Neurointerventional Therapy for Giant Facial Haemangioma: Case Report and Literature Review
by Jian-Wei Huang1#, Hai-Yong He1#, Si-Cai Tao2#, Cong Ling1*, Shuang-Qi Gao1*, Ying Guo1*
1Departments of Neurosurgery, The Third Affiliated Hospital, Sun Yat-Sen University,Guangdong Province, 510630, Guangzhou, China
2Departments of Neurosurgery, The Third Affiliated Hospital, Sun Yat-Sen University·ZhaoQing Hospital, Guangdong Province, 526000, Zhaoqing, China
#Equally contributed authors.
*Corresponding author: Cong Ling, Departments of Neurosurgery, The Third Affiliated Hospital, Sun Yat-Sen University,Guangdong Province, 510630, Guangzhou, China; Shuang-Qi Gao, Departments of Neurosurgery, The Third Affiliated Hospital, Sun Yat-Sen University,Guangdong Province, 510630, Guangzhou, China; Ying Guo, Departments of Neurosurgery, The Third Affiliated Hospital, Sun Yat-Sen University,Guangdong Province, 510630, Guangzhou, China
Received Date: 16 August 2024
Accepted Date: 21 August 2024
Published Date: 23 August 2024
Citation: Huang JW, He HY, Tao SC, Ling C, Gao SQ, et al. (2024) Neurointerventional Therapy for Giant Facial Haemangioma: Case Report and Literature Review. J Surg 9: 11122 https://doi.org/10.29011/2575-9760.11122
Abstract
Backgrounds: Facial giant arteriovenous malformations are uncommon, with causes attributed to both inherited and acquired factors. The typical approach for treatment involves surgical excision and embolization.
Case presentation: Here, we report a patient in their 40s who had facial arteriovenous malformations that caused swelling of the eyelids and facial after two interventional embolization surgeries in an outpatient hospital. After a traumatic experience, the arteriovenous malformation grew rapidly and obscured the eye, so the patient came to our hospital and underwent a third interventional treatment while awaiting surgical resection. In addition, we reviewed the literature on facial arteriovenous malformations and provided an in-depth discussion of the status of facial arteriovenous malformations, including their causes, treatments, and outcomes. Conclusions: Giant facial arteriovenous malformations are rare, and the mechanism of their pathogenesis and rapid enlargement remains to be explored. Through a review of the literature, we found that trauma in these patients may be the mechanism of their onset and exacerbation, and vascular embolization alone is limited, and may be combined with surgical resection.
Keywords: Arteriovenous malformations; Embolism; Facial; Surgical excision
Introduction
Arteriovenous Malformations (AVMs) are an uncommon vascular anomaly that occurs during fetal development. They are characterized by abnormal connections between arteries and veins, bypassing the normal capillary network. AVMs account for a mere 1.5% of all vascular malformations and can be found in various regions, with the majority occurring within the brain. Extracranial arteriovenous malformations are rare, with 50% of cases found in the mouth and maxillofacial region [1]. Most of these anomalies are congenital, meaning they are present at birth [2], and can be caused by hormonal changes or acquired trauma [3]. Untreated, these disorders can result in significant physical and psychological ramifications. Common effects include regional swelling that is both unattractive and unpleasant. In severe instances, blindness and deadly hemorrhage may occur [4]. Typically, there are two categories of treatment for frontal facial Arteriovenous Malformation (AVM): 1. Surgical removal [5]. 2. Vascular interventional embolization refers to a medical procedure that involves blocking or obstructing blood vessels using specialized techniques [6]. 3. Administration of medications through injection directly into the lesion [7]. Due to the lesion's location in the frontal face, to prevent significant blood loss and disfiguring alterations to the patient's face, physicians and patients typically choose for vascular embolization in these cases [4]. Because AVMs often reoccur after incomplete resection or embolization, a combination of both treatment methods is now considered the optimum approach [8].
Case Presentation
The case involved a patient in their 40s who presented with erythema on the left side of face since birth. The patient also had a large mass on the left side of face that was noticeable and had increased skin temperature. The mass had a palpable pulsatile sensation but no signs of ulceration or bleeding. The patient received local treatment for the rapid growth of the tumor at a local hospital 6 years ago, but it was not effective. Four years ago, the patient underwent interventional treatment at the same hospital, which also did not yield significant results. Two years ago, the patient sought interventional treatment at other hospitals, but the specifics of the treatment are unknown. Unfortunately, the mass did not shrink after surgery. Over six months ago, the patient experienced an unintentional fall resulting in an injury to the left orbit. Since then, a mass in the left orbital area has been progressively growing, causing obstruction of the left eye (Figure 1). The patient is currently seeking additional medical care at the hospital.

