B symptoms typically occur with stages III and IV (20-30% of patients). |
|
Table 1: Ann Arbor staging for Hodgkin’s disease and for non-Hodgkin lymphomas.
It has been seen that the majority of primary ovarian lymphomas have a stage between I and II, therefore low grade, while in the case of a secondary lymphoma the stage is between III and IV, therefore a high grade. From this it can be deduced that the prognosis is better in primary lymphoma than in secondary lymphoma. However, we will see in the course of the discussion how the studies carried out on the survival of ovarian lymphoma are very complex and having a limited number of cases available, due to the rarity of the pathology, it is difficult to outline real statistics on the prognosis of these patients.
As regards histological representation, a greater prevalence of diffuse large B-cell ovarian lymphoma is evident, followed by follicular lymphoma, Burkitt’s lymphoma, anaplastic T-cell lymphoma and T-lymphoblastic precursors [10-19]. In the recent literature that we have analysed, several cases of primary and secondary ovarian diffuse large B-cell lymphoma are reported, which represents a clinically and biologically heterogeneous group of aggressive lymphomas which in many cases arises in extranodal sites such as the gastrointestinal tract, soft tissues, bone, breast, gonads and endocrine and exocrine tissues.
Follicular lymphoma is a small B-cell lymphoma that in most cases presents as a dissemination of nodal disease while it manifests as a primary lymphoma in a percentage of cases of 1015% and is well documented in sites such as the tract gastrointestinal tract, the testis, the thyroid, the breast, and the orbit [20,21]. Burkitt lymphoma is an aggressive lymphoma that can present at an extranodal site or as acute leukemia. It is a B-cell neoplasm that can be classified into three distinct clinical forms: endemic, sporadic and associated with immunodeficiency. The non-endemic form, also called American, has an abdominal presentation, often accompanied by ascites, with gastric, ileal, caecal, renal, ovarian, bone and central nervous system involvement [10-12,23,24].
Sometimes the presentation of Brurkitt’s lymphoma, like the onset of lymphoma pathology in general, can affect immunosuppressed subjects (for example HIV-positive subjects) or those who have undergone transplants (so-called post-transplant lymphoproliferative disorders) [23,25].
Aim of the study
The study we carried out has as its objective:
Outline the radiological aspects that best describe ovarian lymphoma, with particular attention to the differential diagnosis between lymphoma and other ovarian tumors, which may have a similar clinical and radiological presentation, underlining the importance of this distinction for the purposes of treatment.
This analysis is carried out a review of the literature.
Distinction between Primary, Secondary Lymphoma and Ovarian Cancer
Introduction
Malignant lymphoma of the female genital tract is unusual, however the ovaries are the most commonly affected site, with up to 25% of women with disseminated lymphoma having ovarian involvement [1].
Differences between Primary and Secondary Lymphoma
As we have said, ovarian involvement by lymphoma can be primary or secondary. The secondary can be of two types:
- an initial presentation of extra-ovarian occult disease
- a manifestation of a widely disseminated disease
The distinction is of considerable importance because primary extra-nodal lymphoma has a less aggressive course with a five-year survival rate of 80% compared to a disseminated malignant lymphoma which has a five-year survival rate of 33%. [5].
Ovarian lymphoma can present at any age, but the majority of affected women are around the age of 40. This type of lymphoma, whether primary or secondary, has various presentations, many of which are discovered incidentally during tests aimed at investigating problems concerning the abdominopelvic area, and present themselves in the form of abdominal or pelvic masses.
Even today it is difficult to ascertain whether an ovarian lymphoma is primary or secondary. In fact, the definition of primary lymphoma has been subject to controversy for years. Skodras et al [26], based on data from 15 cases of primary ovarian lymphoma, proposed that the definition of primary ovarian lymphoma should follow the following criteria:
- there is the presence of an ovarian mass, confined to one or both ovaries;
- lymphoma should be considered primary even if microscopic involvement of contiguous lymph nodes is detected;
- intraoperative and postoperative staging procedures do not reveal lymphoma in other parts of the body.
Talerman [27] states that even if there is local dissemination from the ovary to adjacent tissues, this manifestation should not preclude the diagnosis of primary lymphoma. On the other hand, Palagadu et al [28], argued that the criteria were too stringent and proposed that there should be a disease-free interval of at least 6 months after oophorectomy. Furthermore, some authors maintain that the reactive lymphocytes present in the ovary affected by lymphomatous pathology can secondarily populate the latter in response to various ovarian lesions, such as PID, endometriosis, benign and malignant neoplasms, and the most common luteal and follicular cysts [29]. However, there are many confirmed cases that present no evidence of inflammation either clinically or histologically [30].
Analysis of a clinical case diagnosed with secondary ovarian lymphoma: Below is an article, unique in its description, being the only case present in the literature that describes in detail, in the form of a “case report”, the difference between a primary and secondary ovarian lymphoma, given that their presentation clinical in most cases is identical.
Case Description
Crasta et al [5] report the case of a 44-year-old woman who presented with abdominal pain and dyspepsia lasting three months. The objective examination reveals the presence of a soft abdominal mass in the right iliac fossa, which appears to arise from the pelvis and extend above the navel. Transvaginal examination reveals the presence of a mass in the Douglas pouch pushing the uterus to the left side. Ultrasound examination of the abdominopelvic wall shows a mass in the right ovary and a second mass in the right iliac fossa. Eco-Doppler detects a fair vascularization of the masses and MRI shows hypointense images on T1 and hyperintense on T2. The patient undergoes a colonoscopy which reveals the presence of a large ulcerated submucosal nodule which occupies half the circumference and obstructs the lumen. All tumor markers are normal.
The biopsy reveals an inflammatory infiltrate in the lamina propria with many artifacts, so a definitive diagnosis cannot be made. Exploratory laparoscopy shows an intact and wellencapsulated tumor in the right ovary. The mass in the iliac fossa appears inflamed with the presence of pus in the paracolic recess, thickening of the intestinal wall and omental adhesions. Then the abscess is drained with subsequent salpingo - oophorectomy. The right ovarian mass measured 8.5 x 6.0 x 3.0 cm and was solid and whitish-gray in color.
The microscopic examination of the mass reveals that the ovarian tissue is covered by a diffuse carpet of medium-sized cells, with some large cells (Figure 1) in foci, forming cords and trabeculae. The cells have scant cytoplasm, nuclei with aggregated chromatin, and numerous nucleoli (Figure 2). The immunohistochemical examination highlights the presence of cells positive for LCA and negative for cytokeratin, therefore the diagnosis of non-Hodgkin lymphoma with ovarian, omental and peritoneal involvement is made (most likely a diffuse large B-cell lymphoma). The patient undergoes a CT scan for a post-operative check-up which detects multiple lymph node enlargements in the common iliac, internal iliac and external iliac groups. Bone marrow biopsy reveals no marrow infiltrates. The patient is subjected to a chemotherapy protocol which includes 6 cycles of CHOP, but despite the therapy there is progression of the lymphoma with subsequent renal and splenic involvement.
