New Adolescent Psychiatry Unit: Challenge in Care, Suicidal Prevention and Partnership with Pediatric Emergency Department
by Coulon N1,2*, Caubit L3,4, Michard Lenoir AP3
1Specialized psychiatric establishment, Alpes Isere Hospital Center (CHAI Centre Hospitalier Alpes Isère), Adolescent intensive outpatient center, Child and adolescent Psychiatry Department, 3 Rue de la Gare, 38 120 Saint-Egrève, France.
2FondaMental Foundation, Public Assistance from Paris hospitals, Créteil, France.
3Grenoble-Alpes University Hospital Center, Reference center for child protection, Pediatric Department and Forensic-Social Medicine Department, Boulevard de la Chantourne, 38 700 La Tronche, France.
4Grenoble Alpes University, Medecine Faculty, 23 Avenue des Marquis du Gresivaudan, 38 700 La Tronche, France.
*Corresponding author: Nathalie Coulon, Specialized psychiatric establishment, Alpes Isere Hospital Center (CHAI Centre Hospitalier Alpes Isère), Adolescent intensive outpatient center, Child and adolescent Psychiatry Department, FondaMental Foundation, Public Assistance from Paris hospitals, Créteil, France
Received Date: 12 August 2025
Accepted Date: 22 August 2025
Published Date: 26 August 2025
Citation: Coulon N, Caubit L, Michard Lenoir AP (2025) New Adolescent Psychiatry Unit: Challenge in Care, Suicidal Prevention and Partnership with Pediatric Emergency Department. Arch Pediatr 10: 332. https://doi.org/10.29011/2575-825X.100332
Abstract
Objective: In 2014, World Health Organization raise awareness of suicide as a public health issue. In France, suicide is also the second leading cause of death for young people aged 15 to 24. Moreover, covid 19 pandemic has increased adolescent distress. Very few studies have been carried out in teenagers, who have received care from pediatricians and child psychiatrists. Our study focuses thus on this partnership between Pediatric emergency Department - Child and adolescent psychiatry Department. Our main objectives were first to compare hospitalization durations in Pediatric emergency Department for these teenagers in crisis, and second to measure the rate of suicide attempt recidivism, before and after the opening of the new adolescent psychiatry unit. Method : Retrospective and prospective, single-center, descriptive and comparative study, over a period of 3 months before (period 1) and 3 months after (period 2), the opening of the adolescent intensive outpatient center, on 2022, April the 19th. Results : In both periods studied, population of selected adolescents (N = 184) appeared relatively homogeneous with a mean age 14.64 ± 1.34 years, an over-representation of girls, and very frequent presence of a personal psychiatric history. Despite the expectations, there was no decrease in the length of stay in short-term bed but no recurrence at 3 and 6 months for the teenagers who have benefited from care within the adolescent intensive outpatient center. Conclusion: New adolescent psychiatry unit and its partnership with Pediatric emergency Department would seem effective in reducing the risk of suicidal recidivism for adolescents in crisis. Studies must continue to confirm the recidivism reduction. Taking care of adolescents, helping them better, prepare the adults of tomorrow: a challenge of prevention and care
Introduction
In the world of teenagers, suicide and its entire lexical field has become more and more frequent in all discussions, media, daily life, questioning all professionals (care, teaching, educational), as well as loved ones, for more than 10 years. According to the NIMH [1], suicide is defined as death caused by self-directed injurious behavior with intent to die, as a result of the behavior. A suicide attempt (SA) is a non-fatal, self-directed, potentially injurious behavior with intent to die. A suicide attempt might not result in injury. Suicidal ideations (SI) refers to thinking about, considering, or planning suicide, as a possible way out in a context of emotional pain. In addition, a suicidal crisis is an evolution of mental processes, with a variable duration, whose major risk is suicide. During adolescence, looking for suicidal equivalents, these self-directed injurious behavior often repetitive where intent to die is not explicit (for examples: some scarifications, or addictions, or certain eating disorders), is also interesting.
In 2014, World Health Organization (WHO) raise awareness of suicide as a public health issue in a report “Preventing suicide, a global imperative” [2]. Suicide prevention is an integral part of the plan. About mental health of adolescents in particular, WHO described in 2021 that globally one in seven 10-19-yearolds experiences a mental disorder, accounting for 13% of the global burden of disease in this age group [3]. In 2023, WHO [4] updates the suicide figures about adolescent and young adult health: 1) Depression and anxiety are among the leading causes of illness and disability among adolescents; 2) Half of all mental health disorders in adulthood start by age 14, but most cases are undetected and untreated; 3) Suicide is among the leading causes of death in people aged 15–19 years; 4) One key fact is that over 1.5 million adolescents and young adults, aged 10-24 years, died in 2021, about 4500 every day. Moreover a systematic analysis showed the leading causes of death were self harm in 15-19 year old females and road traffic injuries in 15-19 year old men [5].
In France, Epidemiology center on medical causes of death (CépiDc) of the National Institute of Health and Medical Research (Inserm) estimated 8 366 suicides in 2017 [6], with the assumption of an underestimation of 10%, and in particular 25 deaths by suicide (2.3 %) in subjects aged 1-14, 326 (13.5%) in subjects aged 15-24. Consequently, the share of suicide in the overall French mortality is significantly higher, among young people of both sexes than among elderly people. Nevertheless, average standardized rates of deaths by suicide vary widely depending on the region in the country and seem relatively lower in the southern French regions, below the Loire, as Auvergne-Rhône-Alpes. So, between 2015 and 2017 [6], in the whole of France (excluding Mayotte), the rate of deaths by suicide was 14.0 per 100.000 residents while it was 12.4 per 100 000 residents in the Auvergne-Rhône-Alpes region. The gradual decline in suicide mortality in our region has been confirmed since 2000 (average drop in the standardized rate of 2.1% per year) [7]. However, since 2014, an upward trend in the age group 15-29 years has been recorded [7]. The data concerning suicide attempts and suicidal thoughts declared during adolescence through the use of two surveys (ESCAPAD and ESPAD) [8] piloted by the French Observatory of Drugs and Drug Addiction (OFDT) highlighted : 1) as in the WHO figures [4], suicide is the second leading cause of death for young people aged 15 to 24; nearly 3% of all teenagers aged 17 reported having attempted suicide during their lifetime, resulting in hospitalization, and one in ten adolescents (10.4%) having thought about suicide, at least once, in the last twelve months.