Figure 1: Anterior side of the patient: a large mass may be seen completely occluding the patient's left eye.
Imaging Examination
The CT and MR scans revealed the presence of several abnormal blood vessel formations in various areas including the nose, left eye area, upper jaw and face, temporal region, lower temporal region, space behind the throat, and space around the salivary gland. These formations surround the left eyeball and affect the left eye socket, cheekbone, and sphenoid bone (Figure 2). The patient has bilateral cavernous sinus and left supraocular vein reflux, along with the presence of coils in several locations. Additionally, there is an aberrant thickening of the trunk and branches of the left internal carotid artery, as seen in (Figure 3).
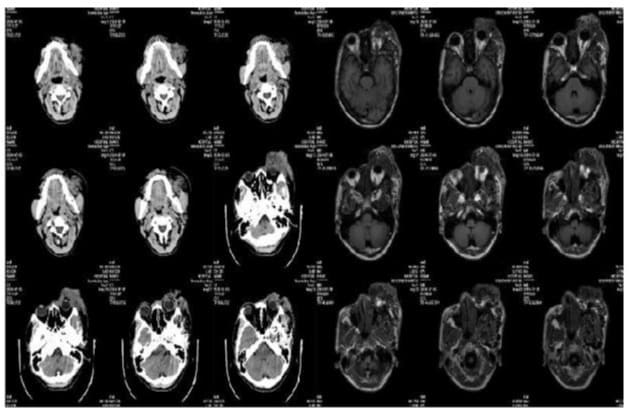
Figure 2: The left side is the CT of the patient, and the right side is MR image: the nasal, left periorbital, maxillofacial area, part, temporal fossa, inferior temporal fossa, parapharyngeal space, and parotid gland space showed multiple tortuous tubular vascular shadows, and the enhanced scan showed vascular-like enhancement, and the tortuous perivascular and vascular space showed flaky soft tissue shadows, the boundary was unclear, and the overall large layer of the lesion was about 83x52x42 mm (not fully encapsulated), and the lesion surrounded the left eyeball, involving the left orbit, zygomatic bone, and sphenoid wing.
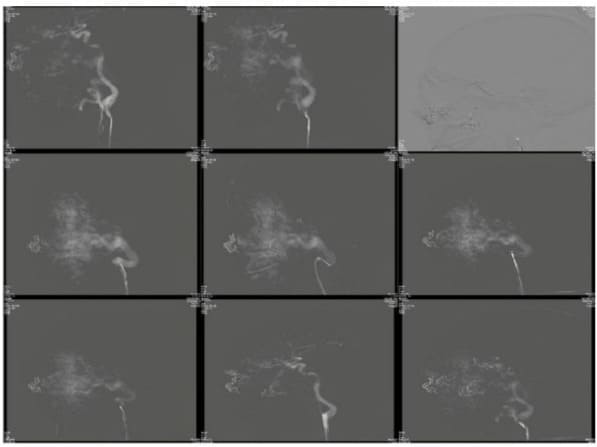
Figure 3: DSA on admission for the first time: the left orbit and the surrounding huge contrast agent concentration area can be seen, the blood vessels are very abundant, mainly supplied by multiple branch blood vessels of the left external carotid artery, and a small part is supplied by the left ophthalmic artery, the flow is very large, and the flow is very large, and the return to the bilateral cavernous sinus and the left superior ocular vein, spring coils can be seen in many places, and the main trunk and branches of the left internal carotid artery are abnormally thickened.
Surgical Procedures
Due to the large size of the facial arteriovenous malformation and the risk of severe bleeding, the third operation opted for vascular intervention to block the blood supply vessel and perform DSA (digital subtraction angiography) first. This involved placing a catheter system with a 6F distal access catheter into the left external carotid artery trunk. A balloon catheter system was then inserted into a branch of the left external carotid artery using a guidewire. The balloon was inflated to block the blood supply artery and a total of 8 liquid embolic systems were slowly injected until it was suspected to have entered the vein. Subsequent imaging revealed a 15% decrease in blood flow to the tumor. Once the balloon is deflated, it is extracted using negative pressure retraction. Furthermore, the occlusion balloon catheter system was directed towards an alternative blood supply branch, and the blood supply artery branch was obstructed using four liquid embolization systems. Subsequent imaging revealed a decrease of around 30% in the blood flow to the tumor (Figure 4).
