Osteoporosis Prevention Fracture: Review and Update on Screening Recommendations by the United States Preventive Services Task Force
by Cameron Y. S. Lee1,2*
1Private Practice in Oral, Maxillofacial and Reconstructive Surgery. Aiea, Hawaii. 96701, USA
2The University of Chicago. Graham School. Chicago, Il 60637, USA
*Corresponding author: Cameron Y. S. Lee, Private Practice in Oral, Maxillofacial and Reconstructive Surgery. Aiea, Hawaii. 96701, USA
Received Date: 08 September, 2025
Accepted Date: 15 September, 2025
Published Date: 18 September, 2025
Citation: Lee CYS (2025) Osteoporosis Prevention Fracture: Review and Update on Screening Recommendations by the United States Preventive Services Task Force. J Community Med Public Health 9: 533. https://doi.org/10.29011/2577-2228.100533
Abstract
Primary osteoporosis is a skeletal disorder characterized by decreased bone mass leading to increased bone fragility, increased fracture risk, morbidity, and mortality. Osteoporosis is a common medical condition, affecting more than 10 million Americans. Another 43.3 million people have low bone mass associated with a considerable risk for progression to osteoporosis. Post-menopausal women are at greatest risk for developing osteoporosis. This paper is a review about osteoporosis, and an update on the screening recommendations by the United States Preventive Services Task Force (USPSTF) to prevent osteoporotic fracture.
Keywords: Osteoporosis; USPSTF screening recommendations; DXA; Fracture; FRAX
Introduction
Primary osteoporosis is a skeletal disorder characterized by decreased bone mass leading to increased bone fragility, increased fracture risk, morbidity, and mortality [1-3]. This condition often does not cause symptoms, and many people with osteoporosis may not be aware that they have this medical condition [4]. Osteoporosis is a common medical condition, affecting more than 10 million Americans. Another 43.3 million people have low bone mass associated with a considerable risk for progression to osteoporosis [5]. Due to a deficiency in the hormone estrogen, post-menopausal women are at greatest risk for developing osteoporosis [6]. Other risk factors include underweight individuals, medications (corticosteroids, insulin dependent diabetes mellitus), cigarette smoking, excess alcohol consumption, and a family history of osteoporosis.
Osteoporotic fractures can occur in any bones of the skeleton, but the risk for fracture is greatest in the hip and spine that leads to pain, disability, loss of independence, and even death [3,7]. Men and young individuals are less affected by this medical condition.
However, men with osteoporotic hip fractures have greater morbidity and mortality than women and seek medical treatment less than women [8-10]. This paper is a review about osteoporosis, and the latest screening recommendations by the United States Preventive Services Task Force (USPSTF) to prevent osteoporotic fracture [7].
In 1994, the World Health Organization defined osteoporosis in post-menopausal White women as bone density at the hip or lumbar spine that is 2.5 standard deviations or lower (T score –2.5) than the mean Bone Mineral Density (BMD) measured at that site for a reference population of young healthy White women [4]. This remains the clinical reference standard for people of all racial and ethnic groups, and for both sexes. However, the prevalence of osteoporosis and incidence of osteoporotic fractures differs among racial and ethnic groups. Prevalence is highest in women, individuals age 65 years or older (27.1% in women and 5.7% in men), compared with men and among Asian, Hispanic, and White persons [11].
Osteoporotic fractures are associated with psychological distress, subsequent fractures, loss of independence, reduced ability to perform activities of daily living, and death. Studies show lower fracture incidence in Asian, Black, and Hispanic populations compared with White populations among both sexes [12,13]. Differences in BMD alone do not completely explain the racial and ethnic differences in fracture incidence. Studies in Asian women have lower BMD than White women, and risk for fracture [14-16]. Although the underlying etiology for the differences in fracture incidence among racial and ethnic groups remain uncertain, this could be due to differences in social and environmental determinants. Although bone density is an important risk factor for fracture (especially fragility fractures), advancing age is a stronger determinant [17]. Further, older adults have much higher fracture rates than younger adults with the same BMD due to declining bone quality and from falling [1-3].