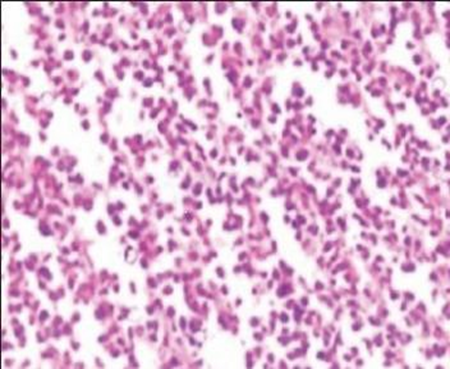
Figure 1: The image shows an ovarian tissue rich in medium volume cells, with large cells in foci, which form cords and trabeculae.
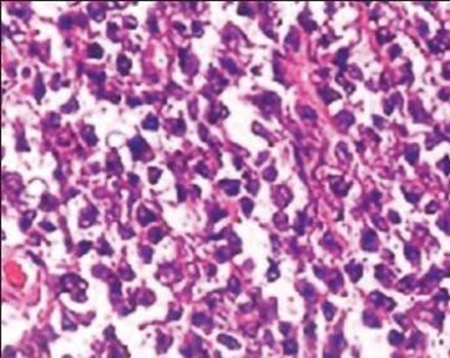
Figure 2: The image shows cells with little cytoplasm, numerous nucleoli and nuclei with aggregated chromatin
Discussion
It is important to take this clinical case into consideration to better understand the difficulty linked to the differential diagnosis between primary and secondary ovarian lymphoma. In fact, this patient who initially, therefore pre-operatively, presents without evident generalized lymphadenopathy could be mistakenly considered as suffering from primary ovarian lymphoma.
On the other hand, the positivity of the iliac lymph node stations after surgery leads towards the diagnosis of secondary lymphoma with initial ovarian presentation but with occult extraovarian disease. Crasta cites an article dating back to 1998 written by Ferrozzi [31], who was one of the first authors to describe the role of imaging techniques in the diagnosis of ovarian lymphoma, underlining the possible difficulties involved in the differential diagnosis between primary and secondary ovarian lymphoma ( for example in the case in which the secondary presents as an occult extraovarian localization) and ovarian tumor.
In fact, he carried out a study with 8 patients between the ages of 13 and 70, all affected by ovarian lymphoma with a prevalent diffuse large B-cell histology, but with the presence also of patients affected respectively by Burkitt’s lymphoma, follicular cell , lymphoplasmacytoid and immunoblastic. There are both primary and secondary ovarian lymphoma cases. The radiological characteristics of lymphoma with ovarian localization that Ferrozzi finds in his study and which are of fundamental importance even today are:
- frequent absence of ascites;
- frequent bilaterality in secondary ovarian lymphomas;
- solid formations on ultrasonography and presence of a discrete vascularization on Eco-Color-Doppler;
- CT highlights the lesions as hypodense and with a slight increase in densitometric values a fter i.v. administration. of the contrast medium;
- MRI highlights homogeneous masses that are hypointense on T1-weighted images and slightly hyperintense on T2weighted images.
As we have seen above, the imaging results obtained in Crasta’s study [5] are also similar to the diagnostic criteria proposed by Ferrozzi [32].
Ovarian localized lymphoma versus ovarian cancer
In an article published in the British Journal of Radiology, Craswshaw et al [2] report a case of primary ovarian Burkitt’s lymphoma describing the imaging methods used in the diagnosis, via ultrasound, CT and MRI. The symptoms initially presented by the patient, a 28-year-old woman, are the same as those found by previous authors in cases of ovarian lymphoma, i.e. abdominal distention, lowering of abdominal pressure and increased frequency of urination.
Here too, the physical examination reveals a mass arising from the pelvis and extending just above the pubic symphysis. Three weeks after the visit the mass had grown to the level of the xiphosternum. There was no lymphadenopathy or hepatosplenomegaly, and the patient was not immunocompromised. The blood indices taken into consideration were elevated with an increase in CA-125 (1111 U ml), LDH (950 U L) and other markers such as alpha-fetoprotein (AFP), human chorionic gonadotropin (HCG) and antigen carcino-embryonic (CEA).
The ultrasonographic study shows two large masses, one in the left pelvic portion and the other in the right pelvic portion.
The masses appear homogeneous and slightly echogenic with small cystic areas around the periphery. There is a small amount of free fluid in the pelvis (Figure 3).
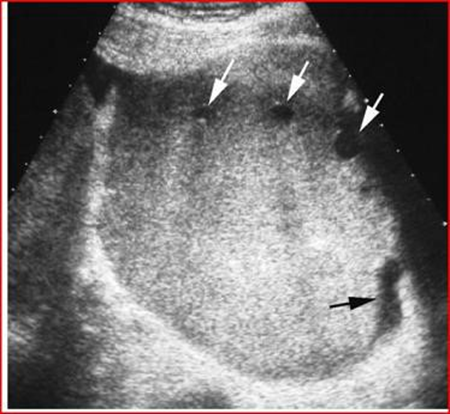
Figure 3: Transverse ultrasound shows a well-defined, homogeneous and hyperechoic mass, with focal cysts at the periphery (white arrows) and a small amount of free fluid (black arrow).
MRI shows a mass-free uterus, with no evidence of normal ovaries. The masses are approximately 13 cm in diameter and have low signal intensity on T1-weighted images and increased avidity after gadolin administration. On T2-weighted images the mass is hyperintense and the peripheral lesions probably correspond to ovarian follicles (Figures 4-6).
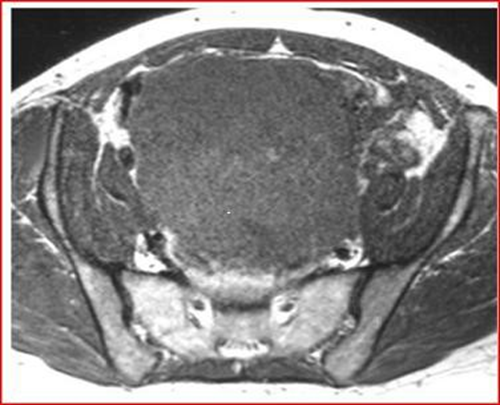
Figure 4: Axial T1-weighted MRI image, showing low signal intensity of the mass
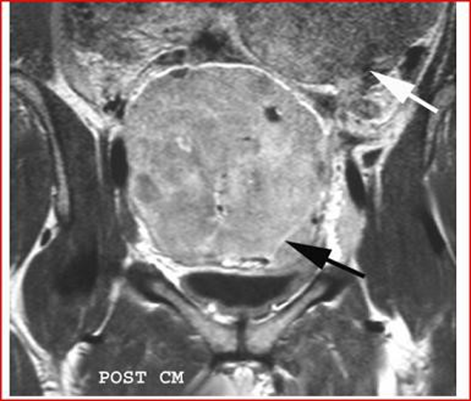
Figure 5: Coronal T1-weighted MRI image, performed by administration of intravenous gadolin, shows low signal intensity of the mass, the black arrow highlights an increase in the septal area. The second mass, white arrow, extends into the upper left quadrant.
