Non-Alcoholic Wernicke’s encephalopathy in a Young Female with Chronic Nausea and Vomiting
by Abdulkerim Ali*, Shoaib Sheikh, Priya Vijayaragavan
Kings Mill Hospital, Sherwood Forest Hospitals Trust, Nottinghamshire, England, United Kingdom
*Corresponding author: Abdulkerim Ali, Kings Mill Hospital, Sherwood Forest Hospitals Trust, Nottinghamshire, England, United Kingdom
Received Date: 26 August 2025
Accepted Date: 29 August 2025
Published Date: 02 September 2025
Citation: Ali A, Sheikh S, Vijayaragavan P. (2025). Non-Alcoholic Wernicke’s encephalopathy in a Young Female with Chronic Nausea and Vomiting. Ann Case Report. 10: 2396. DOI:10.29011/2574-7754.102396
Abstract
Wernicke’s encephalopathy (WE) is a serious neurological condition caused by thiamine deficiency, most commonly associated with chronic alcohol use. However, it can also occur in non-alcoholic individuals with malnutrition or prolonged vomiting.
This is a case of 30-year-old female patient with a three-month history of nausea, vomiting, and significant weight loss. She developed confusion, visual disturbances, and gait instability.
Blood tests showed multiple nutritional deficiencies electrolyte abnormalities, consequently, MRI brain revealed symmetrical hyperintensities in the thalami, mammillary bodies, and periaqueductal grey matter. These findings, along with clinical features, confirmed a diagnosis of non-alcoholic WE. High-dose intravenous thiamine was initiated promptly, resulting in gradual neurological improvement.
This case underscores the importance of early recognition and treatment of WE in non-alcoholic patients, and timely thiamine administration can prevent irreversible neurological damage and improve outcomes.
Keywords: Non-Alcoholic Wernicke’s encephalopathy; Nausea and Vomiting; Thiamine Deficiency; Cognitive Decline; Malnutrition.
Introduction
Wernicke’s encephalopathy (WE) is an acute neuropsychiatric disorder caused by thiamine (vitamin B1) deficiency, leading to disruption of cerebral energy metabolism and selective vulnerability of regions with high metabolic demand, such as the thalami, mammillary bodies, and periaqueductal gray matter. Although classically associated with chronic alcoholism, WE is increasingly recognized in non-alcoholic patients, where it often presents atypically and is more likely to be underdiagnosed or misdiagnosed, resulting in severe or irreversible neurological damage if untreated [1-3].
In non-alcoholic individuals, WE may arise in a variety of clinical settings that compromise nutritional intake or increase thiamine demand. These include prolonged vomiting, gastrointestinal surgery, malignancy, hyperemesis gravidarum, and chronic illness. The absence of a history of alcohol use can delay diagnosis, particularly when the classic triad of ophthalmoplegia (or nystagmus), ataxia, and confusion is incomplete. Indeed, studies report that this triad is present in only a minority of non-alcoholic WE cases [1-3].
Liang et al. described a non-alcoholic WE case presenting with prominent polyneuropathy and without the full clinical trial, leading to delayed diagnosis and treatment [1]. Similarly, Guler et al. reported a non-alcoholic patient with atypical MRI findings, emphasizing that radiological pattern in WE could be subtle or incomplete. Their case highlighted the importance of maintaining clinical suspicion even when imaging does not reveal classic lesions [3].
MRI remains an essential tool in the diagnosis of WE. Zilioli et al. retrospectively examined 12 non-alcoholic WE patients and found that symmetric lesions in the thalami and periaqueductal region were common in those with altered consciousness. Moreover, cortical involvement was associated with worse outcomes, including death and persistent vegetative state. Importantly, early administration of high-dose thiamine led to radiologic and clinical recovery in patients without cortical lesions [2].
In this report, we present a case of a 30-year-old woman with chronic nausea and vomiting who developed cognitive impairment and gait disturbance. Despite no history of alcohol use, her clinical features and MRI findings were consistent with WE. Prompt recognition and high-dose intravenous thiamine resulted in significant improvement. This case highlights the need for heightened clinical vigilance for WE in non-alcoholic settings and supports early intervention to prevent lasting neurological damage.