Treatment
Although this review is not about the treatment to prevent fractures from osteoporosis, the United States Food and Drug Administration has approved several drug therapies for the prevention of osteoporosis [3,18]. Therapies include the following: receptor activator of nuclear factor κB (RANK) ligand inhibitor (denosumab), bisphosphonates (alendronate, ibandronate, risedronate, zoledronate), selective estrogen receptor modulators (SERMs) (bazedoxifene, raloxifene), a sclerostin inhibitor (romosozumab), recombinant human parathyroid hormone (recombinant PTH) (teriparatide), analogue of human parathyroid hormone–related protein (PTHrP) (abaloparatide).
Screening Tests for Osteoporosis
To prevent osteoporotic fractures in women under 65 years old and who are at risk for fracture, screening for osteoporosis is recommended. For women over 65 years old, screening for osteoporosis is also recommended to prevent osteoporotic fractures. For men of all ages the risk for osteoporotic fracture is unknown and therefore, screening for osteoporotic fracture is not indicated (Figure 1).
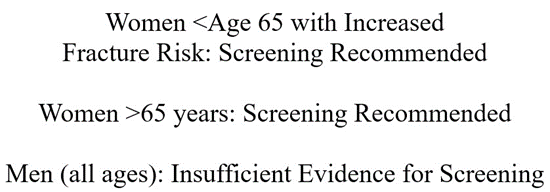
Figure 1: Screening Recommendations to Prevent Osteoporotic Fracture.
The most common bone measurement test to screen for osteoporosis is Dual-energy X-ray Absorptiometry (DXA) at a central site such as the hip, femoral neck, or lumbar spine [17,19]. Centrally measured DXA correlates with bone strength and clinical fracture outcomes. Fracture risk at a specific site is best predicted if bone density is measured at that site. However, clinical evidence suggests that BMD alone may not be the most useful predictor of fracture risk, especially in younger populations [20]. Several risk assessment tools that incorporate age and sex, with or without other risk factors have been developed to either identify probability of osteoporosis or predict fracture risk.
A risk assessment tool that is frequently used with BMD studies is the fracture risk assessment tool (FRAX) [21]. FRAX predicts the 10-year probability of hip fracture for people aged 40 to 90 years by using demographic and clinical factors alone or in combination with BMD measured at the femoral neck [21-23]. In the United States, four different versions of FRAX using racial and ethnic specific fracture incidence data are available for Hispanic, nonHispanic Asian, non-Hispanic Black, and non-Hispanic White persons [21]. As hip fracture incidence in the United States is lower in most non-White racial ethnic groups, fracture risk estimates for Asian, Black, and Hispanic people will be lower than White people of the same age, sex, weight, BMD in the FRAX model. However, for multi-racial individuals, there is no consensus as to which FRAX version to use [24].
Conclusion
The United States Preventive Services Task Force has determined that screening for women over age 65 has moderate benefit. For women 65 years or younger at increased risk for osteoporotic fractures, screening is recommended. For men of all ages, there is insufficient evidence to recommend screening for osteoporosis to prevent osteoporotic fractures.
References
- Rizkallah M, Bachour F, Khoury ME, Sebaaly A, Finianos B, et al. (2020) Comparison of morbidity and mortality of hip and vertebral fragility fractures: Which one has the highest burden? Osteoporos Sarcopenia 6: 146-150.
- Crandall CJ, Hunt RP, LaCroix AZ, Robbins JA, Wactawski-Wende J, et al. (2021) After the initial fracture in postmenopausal women, where do subsequent fractures occur? EClinicalMedicine 35: 100826.
- Qaseem A, Hicks LA, Etxeandia-Ikobaltzeta I, Shamliyan T, Cooney TG, et al. (2023) Pharmacologic Treatment of Primary Osteoporosis or Low Bone Mass to Prevent Fractures in Adults: A Living Clinical Guideline From the American College of Physicians. Ann Intern Med 176: 224-238.
- (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser 843: 1-129.