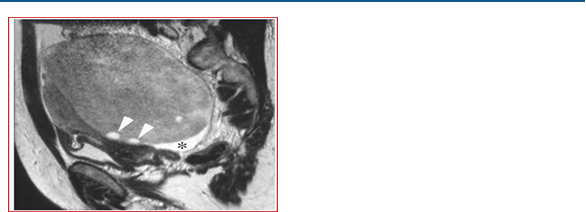
Figure 6: Sagittal T2-weighted MRI image of the pelvis, shows that the ovarian mass posterior to the uterus has an heterogeneous, intermediate-high signal intensity, the follicles in the periphery (arrow points), have a high signal intensity. The asterisk highlights the free liquid in the Douglas cord.
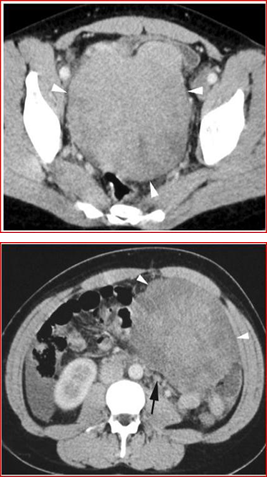
Figures 7 and 8: Axial CT images with contrast medium 7-8 show two masses (arrow points), one in the pelvis (Figure 7) and one in the left iliac fossa (Figure 8). The masses tend to displace the surrounding organs and free fluid is observed in the right area. Small retroperitoneal lymph nodes are also noted in the left paraaortic region (black arrow).
Abdominal and pelvic CT shows two contiguous solid masses. The small cysts on the periphery of the masses, identified by ultrasound and MRI, are not shown by CT which instead highlights the presence of some small retroperitoneal lymph nodes of approximately 1 cm. (Figures 7 and 8). There was no further adenopathy and the spleen was normal. Furthermore, the bone marrow aspirate did not contain infiltrates.
The needle biopsy performed on the right ovarian mass demonstrates the presence of a non-endemic Burkitt’s lymphoma.
The analyzed tissue shows the presence of a diffuse infiltration of intermediate-sized lymphoid cells with scant cytoplasm and round nuclei with areas of pleomorphism. The nuclei contain multiple nucleoli and frequent miosis is present. (Figure 9) The cells express CD20, CD10, bcl-6, and IgM but are negative for bcl-2. The nuclei Cytology demonstrates the presence of traslocation t (8; 14), given that it supports the diagnosis of Burkitt’s lymphoma with ovarian localization. The patient began chemotherapy treatment and CT performed 6 weeks after therapy showed a dramatic reduction in the volume of the mass. (Figure 10).
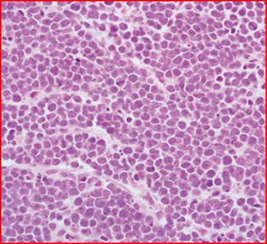
Figure 9: Hematoxylin-eosin section shows a diffuse population of medium-sized cells, with some dispersed macrophages. There are frequent mitoses and abundant apoptosis.

Figure 10: CT with contrast medium, performed six weeks after administration of two cycles of chemotherapy. The tumor (arrowheads) has significantly reduced in size.
We know that Burkitt lymphoma has been described in HIVinfected individuals and particularly in pediatric patients.
Due to an increase in the prevalence and incidence of HIV-infected patients, the incidence of AIDS-related Burkitt’s lymphoma has also increased [23,25]. The ovary is a relatively rare site of disease in Burkitt’s lymphomas, compared to the mesentery which is the most common site for this form of lymphoma. In the case described by Crawshaw et al [34] the tumor had extensive growth during the ten days between discovery and diagnosis. This rapid growth aspect is very important since ovarian cancer generally does not exhibit this type of growth; on the other hand, germ cell tumors can present this particular aspect. Lymphoma also manages to double its mass in a very short time.
This article is of fundamental importance especially for the field of radiodiagnostics, being a case report that highlights the radiological figures of an ovarian extranodal Burkitt-type NonHodgkin lymphoma.
Furthermore, Crawshaw uses the criteria described by Fox et al [35] for the diagnosis of primary lymphoma. The proposed criteria are basically three:
- The lymphoma at the time of diagnosis is clinically confined to the ovary only and a thorough observation does not reveal the presence of lymphoma in other sites of the body. Lymphoma can be considered primary even if there is visible diffusion to adjacent lymph nodes or infiltrative propagation into adjacent tissues;
- Peripheral blood and bone marrow do not contain abnormal cells;
- If the lymphomatous lesions appear in sites distant from the ovary, several months must have elapsed between the single ovarian manifestations and subsequent extranodal involvement.
These criteria appear to be in agreement with those already presented years earlier by authors such as Talerman and Palagadu [28,27].
As we mentioned before, it is important not only to differentiate lymphoma from ovarian cancer, but also to recognize whether the lymphoma is primary or secondary, especially for prognostic and therapeutic purposes. The above criteria help differentiate a primary lymphoma from a disseminated lymphoma, while other characteristics can help differentiate lymphoma from ovarian cancer.
In the case of the patient suffering from ovarian Burkitt lymphoma, many signs such as the elevation of tumor markers and the presence of ascites could confuse the specialist in a first clinical diagnosis. Other figures that are present above all in ovarian cancer, but which in many cases can also appear in lymphoma are: omental involvement as we have seen in the above case of B-cell lymphoma and a pleural effusion.
Crawshaw emphasizes the need for specialists to avoid definitive diagnoses of the presenting mass, particularly if they are in the presence of unusual images. In this case the exploratory laparotomy would have been inappropriate as there was a certain diagnosis after the needle biopsy.
Biopsy certainly represents the gold standard for identifying the nature of the mass. MRI appears to be the best diagnostic tool in characterizing lesions, compared to the sole use of ultrasound. Overall, MRI is better than ultrasound because it is able to differentiate the solid forms from the fluid components of cystic complexes, and it is also able to identify the organ of origin. In this case the MRI confirms that the lesions are solid and bilateral.
Due to the rapid growth of the tumor in this case the main differential diagnosis is between a lymphoma and a germ cell tumor or a granulocytic sarcoma. Tumor markers such as AFP and β-HCG are generally not elevated in immature germ cell tumor. Granulocytic sarcoma is a mass of malignant precursor cells of the myeloid lineage found in an extramedullary site, and has a low probability of being bilateral.