Case Presentation
A 30-year-old female with a history of anxiety, depression, and gastroesophageal reflux disease (GORD) presented with a three-month history of persistent nausea, vomiting, and significant weight loss (5 stone/32 kg). Initial blood work revealed hypokalaemia, hypomagnesemia, and mildly elevated inflammatory markers, which were corrected. Further testing showed low folate, low iron, and low transferrin, with a transferrin saturation of 17%, suggestive of nutritional deficiencies. Vitamin B12 levels were within normal limits. Inflammatory markers included an elevated erythrocyte sedimentation rate (ESR), with low complement C3 and C4, raising concerns for a possible autoimmune or inflammatory pathology.
She was initially treated for an Escherichia coli urinary tract infection and underwent further investigations for her ongoing gastrointestinal symptoms and significant weight loss. CT thorax, abdomen, and pelvis (CT TAP) was unremarkable, aside from gallbladder calculi with mild wall thickening (3.2 mm), which did not warrant acute intervention. Oesophagogastroduodenoscopy (OGD) confirmed esophagitis, with no evidence of malignancy or structural obstruction.
Despite supportive treatment, her symptoms persisted and evolved, with worsening swallowing difficulties, persistent hiccups, and progressive fatigue, raising concerns for an underlying systemic or neurological disorder. She subsequently developed confusion, disorientation, and blurry vision, prompting further neurological assessment. A bedside Abbreviated Mental Test (AMT) score of 7/10 indicated cognitive impairment, leading to brain imaging. A CT head was performed, revealing benign tonsillar ectopia (<5mm), but no acute pathology. As her neurological symptoms worsened, she was treated for a suspicion of meningitis/encephalitis, CSF analysis was unremarkable, and viral and bacterial infections were rule out Afterwards, MRI brain was requested, though delayed due to claustrophobia, necessitating imaging under general anaesthesia (GA).
MRI findings, combined with her clinical presentation, fulfilled the semiological triad of Wernicke’s encephalopathy: ophthalmoplegia, confusion, and ataxia. She exhibited altered mental status (confusion), visual disturbances (blurry vision and possible ophthalmoplegia), and unsteadiness, consistent with the classical features of the disease. Given her three-month history of nausea, vomiting, and hiccups, the possibility of neuromyelitis optica spectrum disorder (NMOSD) with area postrema involvement was also considered, prompting further autoimmune workup, which was unremarkable.
Prompt recognition of this triad altered mental status (confusion), visual disturbances (blurry vision and possible ophthalmoplegia), and unsteadiness along with MRI findings helped confirming the diagnosis of non-alcoholic Wernicke’s encephalopathy. Consequently, immediate initiation of high-dose intravenous thiamine was given resulting in gradual cognitive and visual improvement and the patient was started on physiotherapy to help with her gait disturbance and mobility issues.
Below is a table summarizing results of the relevant laboratory investigations conducted during the patient's hospital stay.
|
NO |
Type of investigation |