In addition to this worrying development on suicide, the covid 19 pandemic has increased adolescent distress [9-12]. Consultations for this medical reason have exploded in Pediatric emergency Department [13-14]. Note however, numerous articles have been published on the subject of suicide attempts among young people, but the heterogeneity of data collection methods makes it challenging to compare them [15]. In the same way, few studies have been carried out in teenagers in crisis who have received care from pediatricians and child psychiatrists [16]. Our study focuses thus on this partnership between Pediatric emergency Department - Child and adolescent psychiatry Department, with the creation of a new adolescent psychiatric unit, focused on crisis symptomatology. Our main objectives were first to compare hospitalization durations in Pediatric emergency Department for these teenagers in distress, and second to measure the rate of suicide attempt recidivism, within the first six months, before and after the opening of the new adolescent psychiatry unit.
Method
Study design
The study design was retrospective and prospective, single-center, descriptive and comparative, over a period of 3 months before (period 1) and 3 months after (period 2), the opening of a new adolescent psychiatric unit, an intensive outpatient center for teenagers, on 2022, April the 19th. For more details, the design follows the lines of the French national call for projects DGOS/ R4/2019/175 “Structuring the pathway for teenagers in child psychiatry” [17] whose objective were to allocate new measures in child psychiatry and to response, for us in particular (Figure 1), on the care area in France, South Isere (38). With cooperation of Grenoble-Alpes University Hospital Center (GA-UH), France Student Clinic Grenoble-La Tronche and Isere area (38), the specialized psychiatric establishment, Alpes Isere Hospital Center (CHAI Centre Hospitalier Alpes Isère), the boss in the adolescent psychiatry sector, proposed a crisis unit, making the link in all the adolescent healthcare area. The main principle of the outpatient crisis unit for adolescents was designed to respond quickly to the suffering of teenagers, with the idea of reducing the workload on pediatric emergencies and overloaded colleagues in the South Isere area.

Figure 1: location of the country and the city of the study.
Population
Inclusion criteria
Were collected all the adolescents (12-17 years of age), admitted to the Pediatric emergency Department of GA-UH for a suicide attempt or suicidal ideations. For safety and monitoring, these young patients were admitted, in particular, on a bed in the shortterm unit of the Pediatric emergency Department (GA-UH).
The duration of the study extended over two periods of 3 months, one before the opening of the new adolescent psychiatric unit in CHAI, the other after the opening of CHAI’s unit. Iinitially, according to the national calendar of the call for projects, the unit was to open in 2021, November and we had projected period 1 on 2021, March-June and period 2 on 2022, March-June. However, the development work for the opening of the unit was delayed and the unit was only able to open on 2022, April, the 19th. So, period 1 was kept on 2021, March-June, and period 2 was shifted to 2022, May-August.
Exclusion criteria
Were excluded all the adolescents with 1) age outside 12-17 years; 2) crisis symptoms where mental retardation, a state of agitation or prolonged hospitalization were at the forefront of the clinical picture; 3) a lack of precise domiciliation; and 4) an opposition from parents or from the teenager himself for the study.
Measures
With the agreements of the doctors responsible for Pediatric Department (GA-UH), Child and adolescent Psychiatry Department (CHAI) and the head doctor of Pediatric emergency Department (GA-UH), were collected all eligible subjects admitted in Pediatric Emergency Department (GA-UH): N = 138 in period 1 and N = 146 in period 2. In both periods, in a retrospective mode, all medical files with a reason for admission to child psychiatry were examined such that each period contains 92 medical records (Figure 2). Suicidal crisis clinic was searched with SA, SI, and history (personal medical/ surgical/ child psychiatric and family psychiatric). Were also noted 1) sociodemographic data (age, sex, number of siblings, sibling position, lifestyle, schooling, parents’ marital status); 2) current and passed treatment; and 3) total length of hospital stay in Pediatric emergency Department.
Finally in both periods, in a prospective mode for each subject, the question of suicidal recidivism at 3 and 6 months was followed, through the possibility of readmission in Pediatric emergency Department.
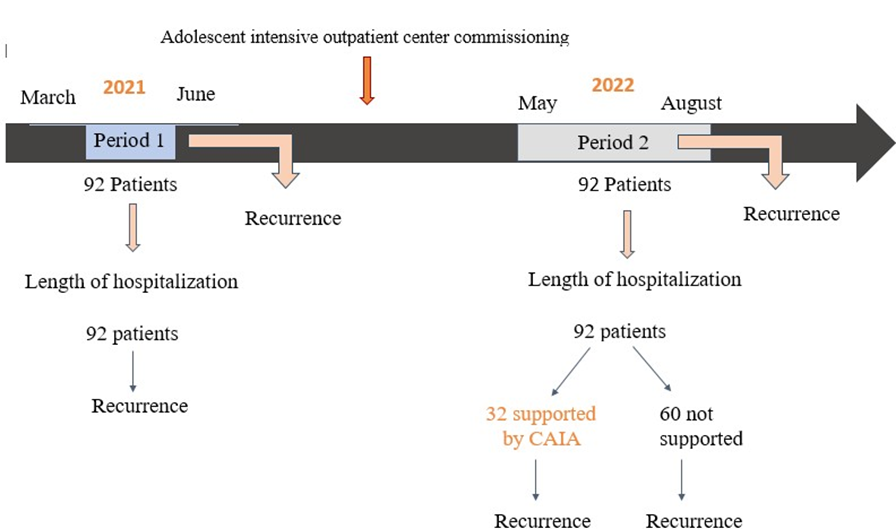
Figure 2: Study and chronology
Care
Grenoble-Alpes University Hospital Center, Pediatric Emergency Department
In Pediatric emergency Department, adolescents are welcomed and cared for by a multidisciplinary team: doctors, nurses, educators, psychologists. Furthermore, parents, relatives or other person close to the youth, are received in order to better understand the situation. Safety measures are ensured throughout the hospitalization [18]. Depending on clinic and problem, a shortterm bed is offered to take some distance from the acute crisis and monitor the young patient over several hours or even days. According to recommendations19, the length of stay in short-term bed from Pediatric Emergency Department should not exceed two consecutive nights or around 48 hours; however, the reality is sometimes quite different and this is very frequently exceeded.