Other types of ovarian-only tumors such as fibroma, thecoma and Brenner cell tumor were excluded due to the rapidity of tumor growth. No areas of fibrosis appear on MRI to suggest a diagnosis of fibroma or thecoma. Brenner cell tumors are frequently small, rarely bilateral, and show areas of extensive calcification. Furthermore, malignant epithelial ovarian cancers are only rarely solid. It is equally important to know that a small amount of ascites and the concomitant increase in the CA-125 marker are not specific indicators for the diagnosis of epithelial ovarian cancer.
Nongerminal gonadal tumors such as granulosa cell tumors and Leydig and Sertoli cell tumors are often functional. Ovarian metastases should be taken into consideration in the differential diagnosis, occurring in approximately 30% of malignant diseases affecting the ovary; on the other hand, in the case described above there were no metastatic extraovarian lesions.
Metastases can appear solid, cystic and bilateral on MRI and these characteristics depend on the primary tumor. In essence, ovarian Burkitt lymphoma has a characteristic that it shares with other types of lymphoma but substantially differentiates it from other ovarian solid tumors and that is that of having rapid growth. Imaging techniques show solid lesions with preservation of follicles at the periphery of the ovary.
The importance of considering lymphoma in the differential diagnosis is that the prognosis and treatment in these patients is different compared to other forms of ovarian tumors, given that the primary choice in ovarian lymphoma is chemotherapy.
The aim of obtaining a certain diagnosis through the use of imaging techniques, integrated with biopsy and immunohistochemical examination is to avoid unnecessary and extensive surgery in very young patients. Another author who described the figures that appear on imaging in the case of lymphoma with ovarian localization is Mitsumori [6] in fact reports the case of a 12-year-old girl suffering from primary ovarian lymphoma, accurately describing the images provided by the MRI (Figures 11-13).
The T2-weighted image highlights a solid mass with an intermediate signal intensity and a hyperintensity of the septal structures. When gadopentetate dimeglumine is administered intravenously, T1-weighted images reveal marked enlargement of the septa.Numerous small, regular-walled cysts are visible at the periphery of the tumor. In the contralateral ovary, three nonconnected nodules are evident on a T2-weighted image.
These nodules show the same signal intensity as the tumor mass. A needle aspiration biopsy reveals the presence of B-cell non-Hodgking lymphoma. There are three characteristic images in this case:
1) septal structures are hyperintense on T2-weighted images.
2) the periphery of the tumor is delimited by regularly arranged cysts of small size, of uniform volume and with smooth walls (presumably these are ovarian follicles).
3) three independent nodules are present in the contralateral ovary.
The septa that form at the base of the interstitial structures of the ovary, in step with tumor growth, appear hypointense on T2-weighted images, given that they contain fibrous tissue. In this case, however, the septae most likely appear hypointense due to a decrease in fibrous tissue and the presence of edema. The cortical structure of the ovary appears well preserved after surgical resection carried out following chemotherapy. At the basis of these pathological figures Mitsumori believes that the small regularly shaped cysts observed peripherally are the ovarian follicles of the cortex.
In the process of tumor growth, in fact, the lymphoma tends to invade the ovary, preserving its normal structure. In fact, as we will see later, cystic areas are characteristic of other types of ovarian tumors, such as metastases from a colorectal neoplasm. Mitsumori then underlines how the cysts found represent ovarian follicles. It is extremely rare to see more than one solid tumor in the same ovary on MRI.
Hattori [64] previously described a case of lymphoma with the description of two solid nodules in the same ovary. The author concludes by identifying MRI as a useful tool in the diagnosis of ovarian lymphoma, particularly useful for specialists in trying to make a first differential diagnosis between cancer and lymphoma.

Figure 11: Sagittal T2-weighted MRI image shows that the tumor has intermediate signal intensity (open arrows) and there are hyperintense septal structures within the tumor (arrowheads). In the contralateral ovary there are three disconnected nodules (black arrows).
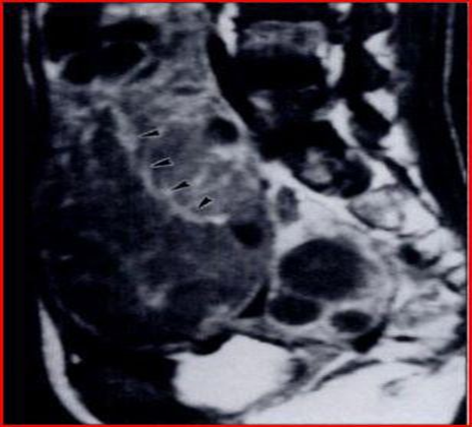
Figure 12: Sagittal T1-weighted MRI image, septa show increased signal intensity after administration of gadopentetate dimeglumine (arrowheads).
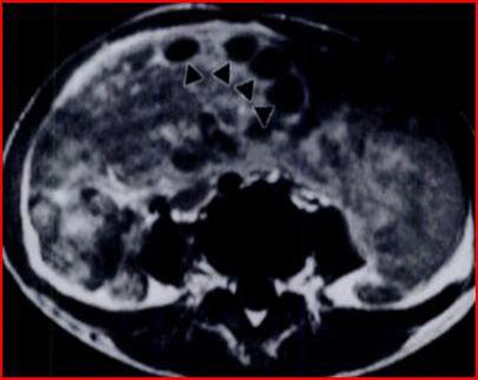
Figure 13: Axial T1-weighted MRI images with gadopentetate dimeglumine administration show many small, uniformly sized, smooth-walled cysts at the periphery of the mass (arrowheads).
Ferrozzi [32] also reports results very similar to those of Mitsumori in the article concerning the use of MRI in the diagnosis of ovarian lymphomas. In fact, examining five women affected by ovarian lymphoma aged between 14 and 70 years, among which there is a case of primary ovarian lymphoma, a case of ovarian lymphoma which presents 30 months after a surgical resection of a primary uterine lymphoma and the remaining represented by secondary ovarian lymphoma. All patients present with large B-cell lymphoma. The results obtained demonstrate that three cases present bilateral involvement, with an average volume of the tumor mass of around 7.9 cm.
All lesions appear homogeneous with a low signal intensity on T1-weighted images and an intermediate-high intensity on T2weighted images. Furthermore, after administration of Gadolino the images show a moderate increase in heterogeneity. In conclusion, Ferrozzi [35] maintains that the diagnosis of an ovarian lymphoma should be considered in the presence of bilateral involvement, with the presence of solid and homogeneous masses (with low signal on T1 and moderately high on T2), without areas of necrosis, calcification or hemorrhagic lesions and with moderate increase in contrast enhancement.
In fact, the author identifies the presence of necrotic or hemorrhagic areas as a fundamental point for the differential diagnosis with other types of neoplasms that can affect the ovary both primarily and secondarily. But in some cases of lymphoma, as we will see in our experience, these characteristics may appear.