Result |
Result |
|
1 |
Anti MOG antibody |
negative |
Negative |
|
2 |
Anti CCP |
1.1 |
Negative |
|
3 |
DsDNA |
16.5 |
Normal |
|
4 |
Cardiolipin |
Negative |
Negative |
|
5 |
ESR |
67 |
Elevated |
|
6 |
GBM antibodies |
<2.9 |
Negative |
|
7 |
Complement C3 |
2.55 g/L |
Elevated |
|
8 |
Complement C4 |
0.69 g/L |
Elevated |
|
9 |
ANA |
Negative |
Negative |
|
10 |
serum paraprotein |
Negative |
Not detected |
|
11 |
Meningitis/Encephalitis Pathogens PCR |
Negative |
Not detected |
|
12 |
CSF ANALYSIS |
||
|
12(a) |
CSF Protein |
472 |
Elevated |
|
12(b) |
CSF Glucose |
4.5 mmol/L |
Elevated |
|
12(c) |
CSF Lactate |
3.0 mmol/L |
Elevated |
|
12(d) |
Oligoclonal bands |
Identical |
Identical |
|
12(e) |
Xanthochromia |
Negative |
No evidence |
|
13 |
Cortisol |
475 |
Normal |
|
14 |
TSH |
1.8 |
Normal |
|
15 |
Folate |
2.1 |
Low |
|
16 |
Iron |
7.4 umol/L |
Low |
|
17 |
Vitamin B12 |
465 |
Normal |
|
18 |
Urine culture |
E. Coli |
Positive |
|
19 |
Serum Sodium |
138 |
Normal |
|
20 |
Serum Potassium |
3.4 |
Low |
|
21 |
ANCA |
||
|
21(a) |
Anti MPO |
3.7 |
Negative |
|
21(b) |
Anti PR3 |
<2.3 |
Negative |
|
21(c) |
B2G IgG |
1.1 |
Negative |
|
21(d) |
B2G IgM |
<1.0 |
Negative |
|
22 |
Immunoglobin |
||
|
22(a) |
IgG |
12.63 |
Negative |
|
22(b) |
IgM |
1.38 |
Negative |
|
22(c) |
IgA |
4.28 |
Elevated |
|
23 |
Rheumatic factor |
<10 |
Negative |
Table 1: Relevant investigation results
MRI revealed bilateral symmetrical high signal intensities on T2-weighted and FLAIR sequences involving the thalami, periaqueductal grey matter, mamillary bodies, and regions surrounding the third ventricle. These findings were associated with mild post-contrast enhancement, suggestive of inflammatory or metabolic encephalopathy. The tectal plate demonstrated hyperintensity changes on FLAIR. FLAIR images showed cortical hyperintense changes in the high frontal region. Post-contrast T1-weighted images demonstrated enhancement of the mamillary bodies and periaqueductal grey matter. These findings are characteristic of metabolic or nutritional encephalopathy, such as Wernicke's encephalopathy. (Figures 1-5)
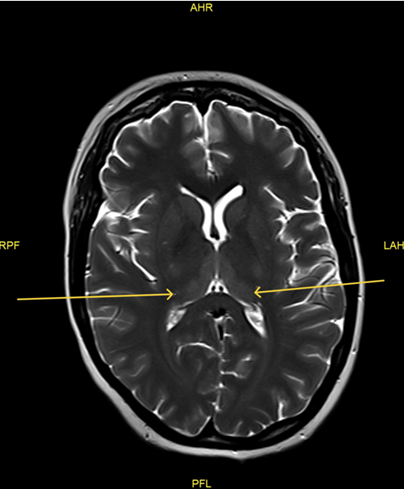
Figure 1: Post contrast (T1) mamillary body enhancement and periaqueductal grey matter enhancement
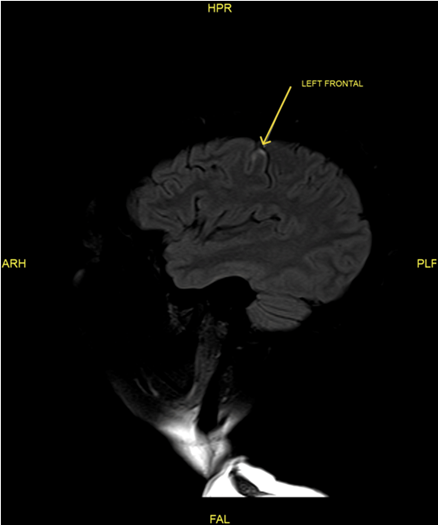
Figure 2: Flair Image:Cortical high frontal region hyperintense changes
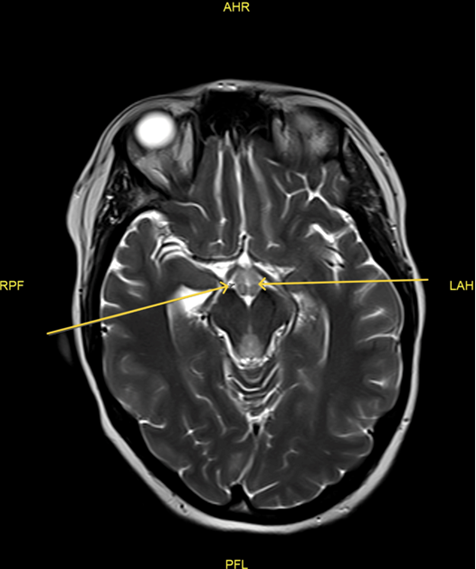
Figure 3: Bilateral mamillary body hyperintensity
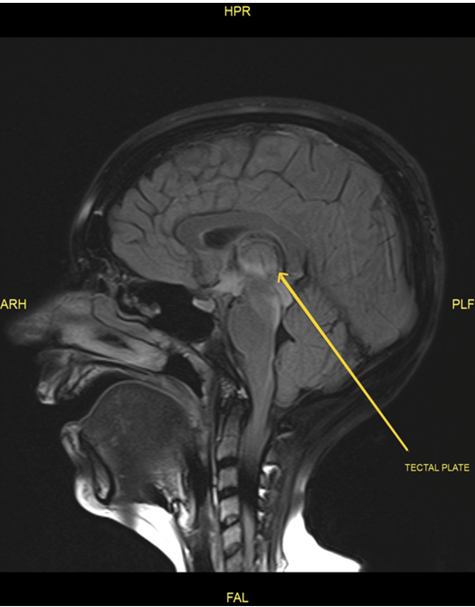
Figure 4: Flair image: Tectalplate hyperintense changes
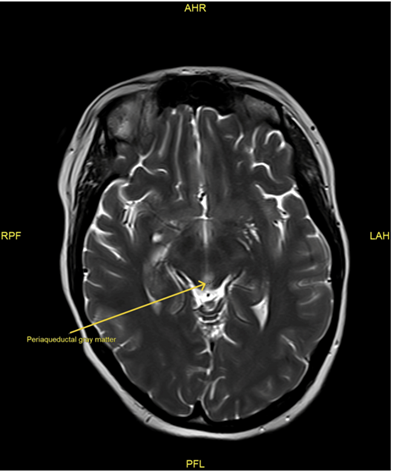
Figure 5: Periaqueductal grey matter hyperintensity
Discussion
Wernicke’s encephalopathy (WE) is a life-threatening but reversible neurologic syndrome resulting from thiamine (vitamin B1) deficiency. Although it is classically associated with chronic alcoholism, increasing recognition of non-alcoholic cases has broadened the clinical understanding of WE. Our case highlights a typical radiologic but clinically nuanced presentation of non-alcoholic WE in a young female with prolonged vomiting and nutritional compromise. This case provides a meaningful point of comparison with several previously reported non-alcoholic WE cases, offering both alignment and contrast in terms of clinical presentation, diagnostic approach, and imaging findings.