At the end of the care, a referral is made, either towards hospitalization in another unit, or towards discharge with recommendations [18, 20].
Specialized Psychiatric establishment, adolescent intensive outpatient center
On the new teen psychiatric unit, the adolescent intensive outpatient center, Pediatric emergency Department assessments are continued and deepened on the medical, nursing, psychological and socio-educational dimensions. Various therapeutic mediations (artistic, physical, some of which are in partnership with the city of Grenoble, or the Isere area) are used. Links with family, relatives and the entire network around the young person are also examined. This care system with an outpatient schedule of 5 half-days, after the stay in Pediatric emergency Department, is presented as soon as the adolescent presents symptoms of a crisis and even more so if he is suicidal.
In general, admissions from Pediatric emergency Department are prioritized on the new psychiatric unit. Each day, from Monday to Friday, an emergency consultation slot is reserved for a potential admission, or an urgent consultation. So, each week, the intensive adolescent outpatient center can receive an average of 5 new adolescents. Adolescent, relatives and care professionals commit in each adolescent care project, and sign a care contract for these 5 half-days.
For each patient lastly, a care orientation is worked on after the 5 half-days schedule, after a multi-professional synthesis meeting. Only a few adolescents will continue treatment for a period of two months. The lengths of stay at the adolescent intensive outpatient center are announced from the outset and are relatively strict in order to allow for continuous turnover.
Finally, in this new adolescent system under construction, it should be noted that this adolescent intensive outpatient center is a link designed in conjunction with crisis beds, for young patients with more severe symptoms. The plan would be to create six beds dedicated to the crisis center, open 24/7. All the new crisis unit is not intended to provide regular long-term care for patients, and must be coordinated with the various players involved in the patient’s care project.
Ethical Concerns
The study was carried out in accordance with ethical principles for medical research involving humans (World Medical Association WMA, Declaration of Helsinki). The Clinical Research and Innovation Department of the Grenoble University Hospital, which works under agreement with the psychiatric establishment (CHAI), validated the research protocol. All participants (and the legal guardians, for minors) received appropriate information; the study was explained on request and a poster was placed in the waiting room of the Pediatric emergency Department
All data were collected anonymously with an alphanumeric code, from computerized medical records, by a single operator, to ensure consistency and accuracy.
Statistical analysis
Firstly, statistical analysis was performed to determine the required sample size for the study, in order to obtain results with satisfactory statistical power. This calculation of the number of subjects required was thus estimated from various factors, such as the expected reduction in length of hospital stay and variability in this measure, based on historical data from previous months. The result was at least N = 91 for each period studied and we opted for N = 92 in each period, in order to secure data.
Secondly, descriptive statistics were used. For continuous variables, quantitative data were presented with mean, standard deviation, median, quartile, minimum and maximum. For qualitative variables, frequency and percentage were conducted. To compare variables, for quantitative data, Student’s t test or non-parametric tests (depending on the validity conditions) were realized and for quantitative data, univariate tests such as Chi-square test or Fischer test were followed. Analysis and statistical testing were conducted using JAMOVI software. Results
Population characteristics
Sociodemographic and clinical characteristics, for both periods studied, can be observed in (Table 1). Overall, the total population (N = 184) appeared relatively homogeneous with a mean age 14.64 ± 1.34 years (mean =14.56 ± 1.39 y in period 1, vs mean = 14.68 ± 1.25 y in period 2; p = 0.608), an over-representation of girls (85.3 %). However, note that a statistically significant difference was found in the sex ratio with more boys over period 2 (8.7 % boys in period 1 vs 20.7 % in period 2; p = 0.022) and more suicide attempts in period 2 (33.7 % in period 1 vs 50 % in period 2; p = 0.025 . There was also a statistical significant difference in terms of parental marital status, with parents more frequently separated in period 2 (parents separated 47.1 in period 1 vs 62.1 % in period 2; p = 0.048).
On an overview, the adolescent population in crisis of the study was illustrated through a place of the eldest in the siblings (close 40 %) and around 20 % of subjects mentioned school bullying, while between 8 to 13 % of teenagers have dropped out of school. About psychopathology, social history (around 11.5 % of adolescents were dependent on child welfare), medical history (around 10 % of teenagers with chronic illness), and even more psychiatric history were very present before admission to the Pediatric emergency Department: 1) previous suicide attempt (more than a third of adolescents); 2) previous scarifications (more than 60 % of cases); 3) previous private sector consulting (around 50 %); 4) previous treatment (about half were taking anxiolytics and about a third were taking antidepressants); 5) addictions (approximately a quarter reported using tobacco and 15.4 % cannabis).