Correct diagnoses that avoid surgery
There are rare cases in the literature describing ovarian lymphoma which, although mimicking ovarian cancer, are diagnosed preventively, avoiding surgery. This aspect is well highlighted by Cyriac et al [11] who described the presence of Burkitt’s lymphoma in a 13-year-old patient, who, thanks to the use of CT, which highlighted the bilateral solid masses with peritoneal and omental deposits and the subsequent biopsy which detected positivity for CD45, CD20, CD10 and CD79 (Figure14), she was subjected to the LMB 89 therapeutic protocol obtaining a complete remission of the masses and remaining stable in the following 6 months of follow-up -up. Given the young age of the patient, this case highlights how chemotherapy treatment of lymphoma alone can avoid radical surgery. Another example of correct diagnosis is reported by Yamada [35], who describes a case of ovarian malignant lymphoma manifesting as advanced ovarian cancer.
In fact, the patient, a 47-year-old woman, presents with signs and symptoms suggestive of advanced ovarian cancer, as imaging tests such as ultrasonography and MRI highlight a picture that differs from the criteria highlighted by Crawshow [6] and by Ferrozzi [30]. Radiodiagnostic tools show a bilateral abdominal tumor measuring 10 cm, with omental involvement and abundant presence of ascitic fluid, which may be indicative of ovarian cancer, but cannot exclude possible lymphoma. There is no evidence of lymph node involvement. Blood markers like CA-125, LDH are elevated, which increases the belief that it may be ovarian cancer.
The patient underwent exploratory laparotomy, which highlighted the ascitic fluid, 2,500 ml, the tumor masses extending to the fallopian tubes, the peritoneal involvement and the absence of involvement of the liver and spleen. Peritoneal washing and drainage of the cavity are then carried out. The definitive immunohistochemical diagnosis reveals the presence of a diffuse large B-cell lymphoma at stage IV according to the Ann Arbor classification and stage IIIc according to the International Federation of Gynecology and Obstetrics. The treatment consists of the administration of 8 cycles of CHOP. At the end of the treatment the MRI reveals the disappearance of the ovarian masses and omental involvement. The authors underline the importance of considering ovarian lymphoma when faced with cases of this type, administering an appropriate chemotherapy regimen for the different histological types of lymphoma.
Below are the laparoscopic and MRI images (Figures 15 and 16).
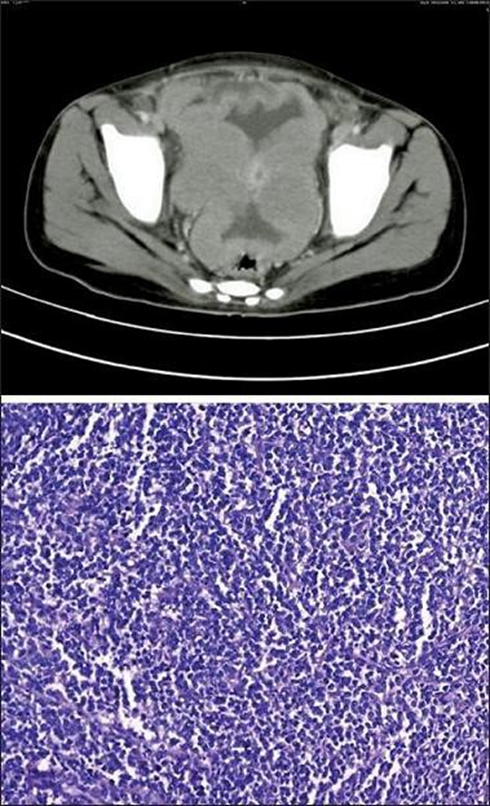
Figure 14: The CT image highlights two solid and bilateral ovarian masses, with the presence of omental deposits and peritoneal implants. The immunohistochemical image obtained after biopsy highlights a proliferation of atypical lymphoid cells with little cytoplasm, nuclei with aggregated chromatin and many small nucleoli showing a high mitotic count.
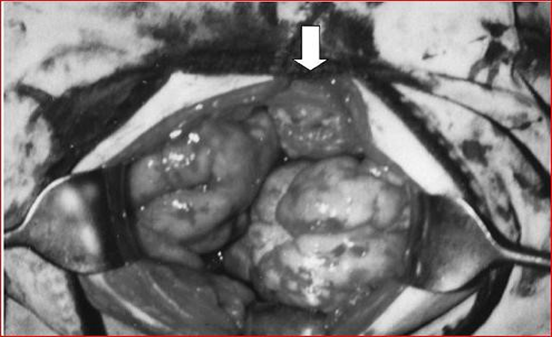
Figure 15: The image shows bilateral tumor masses and omental enlargement.

Figure 16: The image highlights bilateral multi-nodular masses and some omental tumor involvement (arrows), which is visible in the lower abdominal cavity.
Cases treated with immediate surgery
On the other hand, the literature reports cases of ovarian Burkitt lymphoma that were treated immediately by surgery, precisely because the diagnosis of lymphoma was not suspected. This is the case described in Szu-Ching Lu et al [10] who describe the appearance of ovarian Burkitt’s lymphoma in a 50-year-old woman. Unfortunately, the woman does not present with the common systemic symptoms of lymphoma such as fever, night sweats, nausea, vomiting or bladder symptoms. His Pap test was normal and on physical examination, as in the cases described previously, a pelvic mass of the size of approximately 20 weeks of gestation was revealed. The high resolution trans-vaginal ultrasound examination revealed a large and homogeneous abdominal mass measuring 10.8 x 8.7 cm extending from the uterus to the left ovary and the presence of a minimal content of free liquid (Figure17-18 ). Power-Doppler ultrasound showed no vascularity in the mass. All blood tests, including tumor markers, were normal before surgery.
Initially, the presence of a uterine subserous myoma or a tumor of ovarian origin was therefore suspected, without taking into consideration a hypothetical diagnosis of lymphoma. The patient, given the tests previously carried out, underwent an exploratory laparotomy, which revealed the presence of a yellowish ovarian tumor mass measuring 15 x 15 cm, with a uterine adhesion. An involvement of the cecal area is also highlighted. Initial frozen section analysis showed a malignant ovarian neoplasm of stromal origin. The patient is then subjected to a total hysterectomy, with a bilateral salpingo-oophorectomy, omentectomy, excision of the tumor at the peritoneal level, hemicolectomy plus sampling of the para-aortic lymph nodes.
The final diagnosis instead reveals the presence of Burkitt’s lymphoma, with bilateral involvement of the ovary, cervical, terminal ileum, ascending colon and peritoneal cavity. All dissected lymph nodes were negative for tumor metastasis. The tumor cells showed positivity for LCA, CD20, CD10, Bcl-6. Furthermore, IgG for Epstein-Barr virus was positive. The patient was invited to a medical oncology department for further chemotherapy treatment.

Figure 17: Trans-abdominal ultrasound showing a large irregularly shaped echogenic pelvic mass. The mass measures 10.8 x 8.7 cm.