- Sarafrazi N, Wambogo EA, Shepherd JA (2021) Osteoporosis or Low Bone Mass in Older Adults: United States, 2017-2018. NCHS Data Brief 1-8.
- Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, et al. (2020) The epidemiology of osteoporosis. Br Med Bull 133: 105-117.
- Kahwati LC, Kistler CE, Booth G, Sathe N, Gordon R, et al. (2025) Screening for Osteoporosis to Prevent Fractures: An Evidence Review for the US Preventive Services Task Force. Evidence Synthesis No. 238. Agency for Healthcare Research and Quality. AHRQ publication 23-05312-EF-1.
- Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39: 203-209.
- Herrera A, Lobo-Escolar A, Mateo J, Gil J, Ibarz E, et al. (2012) Male osteoporosis: a review. World J Orthop 3: 223-234.
- Riska BSL, Forsén L, Omsland TK, Søgaard AJ, Meyer HE, et al. (2018) Does the association of comorbidity with 1-year mortality after hip fracture differ according to gender? The Norwegian Epidemiologic Osteoporosis Studies (NOREPOS). J Am Geriatr Soc 66: 553-558.
- (2021) QuickStats: Percentage* of Adults Aged ≥50 Years with Osteoporosis,† by Race and Hispanic Origin§ - United States, 20172018. MMWR Morb Mortal Wkly Rep 70: 731.
- Lo JC, Zheng P, Grimsrud CD, Chandra M, Ettinger B, et al. (2014) Racial/ethnic differences in hip and diaphyseal femur fractures. Osteoporos Int 25: 2313-2318.
- Liu LH, Chandra M, Gonzalez JR, Lo JC (2017) Racial and ethnic differences in hip fracture outcomes in men. Am J Manag Care 23: 560-564.
- Walker MD, Babbar R, Opotowsky AR, Rohira A, Nabizadeh F, et al. (2006) A referent bone mineral density database for Chinese American women. Osteoporos Int 17: 878-887.
- Lo JC, Kim S, Chandra M, Ettinger B (2016) Applying ethnic- specific bone mineral density T-scores to Chinese women in the USA. Osteoporos Int 27: 3477-3484.
- Lo JC, Chandra M, Lee C, Darbinian JA, Ramaswamy M, et al. (2020) Bone mineral density in older U.S. Filipino, Chinese, Japanese, and White women. J Am Geriatr Soc 68: 2656-2661.
- Kanis JA, Johnell O, Oden A, Dawson A, De Laet C, et al. (2001) Ten-year probabilities of osteoporotic fractures according to BMD and diagnostic thresholds. Osteoporos Int 12: 989-995.
- Dakkak MA, Banerjee M, White L (2023) Osteoporosis Treatment: Updated Guidelines From ACOG. Am Fam Physician 108: 100-104.
- Ward RJ, Roberts CC, Bencardino JT, Arnold E, Baccei SJ, et al. (2017) ACR Appropriateness Criteria® Osteoporosis and Bone Mineral Density. J Am Coll Radiol 14: S189-S202.
- Sanders KM, Nicholson GC, Watts JJ, Pasco JA, Henry MJ, et al. (2006) Half the burden of fragility fractures in the community occur in women without osteoporosis. When is fracture prevention cost- effective? Bone 38: 694-700.
- Fuggle NR, Curtis EM, Ward KA, Harvey NC, Dennison EM, et al. (2019) Fracture prediction, imaging, and screening in osteoporosis. Nat Rev Endocrinol 15: 535-547.
- Kanis JA (2008) World Health Organization Scientific Group. Assessment of Osteoporosis at the Primary Health Care Level: Technical Report. World Health Organization Collaborating Centre for Metabolic Bone Diseases.
- Kanis JA, Harvey NC, Johansson H, Odén A, Leslie WD, et al. (2017) FRAX Update. J Clin Densitom 20: 360-367.
- Lewiecki EM, Erb SF (2022) Racial disparities and inequalities in the management of patients with osteoporosis. Orthop Nurs 41: 125-134.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.