|
Period 1 (N = 92) |
Period 2 (N = 92) |
|||
|
N, mean or % ; (25, 75) |
N, mean or % ; (25, 75) |
p (α = 5%) |
||
|
Age |
(N=184) |
14.56 ±1.39 (13.0;16.0) |
14.68 ±1.25 (13.8;16.0) |
0.608 |
|
Gender Boys, N (%)/Girls, N (%) |
(N=184) |
8 (8.7%) / 84 (91.3%) 1 boy / 10.5 girls |
19 (20.7%)/ 73 (79.3 %) 1 boy / 3.8 girls |
0.022* |
|
SA |
(N=184) |
31 (33.7 %) |
46 (50.0%) |
0.025* |
|
Sibling position - Oldest sibling - Other - Youngest - Single |
(N=159) |
- 33 (39.6%) - 12 (14.5%) - 24 (28.9%) - 14 (16.9%) |
- 28 (36.8%) - 6 (7.9%) - 25 (32.9%) - 17 (22.4%) |
0.490 |
|
Lifestyle - Children social welfare - Family, parents |
(N=182) |
- 10 (11.0%) - 81 (89.0%) |
- 11 (12.1%) - 80 (87.9%) |
0.817 |
|
School bullying |
(N=184) |
19 (20.7%) |
21 (22.8%) |
0.721 |
|
No schooling |
(N=184) |
8 (8.7%) |
12 (13.0%) |
0.343 |
|
Parents Marital status - Together - Separated |
(N=184) |
- 45 (52.9%) - 40 (47.1%) |
- 33 (37.9%) - 54 (62.1%) |
0.048* |
|
Medical history - Chronic illness |
(N=184) |
13 (14.1%) - 10 (10.9%) |
10 (10.9%) - 9 (9.8%) |
0.504 - 0.809 |
|
Psychiatric history - SA - Scarifications |
(N=183) |
- 32 (35.2%) - 55 (60.4%) |
- 41 (44.6%) - 62 (67.4%) |
- 0.194 - 0.327 |
|
At least, 1 previous consultation |
(N=184) |
22 (23.9%) |
15 (16.3%) |
0.198 |
|
At least, 1 previous hospitalization |
(N=184) |
27 (29.3%) |
22 (23.9%) |
0.404 |
|
Previous psychological or psychiatric ttt - Medicopsychological outpatient center (public medecine) - Private sector consulting - University Hospital Center |
(N=181) |
64 (71.1%) - 13 (14.4%) - 47 (52.2%) - 3 (3.3%) |
68 (74.7%) - 19 (20.9%) - 43 (47.3%) - 4 (4.4%) |
0.584 - 0.257 - 0.504 - 1.000 |
|
Drug treatment - Anxiolytics - Antidepressants |
(N=184) |
45 (48.9%) - 39 (42.4%) - 32 (34.8%) |
55 (59.8%) - 47 (51.1%) - 29 (31.5%) |
0.139 - 0.237 - 0.638 |
|
Addiction - Tabacco - Cannabis |
(N=175) |
24 (26.1%) - 22 (23.9%) - 15 (16.3%) |
24 (28.9%) - 24 (28.9%) - 12 (14.5%) |
0.675 - 0.453 - 0.736 |
|
Diagnosis - Anxiety disorders - Mood disorders - Eating disorders |
(N=184) |
- 34 (30.9%) - 43 (46.7%) - 12 (13.0%) |
- 17 (23.0%) - 42 (45.7%) - 16 (17.4%) |
- 0.238 - 0.882 - 0.412 |
Table 1: Sociodemographic and clinical characteristics for both periods studied.
Data on hospitalization in Pediatric emergency Department and suicidal gesture
Data about hospitalization in Pediatric emergency Department and suicidal gesture were summarized in (Tables 2a, 2b, and 2c). Firstly, in terms of admissions to Pediatric emergency Department, they occurred significantly more at night over period 2 (55.4 % in period 1 vs 70.7 % in period 2; p = 0.032). Secondly however, there is no statistically significant difference either in the accompanying persons present with the teenagers (majority = parental support), or in hospital referrals following admission. In both periods studied, approximately three quarters (72.8 % in period 1 vs 77.2 % in period 2) of admissions to Pediatric emergency Department, for an adolescent meeting the inclusion criteria (so with already an admission in short-term bed), were followed by an extension of the stay in the short-term bed in this same Pediatric emergency Department (GA-UH). A fifth of these teenagers admissions (20.7 % in period 1 vs 18.5 % in period 2) were directed to the specialized psychiatric establishment (CHAI) within the Child and adolescent psychiatric Department.
Regarding suicidal gestures (Table 2b), 31 were analyzed over period 1 and 46 over period 2. Both periods studied did not present a statistically significant difference about the modality of the suicide attempt (p = 0.807). Voluntary poisoning was the most common, with 77.4 % in period 1 and 84.8 % in period 2. Other modalities such as phlebotomy, hanging, defenestration were poorly represented in both periods. About voluntary drug intoxication as shown in Table 2c, pharmaceutical[NC1] drugs have been usually involved and in particular paracetamol, but without a statistically significant difference between both periods (paracetamol 75 % in period 1 vs 56.4 % in period 2; p = 0.966). The only difference observed was the presence of more multidrug gestures in period 1 compared to period 2 (45.8 % vs 12.8 %; p = 0.013).
|
Period 1 (N = 92) |
Period 2 (N = 92) |
||
|
N, mean or % ; (25, 75) |
N, mean or % ; (25, 75) |
p (α=5%) |
|
|
Consultation by night (N=184) |
51 (55.4%) |
65 (70.7%) |
0.032* |
|
Companion (N=73) - Parent - Other |
(N=36) - 26 (72.2%) - 10 (27.8%) |
(N=37) - 25 (67.6%) - 12 (32.4%) |
0.665 |
|
Hospitalization referral after admission to the Pediatric emergency Department (N=184) 1) University Hospital Center - Pediatric Emergency Department (Short-term bed) - Pediatrics Department - Intensive care 2) Psychiatric Establishment - Child and adolescent psychiatry Department - Adult psychiatry Department |
- 67 (72.8%) - 4 (4.3%) - 1 (1.1%) - 19 (20.7%) - 1 (1.1%) |
- 71 (77.2%) - 2 (2.2%) - 1 (1.1%) - 17 (18.5%) - 1 (1.1%) |
0.925 |
Table 2a: Hospitalization in Pediatric emergency Department[NC2]
|
Period 1 (N = 31) |
Period 2 (N = 46) |
||
|
N (%) |
N (%) |
p (α = 5%) |
|
|
Modality - Voluntary drug intoxication - Phlebotomy - Hanging/strangulation - Defenestration -Unknown |
- 24 (77.4%) - 2 (6.5%) - 2 (6.5%) - 2 (6.5%) - 1 (3,2 %) |
- 39 (84.8%) - 1 (2.2%) - 2 (4.3%) - 2 (4.3%) - 2 (4.3%) |
0.807 |
Table 2b: Suicidal gesture characteristics (N = 77)
|
Period 1 (N = 24) |
Period 2 (N = 39) |
||
|
N (%) |
N (%) |
p (α = 5%) |
|
|
Voluntary drug intoxication with paracetamol (mono or poly intoxication) |
- 18 (75.0%) |
- 22 (56.4%) |
0.966 |
|
Multidrug gesture |
- 11 (45.8%) |
- 5 (12.8%) |
0.013* |
Table 2c: Voluntary Drug Intoxication (N = 63)
Table 2: Data on hospitalization in Pediatric emergency Department and suicidal gesture.