A key feature of our case is the presence of the full classical triad-ophthalmoplegia, ataxia, and confusion-though these symptoms evolved gradually and began with nonspecific manifestations like fatigue, visual changes, hiccups, and unsteadiness. In contrast, Liang et al. (2017) described a non-alcoholic patient who did not display the full triad and instead presented with prominent peripheral polyneuropathy, which diverted diagnostic consideration away from WE [1]. The delayed diagnosis in that case resulted from both the absence of hallmark features and the misleading presence of peripheral involvement. While our patient shared some gastrointestinal and neurologic symptoms (notably nausea and unsteadiness), the early appearance of cognitive and oculomotor signs, along with characteristic MRI changes, allowed for a more prompt diagnosis. This comparison underscores how non-alcoholic WE can either mask itself with atypical symptoms-as in Liang’s case-or reveal itself gradually, as in ours, depending on symptom progression and clinical vigilance.
Further, our patient’s persistent vomiting and hiccups initially raised suspicion for neuromyelitis optica spectrum disorder (NMOSD), a diagnostic consideration also explored by Zilioli et al. (2023). In their case, area postrema involvement led to intractable nausea, vomiting, and hiccups, closely mimicking NMOSD and necessitating autoimmune workup and extensive imaging [2]. However, their patient experienced a more complex and ambiguous diagnostic course due to overlapping radiologic features and symptomatology. In contrast, while our patient had overlapping gastrointestinal symptoms, the diagnosis of WE was favored over NMOSD based on the absence of longitudinal spinal cord lesions, optic neuritis, and negative autoimmune serology. Moreover, MRI in our case showed classic symmetric hyperintensities in the thalami, mammillary bodies, and periaqueductal gray-hallmarks of WE-which provided further diagnostic clarity. The comparison demonstrates that while gastrointestinal symptoms can appear in both disorders, careful exclusion of NMOSD-specific features and reliance on clinical context and MRI distribution can effectively differentiate the two.
From an imaging standpoint, our case aligns more closely with traditional radiological patterns of WE than the atypical presentation reported by Guler et al. (2015). Their non-alcoholic patient exhibited atypical MRI findings that initially did not match the clinical picture, resulting in diagnostic uncertainty [3]. They emphasized the limited sensitivity of MRI (approximately 53%), noting that imaging may not always reflect the clinical severity or distribution of symptoms. In contrast, our patient’s imaging demonstrated the classic pattern of symmetrical involvement in diencephalic and periaqueductal regions, which helped confirm the clinical suspicion of WE early in the course of illness. This distinction illustrates a key learning point: although MRI is a valuable diagnostic tool, its reliability varies. In our case, timely imaging complemented the clinical evaluation, whereas in Guler et al.’s case, imaging introduced diagnostic ambiguity.