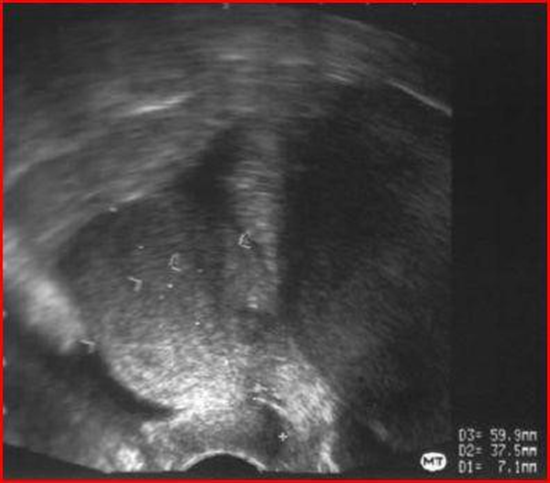
Figure 18: Trans vaginal ultrasound showing a large pelvic mass, extending from the right anterior wall of the uterus, with homogeneous echogenicity and some small anechoic areas within the mass.
For prognostic and treatment purposes, as we have observed, it is necessary to differentiate ovarian lymphoma whether secondary or primary from an ovarian neoplasm. As Ray [36] reports, describing a clinical case of an 8-year-old girl affected by primary ovarian diffuse large B-cell lymphoma which presents as a bilateral ovarian mass.
Thanks to the use of ultrasound, the highlighted mass appears heterogeneous and overall solid with some cysts and measures 10 x 5.2 x 3.5 cm on the right and 9.2 x 4.8 x 3.0 on the left. As in the previous case, the presenting symptoms are similar with discomfort and abdominal swelling, on objective examination the abdomen appears of a pasty consistency but with the absence of free liquid. During the exploratory laparotomy it is observed that there is no longer a free ovarian mass and the tumor appears whitish-grey, homogeneous and solid.
A total hysterectomy is then performed accompanied by a bilateral salpingo-oophorectomy. On the basis of the histochemical examination, the presence of cells positive for LCA and for the B cell line marker CD20 is detected. The author highlights how a malignant lymphoma can be confused with another primary ovarian tumor.
However, it should be noted that infiltration of the adjacent fallopian tube and/or broad ligament is generally more common in lymphomas than in other tumors included in the differential diagnosis. For example, dysgerminoma may be indistinguishable on initial gross observation from malignant lymphoma. On the other hand, however, only 10% of dysgerminomas have bilateral presentations compared to 50% of malignant lymphomas.
It is also interesting to observe the MRI images obtained by Weingertner et al [37] which differ slightly from the usual images previously described by Ferrozzi and Mitsumori, regarding the ovarian localization of non-Hodgkin’s lymphoma (Figures 19-21).
In fact, Weingertner describes a case of ovarian lymphoma that mimics a metastatic ovarian tumor. In fact, the patient, in addition to presenting an elevation of tumor markers such as CA125 which are generally used as a warning light for ovarian cancer, did not present any typical symptoms of lymphoma, such as fever or night sweats. It has a pelvic mass measuring 8 x 11 x 15 cm.
However, the author tends to point out that even the cold section carried out during an exploratory laparotomy was difficult to analyse, orienting the diagnosis towards an undifferentiated carcinoma. A total salpingo-oophorectomy is then performed with removal of the uterus and involved peritoneum.
Surgery is carried out in the first instance precisely because the diagnosis of lymphoma had not been taken into consideration. The final immunohistochemical diagnosis, however, revealed a diffuse large B-cell lymphoma, with positivity also in the bone marrow. The stage assigned to the patient is IV according to the Ann Arbor classification. Subsequently the patient is subjected to ACVBP (a combination of adriamycin, cyclophosphamide, vindesine, bleiomycin and prednisone), plus intrathecal administration of methotrexate to prevent meningeal spread. The use of methotrexate in the treatment of ovarian lymphoma is also cited by Yildirim et al, in a patient suffering from juvenile rheumatoid arthritis, affected by ovarian diffuse large B-cell lymphoma [13].
A few months later the patient presents splenomegaly and for this reason a splenectomy is performed with a liver biopsy which detects the presence of follicular lymphoma with large and small cells. Subsequently, the patient achieved complete remission after four cycles of IVAM (ifosfamide, vepeside, aracytin, methotrexate and folic acid) with the administration of monoclonal antibodies. The author tends to underline how lymphoma with ovarian localization can be treated with chemotherapy alone, as described by Dimopoulos [38] who in a retrospective study demonstrates the possibility of chemotherapy alone in a cluster of patients suffering from ovarian lymphoma.
Obviously each histological type has its own chemotherapy treatment. The author concludes by saying that, even if there are rare sources in the literature describing cases of ovarian lymphoma treated with chemotherapy alone, radical surgery in these patients does not seem to be associated with a good prognosis.
On the other hand, the combination of biopsy and chemotherapy seems to be the most pertinent choice in the management of these patients. In the presence of some clinical and radiological signs, surgeons and pathologists should consider the diagnosis of ovarian lymphoma, to outline the optimal treatment, avoiding mutilating surgery, and consequently preserve the quality of life of the affected patients [40,27,23,39].
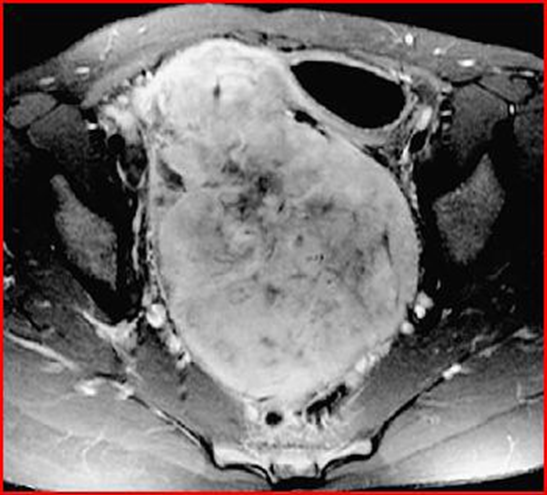
Figure 19: Transverse MRI image showing a solid and heterogeneous pelvic mass, with a necrotic center. The volume of the mass is 8 x 11 x 15 cm.
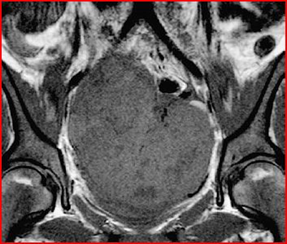
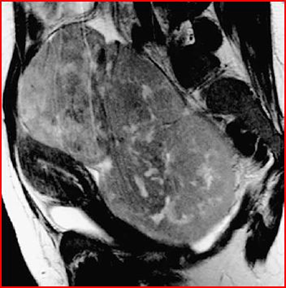
Figure 21: Sagittal MRI image, showing compression of the bladder, uterus and urinary tract.