Evolution from Pediatric emergency Department
For both periods studied, evolution from Pediatric emergency Department was presented in Table 3a. Despite the opening of the new teen unit, with the overall figures on the evolution from Pediatric emergency Department and data on discharge, no statistically significant difference were highlighted, neither in the duration of hospitalization (p = 0.590), nor in the recidivism of suicide attempt at 3 and 6 months (respectively, p = 0.7333 and p = 0.844). Nevertheless, with the opening of the new teen unit, it was obvious that a statistically significant difference appeared in the referral after discharge from the Pediatric emergency Department (p<0.001).
Only in period 2, so the period which was able to benefit from the presence of the new teen unit in its care offering, the evolution from Pediatric emergency Department to the adolescent intensive outpatient center was presented in table 3b. It was then interesting and probably reassuring to note that a statistically significant difference was found in recidivism at 3 and 6 months (respectively p = 0.001 and p < 0.001) if the subject is treated in the adolescent intensive outpatient center. In fact, no recidivism of suicide attempt was found at 3 and 6 months for subjects recruited, and who benefit from adolescents intensive outpatient center (Table 3a, 3b).
|
Period 1 (N = 92) |
Period 2 (N = 92) |
||
|
N, mean or % ; (25, 75) |
N, mean or % ; (25, 75) |
p (α = 5%) |
|
|
Pediatric Emergency Department Length of stay in short-term bed, in hours (N=180) |
66.0 (28.0 ;114) |
73.5 (42.8 ;118) |
0.329 |
|
No referral discharge notified in the file |
9 (9.8%) |
14 (15.2%) |
0.265 |
|
Referral after discharge from the Pediatric emergency Department (N=160) - Medicopsychological outpatient center (public medecine) - Private sector consulting - Hospital - Adolescent intensive outpatient center |
- 21 (25.6%) - 36 (43.9%) - 25 (30.5%) - 0 (0.0%) |
- 11 (14.1%) - 14 (17.9%) - 21 (26.9%) - 32 (41.0%) |
<0.001 |
|
Recidivism at 3 months (N=184) |
15 (16.3%) |
16 (17.4%) |
0.844 |
|
Recidivism at 6 months (N=184) |
24 (26.1%) |
22 (23.9%) |
0.733 |
Table 3a: Evolution from Pediatric emergency Department for both periods studied.
|
|
Period 2 (N = 92) |
|
|
|
Adolescent intensive outpatient center |
NO (N = 60) |
YES (N = 32) |
|
|
|
N, mean or % ; (25, 75) |
N, mean or % ; (25, 75) |
p (α = 5%) |
|
Pediatric Emergency Department Length of stay in short-term bed, in hours |
68 (41.8 ; 119.0) |
85.5 (43.8;117) |
0.740 |
|
Recidivism at 3 months |
16 (26.7%) |
0 (0 %) |
0.001* |
|
Recidivism at 6 months |
22 (36.7%) |
0 (0 %) |
<0.001* |
Table 3b: Recidivism for adolescents cared in Adolescent intensive outpatient center.
Table 3: Evolution from Pediatric emergency Department.
Discussion
Summary of main results
The aim of our study was to assess the impact of a new teen unit from specialized psychiatric establishment, Alpes Isere Hospital Center (CHAI Centre Hospitalier Alpes Isère), the adolescent intensive outpatient center, on the management of adolescents hospitalized for suicide attempts and suicidal ideation, in the Pediatric emergency Department from Grenoble-Alpes University Hospital Center. In this work thus, before and after the opening of the new teen psychiatry unit, we compared length of stay in short-term beds from Pediatric emergency Department and suicidal recidivism at 3 and 6 months. In both periods studied, the total population of selected adolescents appeared relatively homogeneous with a mean age 14.64 ± 1.34 years, an over-representation of girls, and very frequent presence of a personal psychiatric history (previous suicide attempt, or scarifications, or addictions; previous care) with a significant school or family problem. Despite the expectations of Pediatric, emergency Department for adolescents in crisis, with the opening of the new unit, the length of stay in short-term bed has not decreased but no suicide attempt recidivism was found at 3 and 6 months for the teenagers who have benefited from care within the adolescent intensive outpatient center. The new unit and the partnership with Pediatric emergency Department would seem effective in reducing the risk of suicidal recidivism for adolescents in crisis.
Confrontation with literature
Firstly, given the sharp increase in the number of visits in Pediatric emergency Department for child psychiatric reasons [21-22]. and the recurring problem in short-term beds, hoping for a solution with the opening of a new teen unit, dependent on the specialized psychiatric establishment, did not appear utopian. Pediatric emergency professionals had imagined that the length of stay, on observation unit, could be closer to 48 hours. Emergency consultations indeed seemed to have become the first recourse for psychiatric and psychological care for adolescents and the new unit was thought to offer an effective downstream care. However, our result did not reveal any evidence of a reduction in this length of stay, during the period studied following the opening of the new unit. Several hypotheses could be discussed. 1) More suicide attempts were observed over period 2 as shown in Table 1 (33.7 % in period 1 vs 50.0 % in period 2; p = 0.025), which would involve more difficult and complex adolescent cases to treat (perhaps with more boys, more separated parents, more personal psychiatric history, etc), with an increased demand for monitoring, short-term beds, and therefore this impossibility of reducing the length of hospitalization.