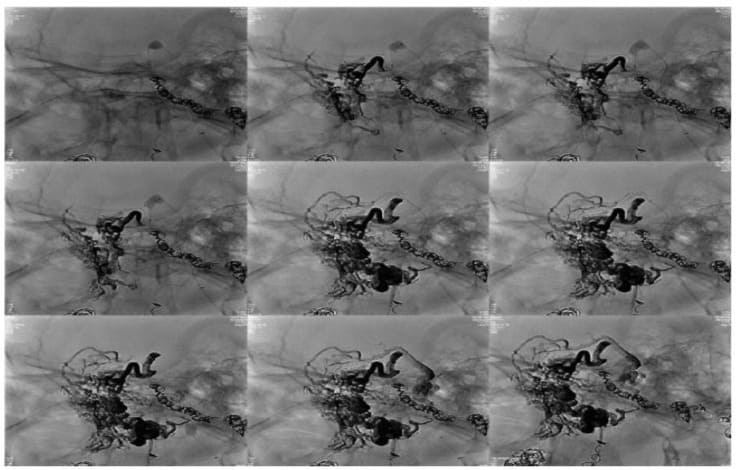
Figure 4: Intraoperative DSA for left-sided giant arteriovenous malformation: significant reduction in blood flow after embolization of the supplying vessels.
Result
Post-operatively, the patient reported no notable discomfort. The Digital Subtraction Angiography (DSA) revealed a substantial decrease in blood flow to the mass. A follow-up examination of the lump is scheduled for one month after the surgery. If there is a considerable reduction in size, it will be surgically excised.
Discussion
An Arteriovenous Malformation (AVM) is a structural vascular abnormality that generally does not have a cellular component proliferation, but histologically, the nodule shows that the proliferating cellular area is composed of endothelial cells and pericytes in addition to the dilated vascular area, and due to the proliferation of these cells, the lesion site is constantly expanding [9].The cause may be attributed to either a congenital developmental defect or an acquired trauma.Maxillofacial arteriovenous malformations can be categorized based on their location into cheeks [10,11], eyelids [12,13], nose [1,14], maxillary [15,16] mandibular arteriovenous malformations [6,17,18] The symptoms and treatment procedures vary depending on the specific site. Occasionally, this condition can manifest in numerous locations simultaneously, leading to widespread lesions. In this particular case, the patient experienced this condition in both the upper jaw and eyelids, resulting in a significant face arteriovenous malformation that impaired their vision. Due to the rarity of this extracranial arteriovenous malformation, there is no standardized treatment approach. The current main treatment options include surgical resection and embolization. Embolization can be further categorized into local injection embolization and endovascular interventional embolization. The choice of treatment method depends on the specific condition of each patient. To determine the appropriate treatment method for arteriovenous malformations in different areas, a thorough search was conducted in the National Library of Medicine. The search yielded a total of 15 reported cases of facial arteriovenous malformations, with only one case classified as a giant facial arteriovenous malformation (as shown in Figure 5). Based on the data presented in the table, it is evident that both simple surgical resection and embolization yield favorable treatment outcomes. However, in this particular case, the patient who had previously undergone two interventional embolization surgeries experienced a relapse. Additionally, due to trauma, the mass rapidly grew, resulting in the patient losing their vision. This demonstrates that the efficacy of simple interventional embolization is actually limited. In contrast, surgical resection following embolization proves to be more effective for patients in similar situations. It is noteworthy that two patients in the table have a prior history of trauma at the same site before the enlargement, which aligns with the findings of this case. Trauma may be the reason for the rapid growth of arteriovenous malformation, possibly due to the release of different growth factors in the blood vessels caused by injury. However, further research is necessary to investigate the mechanism.

Figure 5: Summary of 15 patients with facial arteriovenous malformation.