Martin et al [41] in a 2008 article, also reported the presence of an ovarian Burkitt’s lymphoma mimicking a primary gynecological tumor in a 30-year-old woman. As we see in the images, the patient has a mass in the right ovary and a second mass fixed to the uterine fundus (Figures 22,23).
Imaging techniques reveal a pelvic situation very similar to the case reported by Su-Ching Lu with ovarian and uterine involvement. Here too, the diagnosis of lymphoma is not hypothesized, therefore the patient is subjected to surgery and a certain diagnosis is obtained only after immunohistochemical analysis.
The author emphasizes that there are no specific images that can differentiate Burkitt’s lymphoma from other solid tumors. The patient is subsequently treated with a chemotherapy regimen. (Table 2)Treatment for Burkitt lymphoma is a combination of chemotherapy. This type of chemotherapy regimen alone is effective in 90% of patients with low-grade lymphoma and in 60- 80% of patients with advanced disease.

Figure 22: Trans vaginal ultrasound identifying a mass in the right ovary, measuring 71.66 mm.
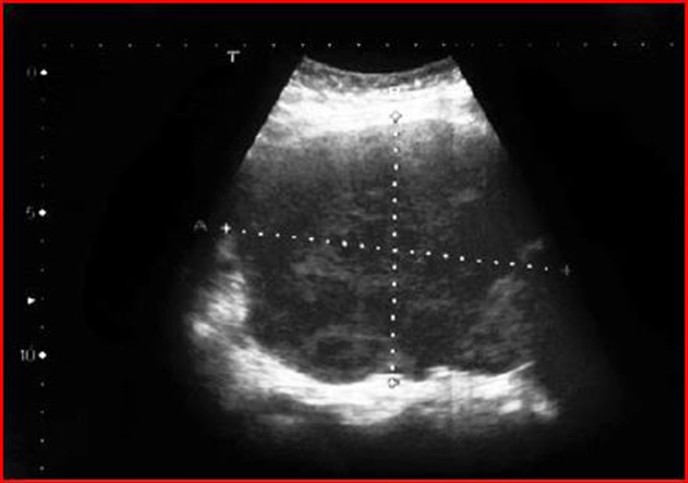
Figure 23: Trans vaginal ultrasound showing a mass adherent to the uterine fundus.
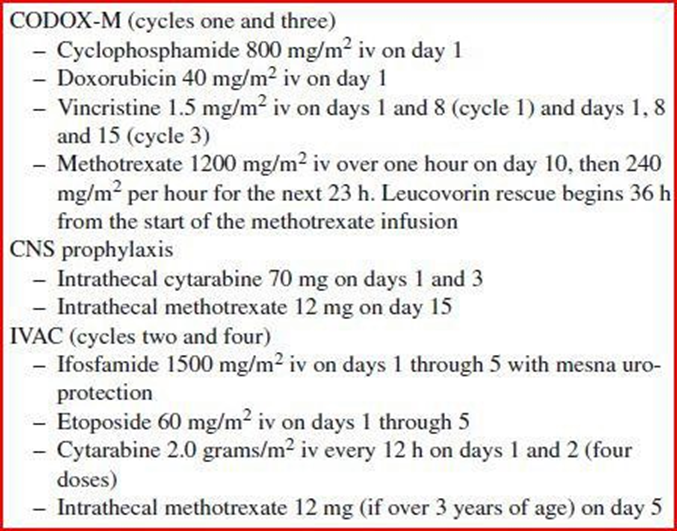
Table 2: CODOX-M-IVAC: The CODOX-M-IVAC therapeutic regimen is composed of four cycles. Cycles one and three are CODOX-M, while cycles two and four are IVAC.
Conclusion
It is evident that the primary differential diagnosis between ovarian masses is extremely difficult. The gold standard is obviously represented by the biopsy, the last step in the chain of clinical procedures, essential for a certain diagnosis. On the other hand, however, to avoid a destructive surgical treatment, in patients suffering from ovarian lymphoma, the specialist can carefully orient the differential diagnosis by keeping in mind some aspects that appear on imaging.
At the same time, we remember that the radiological characteristics, which can be highlighted through the use of means such as ultrasound, CT and MRI, cannot be considered as points of absolute certainty for the diagnosis of ovarian lymphoma. The specialist must pay attention to some fundamental anamnestic data regarding the clinical history of the patients, such as a previous history of lymphomatous disease, which can help in directing the diagnosis towards the presence of ovarian lymphoma. It is equally true that from the literature review it emerges that some parameters that can lead to the diagnosis of advanced stage ovarian epithelial cancer, such as the elevation of the CA-125 marker, the presence of ascitic fluid, and peritoneal implants, can also be present in case of ovarian lymphoma. Precisely for this reason we have focused our research on the role of diagnostic imaging in being able to discriminate as precisely as possible the morphological differences that appear between a lymphoma located in the ovary and its tumor counterpart.
We remind you that the incidence of lymphomas with extranodal localization, in our specific case, with ovarian involvement, has increased in the last two decades. The point of greatest importance, as we have underlined several times during the discussion, is the possible difference in treatment between ovarian lymphoma and ovarian cancer. In fact, through studies carried out recently it has been seen that ovarian lymphoma, especially that with primary localization, is very chemo-sensitive. Primary chemotherapy therapy can be of fundamental importance in women of young age or those wishing to become pregnant, as it would avoid the use of mutilating surgery. Finally, it is useful to remember that studies are underway on the use of Whole-Body Diffusion Magnetic Resonance (DWI) as an alternative tool to PET/ CT in the staging and follow-up of patients affected by malignant lymphoma [52]. This method appears promising as, in addition to being valid for all types of malignant lymphoma (even low-grade ones), it is characterized by the intrinsic advantage of not using ionizing radiation, which is however harmful to the patient.
References
- C M Bacon (2009) Extranodal lymphoma. Diagnostic Histopathology 16: 82-98.
- S C Chua; F I Rozalli; S R O’Connor (2009) Imaging features of primary extranodal lymphoma 64: 574-588.
- W-K Lee; E W F Lau; A Stanley; Y Y Ho (2008) Abdominal manifestation of extranodal lymphoma:Spectrum of imaging findings 191: 198-206.
- A T Ilica; K Kocacelebi; R Savas; A Ayan (2011) Imaging of extranodal lymphoma with PET/CT 36:127-138.
- Jiulian A Crasta ; Elizabeth Vallikad (2009) Ovarian Lymphoma .Indian Journal of Medical Paediatric Oncology 1: 28-30.
- J Crawshaw; S A Sohaib; A Wotherspoon; J A Shepherd (2007) Primay non-Hodgkin’s lymphoma of the ovaries:imaging findings .British Journal of Radiology 80: 155-158.
- Szu-Ching Lu; Wan-Lin Shen; Ya-Min Cheng; Cheng-Yang Chou; PoLing Kuo (2006) Burkitt’s Lymphoma Mimiking a Primary Gynecologic Tumor .Taiwainese J Gynecol 45.