In the future adolescent system, crisis beds are planned, but it will take several more years for them to open; the new open adolescent unit is currently just outpatient care, with daytime schedules, which is sometimes still just in acute crisis. 2) Another real difficulty could be the organization, the planning of interviews in a very short time: the young patient, parents and/or relatives, sometimes links with professionals in contact with the teenager, etc. so a succession of steps which requires time, sometimes incompressible. 3) Known to any manager when faced with a multi-professional team, a certain resistance to change should not be neglected; it would be then important to support the team, over a few months, towards an evolution of its professional practices, particularly when the whole adolescent system will be finalized with the outpatient unit and crisis beds.
Secondly, it is very interesting to note that the population recruited in our study corresponds to the national and international literature, with socio-demographic and clinical characteristics of young suicidal people described : preponderance of girls [12, 16, 23-25], modus operandi of drug intoxication [16, 23-26], previous psychiatric history and warning signs before gesture [23-27], schooling conditions (bullying, pressure) [28-29] or family situation [16, 23-24, 30]. In both periods studied, a rate of bullying above 20% among these adolescents in crisis and parental separations expressed in 62.1% of cases in period 2 can only raise questions for us. In 2022, Kreski et al. [31] showed with data about Youth Risk Behavior Survey (2015-2019, N = 44,066), collected biennially, from high school students across the United States, that rates of bullying follow those of suicidal behavior, whether young people are white, black, or any other ethnic or sexual minority. No doubt therefore that the Anti-Bullying and Suicide Prevention Initiatives are linked [32]. A growing phenomenon, which should not be minimized, is also this association via the internet: cyberbulling and suicide [33]. In the United States, the Centers for Disease Control and Prevention recently insisted through their data [33]: 14.9 % of adolescents have been cyberbullied and 13.6 % of adolescents have made a serious suicide attempt, with cyberbullying increasingly associated with victim suicides.
Moreover, since the emergence of Covid-19, in Grenoble as elsewhere [10], the health crisis has had a major impact on young people’s mental health, and we observed suicidal attempts in both periods studied (33.7 % for 2021, March-June and 50 % for 2022, Mai-August). In a similar way, Cousien et al. [34] described an aberrant dynamic of suicide attempts, independent from its annual seasonality and its trend over the 10-year period for the years 2019-2020. Also comparing September 2020 to September 2019, Pierson et al. [35] found, in a hospital complex in North London, an increase of 48 % of under sixteens presenting to the acute hospital with a mental health crisis, and in particular an increase of 133 % for these young people under sixteen presenting with suicidal ideation, and 200 % for females with suicidal ideation. In its 5th report [12] published in September 2022, French National Suicide Observatory reported the same trend with significant and lasting deterioration in the mental health of children and adolescents in the months following the spring 2020 lockdown, which has also led to a significant rise in suicide attempts and self-harm, particularly among teenage girls.
Thirdly, the challenge in care and prevention, with the partnership between Pediatric emergency Department and the new adolescent psychiatric unit, constitutes a key issue. Classically indeed, for adult emergencies, it is accepted that 40 % of people -who have attempted suicide- re-offend during their lifetime, half of them during the year following the suicidal gesture [36]. In a systematic review, Mendez-Bustos et al [37]. reported that 16 % to 34 % of subjects reoffend in the first 1 to 2 years after the suicidal gesture studied. In this continuity, for US teenagers, after a first suicide attempt, Brent et al [38] mentioned a recidivism rate in nearly one adolescent in four, with an increased risk of recidivism in the 6 months following discharge [39]. In a 3-month follow-up assessment after suicide attempt, Spirito et al.[40] reported a 12 % rate of recidivism. At 6 months, several studies, carried out before the covid 19 pandemic, showed recidivism rates of less than 20 %: 14 % in Consoli et al. [41]; 15 % in Brent et al. [39]; and 18 % in Yen et al. [42]. For our study, about suicidal attempts, the 6-months recidivism rate was above 20 %: 26.1 % in period 1
(2021) and 23.9 % in period 2 (2022). However, our data reflected this difficult time of the covid 19 pandemic. Moreover, it is really worth emphasizing that no adolescent, referred by Pediatric emergengy Department to the new psychiatric unit, and treated in this adolescent intensive outpatient center, presented a recurrence at 6 months. Our data seem to point towards a very significant reduction in suicidal attempt recidivism rate at 6-months with the adolescent intensive outpatient center.
Strengths and weaknesses
First of all, it is undeniable that this study is a strength due to its poorly documented, little-known population of adolescents, going through a psychological/ psychiatric crisis, and arriving in the Pediatric emergency Department. With a descriptive and epidemiological process, a powerful work of reading all medical files by a single examiner (LC) to ensure consistency, data contribute to improving knowledge of pediatric emergency professionals, who are sometimes helpless when faced with adolescents in crisis. Choosing to recruit a child psychiatric population, within the Pediatric emergency Department, shows the current reality experienced by pediatricians, in recent last years, and this challenge of the care-prevention partnership with child psychiatrists. The population was also in line with the national and international child psychiatric literature on demographic aspects, and the burden of medical histories such as family or school histories. In addition, the study included a 6-month follow-up of adolescents, a period characterized by a high risk of suicidal attempts recurrence, in order to analyze the recidivism rate. The fact that the Pediatric emergency Department of Grenoble are the only ones in the entire care area studied allows us to be sure of having counted all the young victims of a suicidal attempt recidivism. The encouraging results for the teenagers, treated in adolescent intensive outpatient center, are a key for the future that seeks solutions to suicidal attempts and recidivism. It seems important to continue building care, stabilizing it, further solidifying it in order to help these suffering adolescents.
The main limitation of our study is the retrospective and monocentric aspect of its design. Consequently, some data were missing, notably those concerning the parents’ characteristics (history, addictions, marital status), which makes interpretation more difficult. Then, the work only concerns professionals from Grenoble area, France (the university hospital center and the establishment specializing in psychiatry). Nevertheless, this analysis could easily be reproduced in any other care area, with just a few specific adjustments that would remain site-specific.