Conclusions
Giant facial arteriovenous malformations are rare, and the mechanism of their pathogenesis and rapid enlargement remains to be explored. Through a review of the literature, we found that trauma in these patients may be the mechanism of their onset and exacerbation, and vascular embolization alone is limited, and may be combined with surgical resection.
References
- Neeta S, Rao R, Upadya M, Keerthi P (2017) Arteriovenous Malformation of Face: A Challenge to Anesthesiologists. Anesthesia, essays and researches 11: 784-786.
- Alsabbagh BM, Alfaqeeh FA, Ajlan AM, Yaghmoor F, Essbaiheen F, et al. (2021) Arteriovenous Malformation of the Upper Eyelid: A Case Report. Plastic and reconstructive surgery Global open 9: e3609.
- Kao ST, Walker PW, Ferguson HW (2014) Posttraumatic arteriovenous malformation of the face: a case report. The Journal of emergency medicine 46: e5-8.
- Meila D, Grieb D, Greling B (2017) Endovascular treatment of head and neck arteriovenous malformations: long-term angiographic and quality of life results. Journal of neurointerventional surgery 9: 860-866.
- Tiwari R, Singh VK (2015) Arterio venous malformation of the face: surgical treatment. Journal of maxillofacial and oral surgery 14: 25-31.
- Loureiro CC, Falchet PC, Gavranich J, Lobo Leandro LF (2010) Embolization as the treatment for a life-threatening mandibular arteriovenous malformation. The Journal of craniofacial surgery 21: 380-382.
- Zheng JW, Yang XJ, Wang YA, He Y, Ye WM, et al. (2009) Intralesional injection of Pingyangmycin for vascular malformations in oral and maxillofacial regions: an evaluation of 297 consecutive patients. Oral oncology 45: 872-876.
- Kansy K, Bodem J, Engel M (2018) Interdisciplinary treatment algorithm for facial high-flow arteriovenous malformations, and review of the literature. Journal of cranio-maxillo-facial surgery : official publication of the European Association for Cranio-Maxillo-Facial Surgery 46: 765-772.
- Yasuda M, Okada E, Nagai Y, Tamura A, Ishikawa O (2010) Reactive proliferation of endothelial cells and pericytes associated with arteriovenous malformation. The Journal of dermatology 37: 363-366.
- Hunasgi S, Koneru A, Vanishree M, Manvikar V (2019) Giant arteriovenous malformation of the face and upper lip. Journal of oral and maxillofacial pathology : JOMFP 23: 32-35.
- Kumar A, Mittal M, Srivastava D, Jaetli V, Chaudhary S (2017) Arteriovenous Malformation of Face. Contemporary clinical dentistry 8: 482-484.
- Tsui E, Dunbar KE, Kim ET, Patel P (2020) Staged embolization and excision of an arteriovenous malformation involving the eyelid and orbit. Orbit (Amsterdam, Netherlands) 39: 71-72.
- Marchal A, Weber M, Le Meur G, Lebranchu P, Vabres B (2019) [Arteriovenous malformation of orbit and eyelid: case report]. Journal francais d'ophtalmologie 42: e261-e262.
- Chen J, Dou J, Han Z, Liang P (2023) Microwave Ablation for Refractory Giant Maxillofacial Arteriovenous Malformation: A Case Report. The Laryngoscope 133: 2984-2987.
- Ariboyina AK, Tatli O, Goriparthi L, Achanta N, Thirumoothy SK, et al. (2023) Arteriovenous malformation presenting as a lip swelling. Clinical case reports 11: e7736.
- Churojana A, Khumtong R, Songsaeng D, Chongkolwatana C, Suthipongchai S (2012) Life-threatening arteriovenous malformation of the maxillomandibular region and treatment outcomes. Interventional neuroradiology : journal of peritherapeutic neuroradiology, surgical procedures and related neurosciences 18: 49-59.
- Housley SB, Cappuzzo JM, Waqas M, Levy EI (2022) Facial Arteriovenous Malformation Embolized Using n-Butyl-2 Cyanoacrylate and Contrast Stasis Rather Than Tantalum Powder with Double Flow Arrest to Prevent Skin Discoloration: A Technical Note. World neurosurgery 164: 350-352.
- Blackhall KK, Ling E, Kunjur J (2020) A rare case of a intraosseous arteriovenous malformation of the temporomandibular joint and mandible - Case report and literature review. International journal of surgery case reports 76: 394-398.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.