Treatment response also highlights a critical difference. In all three reference cases, delayed diagnosis often contributed to more prolonged or incomplete recovery. For example, Liang et al.’s patient required extended supportive care and had persistent neurological deficits following late thiamine initiation [1]. By contrast, our patient improved rapidly after high-dose intravenous thiamine, illustrating the importance of early empirical treatment even when diagnostic uncertainty exists. This supports current clinical guidelines advocating immediate thiamine administration in suspected cases, given the low risk of overtreatment and the high stakes of missed or delayed intervention.
In summary, our case both aligns with and diverges from existing non-alcoholic WE literature. Like Liang et al. and Guler et al., we underscore the diagnostic challenges inherent in non-alcoholic WE, particularly in the presence of atypical symptoms or when the classical triad is absent. However, our case stands apart by presenting the full triad, typical imaging, and a favourable response to prompt treatment, illustrating a best-case scenario in a typically under-recognized condition. Compared to Zilioli et al., our case also demonstrates that although NMOSD may mimic WE symptomatically, detailed neurologic and radiologic evaluation can help delineate the two. Ultimately, this case reinforces the growing recognition of non-alcoholic WE and the necessity for early suspicion, rapid assessment, and empirical treatment-regardless of alcohol history.
Conclusions
Wernicke’s encephalopathy should not be overlooked in non-alcoholic patients, particularly those with prolonged vomiting, significant weight loss, and evidence of nutritional deficiencies. This case demonstrates that timely recognition of the classical clinical triad-confusion, ophthalmoplegia, and ataxia-combined with supportive MRI findings, is crucial for diagnosis. Importantly, early initiation of high-dose intravenous thiamine led to clinical improvement, highlighting the treatable nature of this condition when promptly managed. Clinicians must maintain a high index of suspicion for WE in at-risk patients, regardless of alcohol history, to prevent irreversible neurological damage or death.
Key Learning Points
Wernicke’s encephalopathy can occur without alcohol use
Although commonly associated with chronic alcoholism, non-alcoholic WE is increasingly recognized in patients with malnutrition, prolonged vomiting, or gastrointestinal disorders. Clinicians should maintain a high index of suspicion in non-alcoholic individuals who are nutritionally compromised.
Classic Triad May Be Incomplete or Evolve Gradually
The classical triad of confusion, ophthalmoplegia, and ataxia may be absent or develop progressively, particularly in non-alcoholic WE. In this case, the full triad eventually became apparent but initially presented with subtle or nonspecific symptoms like fatigue, hiccups, and visual disturbances.
MRI is Crucial but Not Always Definitive
MRI findings, including symmetric hyperintensities in the thalami, mammillary bodies, and periaqueductal grey matter, are supportive but not universally present. While imaging supported diagnosis here, clinicians should not rely solely on MRI, especially in atypical cases.
Early Thiamine Administration is Critical
Prompt high-dose intravenous thiamine can lead to significant clinical improvement and prevent irreversible neurological damage. This case illustrates the importance of initiating empirical thiamine therapy before confirming diagnosis, given its safety and potential benefit.
Non-Alcoholic WE Can Mimic Other Neurological Conditions
This case mimicked neuromyelitis optica spectrum disorder (NMOSD) due to gastrointestinal symptoms and hiccups. A thorough autoimmune workup and imaging helped distinguish WE from other mimics. Differential diagnosis is essential to avoid delays in treatment.
References
- Liang H, Wu L, Liu L, Han J, Zhu J, et al. (2017). A case report: Non-alcoholic Wernicke encephalopathy associated with polyneuropathy. Journal of International Medical Research, 45: 1794-1801.
- Zilioli A, Misirocchi F, Mutti C, Romano S, Minetti M, et al. (2023). Non-alcoholic Wernicke's encephalopathy mimicking neuromyelitis optica spectrum disorder in a young woman: a case report and literature review. Acta Biomed. 5: 2023111.
- Guler A, Alpaydin S, Sirin H, Calli C, Celebisoy N. (2015) A non-alcoholic Wernicke's encephalopathy case with atypical MRI findings: Clinic versus radiology. Neuroradiol J. 28: 474-7.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.