Furthermore, despite a prepared, thoughtful and worked protocol, the study had to face the imponderables of reality: 1) the Covid-19 pandemic and the succession of unanticipated lockdowns in period 1 (a confinement from 2021, April 3 to May 3); 2) the consequences of the pandemic on the development work of the new teen psychiatric unit, with an opening center delay of several months and a shift in recruitment for period 2 of several months. In the design, we thought about avoiding summer school holidays, the seasonal effect on Pediatric emergency Department admissions. Nevertheless, as reported by Cousien et al. [34], there was no continuity with known trends, neither in seasonality over the period of the pandemic, nor in the percentages of suicidal crises recorded.
Conclusion and opening
New adolescent psychiatry unit, adolescent intensive outpatient center from the establishment specializing in psychiatry, and its partnership with Pediatric emergency Department from University hospital Center, would seem effective in reducing the risk of suicidal recidivism for adolescents in crisis. This specific adolescent unit would improve access to care for this suffering age group (the teenagers) and improve thus their prognosis. As a result, it would be highly likely that the regional coverage of the adolescent intensive outpatient center would help reduce the number of new admissions to the Pediatric emergency Department, and hence the number of repeat hospitalizations. These encouraging results obviously need to be confirmed and refined, and it would certainly be worthwhile to carry out a complementary, longer-term study to better assess the effects of treating teenagers in the adolescent intensive outpatient center, particularly in terms of suicide attempt recidivism. In any case, this adolescent intensive outpatient center would seem to represent a way forward for the prevention of suicidal recidivism, insofar as it articulates, complements and even synergizes the forces already mobilized around young people in distress. Further work is obviously needed to complete this study and refine the multidisciplinary management of young suicidal adolescents, with a view to the complementary project, the continuation of partnership: outpatient center - crisis beds - Pediatric emergency Department new challenges for tomorrow.
Declaration of interest
The authors declare that they have no conflicts of interest in relation to this article.
Authorship contribution statement
LC and APML thought first of the study while NC worked on adolescent project and the opening of the new child psychiatry unit. NC was the doctor in charge of the adolescent project and the new adolescent psychiatry unit.
LC, APML, and NC design the study.
LC, supervised by APML (pediatric aspect) and NC (child psychiatric aspect), carried out the recruitment, read all the medical files.
LC, APML and NC worked on data and analyzed results.
NC and LC wrote the article.
LC, APML and NC approved all the final work for submission.
Acknowledgments
The authors wish to thank firstly everyone involved in the adolescent project: members of management of the two hospitals (Mrs Bourrachot V., CHAI; Mrs Le Goff C., CHAI; Mr Baïetto J-M, GA-UH), members of Isere area (38), user representatives and all the partners of the adolescent project in the healthcare area : Child and adolescent psychiatry Department (CHAI) with Mrs Pagnier and all the multidisciplinary teams (doctors, educators, nurses, psychomotor therapists, psychologists), Pediatric Department of GA-UH (general pediatrics team and pediatric emergency team), professionals of Child and adolescent psychiatry Department of GA-UH, general practitioners in Isere area, etc
Secondly, the authors also wish to thank Doctor Egot A. from Clinical Research and Innovation Department of GA-UH; Doctor Provoost L., the head of the Pediatric emergency Department, for his access to data; the university professors who validated the path of the young doctor LC as Mrs Scolan V. (Forensic Pediatrics), Mr Debillon and Mr Mortamet (Pediatrics), Mrs Bioulac (Child and Adolescent Psychiatry); and Docteur Benayache R. for his participation in the medical thesis injury.
Finally, the authors thank the dedication of the care teams (in Pediatrics Department and of course in the new teen unit, the adolescent intensive outpatient center), but also the young patients, their parents and loved ones who, despite their often present moral suffering, accepted the study.
References
- National Institute of Mental Health, NIMH (2024). Mental Heal Informations. Suicide.
- World Health Organization, WHO (2014). Preventing suicide: a global imperative. World Health Organization.
- World Health Organization, WHO (2017). Mental health of adolescents. Key facts.
- World Health Organization, WHO (2023). Adolescent and young adult health. Key facts and mental health.
- Liu L, Villavicencio F, Yeung D, Perin J, Lopez G, et al. (2022) National, regional, and global causes of mortality in 5-19-year-olds from 2000 to 2019: a systematic analysis. Lancet Glob. Health 10 : e337-e347.
- Rey G (2017) Epidemiological data on deaths by suicide in France in 2017. Directorate of Research, Studies, Evaluation and Statistics DREES. National Institute of Health and Medical Research - Epidemiological Center for Medical Causes of Death.
- Regional Health Agency Auvergne-Rhône-Alpes: Mental health: Publication of the 10th bulletin “Suicide and attempted suicide in Auvergne-Rhône-Alpes". 2024 Fév 5. In French.
- French Observatory for Drugs and Drug Addiction, Public Health France (2021). Directorate of Research, Studies, Evaluation and Statistics DREES. Suicide attempts and suicidal thoughts among young French people - Results of the ESCAPAD 2014 and ESPAD 2015 surveys. 2021, France.
- Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, et al. (2020) Adolescent Psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res 291: 113264
- Alamolhoda SH, Zare E, Zadeh AH, Zalpour A, Vakili F, et al. (2022) Adolescent mental health during covid-19 pandemics: a systematic review. Int J Adolesc Med Health 35 : 41-60.
- Sheridan DC, Grusing S, Marshall R, Lin A, Hugues AR, et al. (2022) Changes in Suicidal Ingestion Among Preadolescent Children From 2000 to 2020. JAMA Pediatr 176 : 604-606.
- Berthou V, Boulch A, Carrière M, Guichard A, Hazo JB, et al. (2022) National Suicide Observatory - Suicide - Measuring the impact of the health crisis linked to Covid-19. Contrasted effects within the population and unease among young people. Report 5th. 2022 Sept, France.
- Chatagner A, Olliac B, Choquet LH, Botbol M, Raynaud JP (2015) Adolescents received urgently in infant and juvenile psychiatry. Who are they? What is their background? What social and/or judicial monitoring? Neuropsychiatr. Enfance Adolesc 63: 124-132.