- T Elharroudi; N Ismaili; H Errihani; A Jalil (2011) Primary lymphoma of the ovary .Cancer Journal 4: 195-196.
- I Bambury; G Wharfe; H Fletcher; E Williams; J Jaggon (2011) Ovarian Lymphoma .J Obstet Gynaecol 31: 617-639.
- S Cyriac; L Srinivas; V Mahajan; S Sundersingh; S Sagar (2010) Primary Burkitt’s Lymphoma of the ovary .Afr J Pediatric Surg 7.
- M Hatami; K Whitney; G L, Goldberg (2010) Primary bilteral ovarian and uterine Burkitt’s lymphoma following chemotherapy for breast cancer .Ginecology Oncology 281: 697-702.
- R Anand; M Markman (2011) Eleveted Serum CA-125 in a patient with follicular lymphoma and history of ovarian cancer. Cancer Treatment Centers of America, Philadelphia 4: 172-174.
- S Nakamura; M Kat; K Ichimura; Y Yatabe; Y, Kagami, et al. (2001) Peripheral T/natural killer-cell lymphoma involving the female genital tract:a clinicopathologic study of 5 cases .Int J Hematol 73: 108-114.
- R Vang; L J Medeiros; R A Warnke; J P Higgins; M T Deavers (2001) Ovarian Non-Hodgkin’s lymphoma: A clinicopathologic study of eight pimary cases Mod Pathol 14: 1093-1099.
- K G, Koffi; E, N’Dathz; A, Tolo; N, Meite; R, Ayemou; P, Kouehion; I, Sanogo2, 2010, Cahiers Santè, Vol. 20.Lacalisations exceptionnelles du lymphome endemique de Burkitt (a propos de 21 cas vus en Cote d’Ivoire.)
- N Ozsan; BJ Bedke; ME Law; DJ Ineards; RP Ketterling, et al. (2011) Clinoparhologic and genetic characterization of follicular lymphomas presenting in the ovary reveals 2 distinct subgroups .Am J Surg Pathol 35: 1691-1699.
- AL Chong; BY Ngan; S Weitzman; O Abla (2009) Anaplastic large cell lymphoma of the ovary in a pediatric patient .J Pediatr Hematol Oncol 31: 702-704.
- N Sakurai; K Tateoka; J Taguchi; T Terada (2008) Primary precursor B-cell lymphoblastic lymphoma of the ovary: a case report anh review of the literature, Int J Gynecol Pathol 27: 412-417.
- N Niitsu; H Nakamine; M Hayama; Y Unno; S Nakamura, et al. (2002) Ovarian follicular lymphoma:a case report and a review of the literature.) Ann Hematol 81: 654-658.
- D N Lanjewar; D D Dongaonkar (2006) HIV-associated primary Non-Hodgkin’s lymphoma of the ovary: a case report .Gynecologic Oncology 102: 590-592.
- L Guterrez-Garcia; N Medina-Ramos; R Garcia-Rodriguez; MA Barber; MD Arias, et al. (2009) Bilateral ovarian Burkitt’s lymphoma .Eur J Gynecol Oncol, 30: 231-233.
- PS Govender; M Moodley (2010) Primary Non-Hodgkin’s lymphoma of the ovary in the background of human immunodeficiency virus (HIV): a bold and curative approach to treatment .Eur J Gynaecol Oncol 31: 102-104.
- G Skodras; V Fields; PJ Kragel (1994) Ovarian lymphoma and serous carcinoma of low malignant potential arising in the same ovary:a cae report with review of literature of 14 primary pvarian lymphoma 118: 647-650.
- A Talerman, Path FRC (2002) Non specific tumors of the ovary, including mesenchymal tumors and malignant lymphoma. Blaustein’s Pathology of the Female Genital Tract Chapter. p.1035-1362.
- RR Palagadu; RM Bearmen; H Rappaport; H Fox Malignant lymphoma with primary manifestation in the gonad: a clinicopathological study of 38 patients 45: 561-571.
- X-Y Zhao; X-N Hong; J-N Cao; S-J Leaw; Y, Guo, et al. (2011) Clinical features and treatment autcomes of 14 cases of primary ovarian Non-Hodgkin’s lymphoma:a single-center experience .Med Oncol 28 :1559-1564.
- F Ferrozzi; C Catanese; M Uccelli; P Bassi (1998) Ovarian Lymphoma. Findings with ultrasonography, computerized tomography and magnetic resonance .Radiol Med 95 :493-497.
- F Ferrozzi; G Tognini e G, Zuccoli (2000) Non-Hodgkin lymphomas of the ovaries: MR finding .J Comput Assist Tomogr 24 :416-420.
- H Fox; FA Langley; ADT Govan; AS Hill; MH Bennet (1998) Malignant lymphoma presenting as an ovarian tumor:a clinicopathological analysis of 34 cases., Br J Obstet Gynecol 95 :386-390.
- G I Onimoe; S Kahwash; A Termuhlen; T G Gross; E Varga, et al. (2011) Bilateral Burkitt lymphoma of the ovaries: A report case in a child with Williams Syndrome. Tho Ohio State University, Columbus USA .Case Report Med EPub 2011 :1-4.
- T Yamada; N Iwao; H Kasamatsu; H Mori (2003) A case of malignant lymphoma of the ovary manifesting like an advanced ovarian cancer .Gynecologic Oncology 90 :215-219.
- S Ray; MG Mallick; PB Pal; MK Choudhury; A Bandopadadhyay, et al. (2008) Extranodal non-Hodgkin’s lymphoma presenting as an ovarian tumor. Indian J Pathol Microbiol 51 :528-530.
- A S, Weingertner; M N Roedlich; D Hamid; J J Baldauf (2004) NonHodgkin malignant lymphoma revealed by an ovarian tumor: a case report and review of the literature .Gynecologic Oncology 95 :750-754.
- M A Dimopoulos; D Daliani; W Pugh; D Gershenson; F Cabanillas (1997) Primary ovarian Non-Hodgkin’s lymphoma:outcome after treatment with combination chemotherapy. Gynecologic Oncology 64 :446-450.
- M Signorelli; A Maneo; S Cammarota; G Isimbaldi; R G Parra, et al. (2007) Conservative mamagement in primary genital lymphomas: the role of chemotherapy. Gynecology Oncology 104 :416-421.
- J Yun; S J Kim; J H Won; C W Choi; H S Eom, et al. (2010) Clinical features and prognostic relevance of ovarian involvment in NonHodgkin’s lymphoma: a consortium for improving survival of lymphoma (CISL) report. Leukemia Research 34 :1175-1179.
- A Martin; R Fernandez; M Beneitez; V Marin; I Rodas, et al. (2008) Primary ovarian Burkitt lymphoma. Clin Transl Oncol 10 :673-675.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.