- Yard E, Radhakrishan L, Ballesteros MF, Sheppard M, Gates A, et al. (2021) Emergency Department Visits for Suspected Suicide Attempts Among Persons Aged 12-25 Years Before and During the COVID-19 Pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 70 : 888-894.
- de Tournemire R (2010) Teenagers’ suicides and suicide attempts: finding one's way in epidemiologic data. Arch. Pediatr 7 : 1202-1209.
- Hawton K, Harriss L (2008) Deliberate self-harm by under-15-year-olds: characteristics, trends and outcome. J. Child. Psychol. Psychiatry 49 : 441-448.
- General Directorate of Care Offering (2019). Instruction DGOS/R4/2019/175 of 2019, July the 19th, relating to the modalities for allocating new measures in child and adolescent psychiatry for the year 2019. Ministry of health and Prevention. Health Official Bulletin. Social Protection.
- High health authority (2021) Suicidal ideation and behavior in children and adolescents: prevention, identification, assessment, management. Frontline healthcare workers. Recommend good practices. HAS Santé. Paris, France.
- Gerbeaux P, Bourrier P, Chéron G, Fourestié V, Goralski M, et al. (2001) Jacquet-Francillon M. Société Francophone de Médecine d’Urgence (SFMU). Implementation and management of Observation Units. JEUR 14: 144-152.
- High health authority (2021) Suicidal ideation and behavior in children and adolescents: prevention, detection, assessment, management. Hospital and 2nd line care. Recommend good practices. HAS Santé. Paris, France.
- Margret CP, Hilt R (2018) Evaluation and Management of Psychiatric Emergencies in Children. Pediatr Ann. 47 : e328-e333.
- Dolan MA, Fein JA (2011) Commitee on Pediatric Emergency Medicine. Pediatric and adolescent mental health emergencies in the emergency medical services system. Pediatrics 127 : e1356-1366.
- Shaffer D, Pfeffer CR and Work Group on Quality Issue, American Academy of Child and Adolescent Psychiatry (2001). Practice Parameter for the Assessment and Treatment of Children and Adolescents With Suicidal Behavior. J. Am. Acad. Child Adolesc. Psychiatry 40 : 24S-51S.
- Nistor N, Jitareanu C, Frasinariu OE, Ciomaga IM, Rugina AL, et al. (2017) Epidemiologic profile and triggering factors of voluntary poisoning in teenagers. Medicine (Baltimore) 96 : e5831.
- Roversi M, Martini M, Musolino A, Pisani M, Zampini G, et al. (2023) Drug self-poisoning in adolescents: A report of 267 cases. Toxicol Rep 10: 680-685.
- Becker M, Correll CU (2020) Suicidality in Childhood and Adolescence. Dtsch Aerzteblatt Int 117 : 261-267.
- De Luca M, Bonnichon D, Marty F (2012) Scarifications in adolescence, a suicidal equivalent. Psychiatry of Child. PUF 55 : 637-678.
- Charach A (2022) Editorial: Antibullying Initiatives and Suicide Prevention. J Am Acad Child Adolesc Psychiatry 61 : 1421-1422.
- Steare T, Gutiérrez Munoz C, Sullivan A, Lewis G (2023) The association between academic pressure and adolescent mental health problems: A systematic review. Journal of Affective Disorders 15: 339 :302-317.
- Bridge JA, Goldstein TR, Brent DA (2006) Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry 47 (3-4) : 372-394.
- Kreski NT, Chen O, Olfson M, Cerda M, Martins SS, et al. (2022) National Trends and Disparities in Bullying and Suicidal Behavior Across Demographic Subgroups of US Adolescents. J. Am. Acad. Child. Adolesc. Psychiatry 61 :1435-1444.
- Schonfeld A, McNiel D, Toyoshima T, Binder R (2023) Cyberbullying and Adolescent Suicide. J Am Acad Psychiatry Law 51 : 112-119.
- Cousien A, Acquaviva E, Kernéis S, Yazdanpanah Y, Delorme R (2021) Temporal Trends in Suicide Attempts Among Children in the Decade Before and During the COVID-19 Pandemic in Paris, France. JAMA Netw Open 4 : e2128611.
- Pierson K, Pereira Carvalho N, Shaker-Naeeni H (2021) 982 Impact of COVID-19 in the management of Under-16s presenting to the acute hospital with self-harm. in Abstracts A182.2-A183 Paediatric Mental Health Association 106(Suppl 1): A182.2-A183.
- Jardon V, Cleva E, Decoster S, Lamotte A, Debien C (2021) Preventing suicidal crisis and suicide. Rev Infirm. 70 : 29-31.
- Mendez-Bustos P, de Leon-Martinez V, Miret M, Baca-Garcia E, Lopez-Castroman J (2013) Suicide Reattempters: A Systematic Review. Harv. Rev. Psychiatry 21 : 281-295.
- Brent DA, Baugher M, Bridge J, Chen T, Chiappetta L (1999) Age- and Sex-Related Risk Factors for Adolescent Suicide. J Am Acad Child Adolesc Psychiatry 38 : 1497-505.
- Brent DA, Kolko DJ, Wartella ME, Boylan MB, Moritz G, et al. (1993) Adolescent Psychiatric Inpatients’ Risk of Suicide Attempt at 6-Month Follow-up. J Am Acad Child Adolesc Psychiatry 32 : 95-105.
- Spirito A, Valeri S, Boergers J, Donaldson D (2023) Predictors of Continued Suicidal Behavior in Adolescents Following a Suicide Attempt. J. Clin. Child Adolesc. Psychol 32 : 284-289.
- Consoli A, Cohen D, Bodeau N, Guilé JM, Mirkovic, et al. (2015) Risk and Protective Factors for Suicidality at 6-Month Follow-up in Adolescent Inpatients Who Attempted Suicide: An Exploratory Model. Can J Psychiatry 60 (2 Suppl 1): S27-36.
- Yen S, Weinstock LM, Andover MS, Sheets ES, Selby EA, et al. (2013) Prospective predictors of adolescent suicidality: 6-month post-hospitalization follow-up. Psychol Med 43: 983-993.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.