Navigating the Uncommon: A Case of Isolated Pulmonary Metastasis in Prostate Cancer
by Abdul Mannan, Yasir Umar Khawaja, Muhammad Mohsin Zahoor*, Hussain Noon, Hira Gul, Brian Casserly
Respiratory department, University Hospital Limerick, Limerick, Ireland
*Corresponding author: Muhammad Mohsin Zahoor, Respiratory department, University Hospital Limerick, Limerick, Ireland
Received Date: 15 August 2025
Accepted Date: 19 August 2025
Published Date: 21 August 2025
Citation: Mannan A, Umar YK, Mohsin MZ, Noon H, Gul H, et al. (2025). Navigating the Uncommon: A Case of Isolated Pulmonary Metastasis in Prostate Cancer. Ann Case Report. 10: 2381. https://doi.org/10.29011/2574-7754.102381
Abstract
Prostate cancer frequently metastasizes to various organs, with pulmonary involvement occurring in over 40% of cases. However, isolated pulmonary metastasis is rare, occurring in less than 1% of cases. This report presents a case of a 67-year-old male diagnosed with a high Gleason score (8) but negative PSA adenocarcinoma of the prostate in 2017. The patient underwent robotic-assisted radical prostatectomy and pelvic lymph node dissection in July 2017, followed by adjuvant radiotherapy and one year of androgen deprivation therapy (ADT), completed in September 2018. After a period of disease remission, a follow-up appointment with persistently negative but mildly raised prostate-specific antigen (PSA) levels and a doubling time under six months indicated biochemical failure. PET imaging revealed a solitary right lung nodule with low standardized uptake value (SUV max). Follow-up CT showed interval growth, raising suspicion of a primary lung malignancy. Biopsy confirmed metastatic prostate cancer. This case highlights the exceptional rarity of isolated pulmonary metastasis in prostate cancer and underscores the need for vigilant follow-up and thorough diagnostic evaluation.
Keywords: Prostate Cancer; Isolated Pulmonary Metastasis; PSANegative; Metastasectomy; Case Report.
Introduction
Prostate cancer is the second most common malignancy in men worldwide, frequently spreading to bone and lymph nodes. Pulmonary involvement is observed in over 40% of metastatic cases, but isolated pulmonary metastasis—without concurrent dissemination—is exceedingly rare, reported in less than 1% of cases [1]. In a study of 1290 prostate cancer patients, 48 exhibited lung metastases and only 11 (0.86%) had solitary pulmonary nodules [2]. Here, we present a rare case of PSA-negative prostate cancer presenting years later with an isolated pulmonary metastasis confirmed by biopsy. The patient provided verbal consent for publication of clinical details and associated images.
Case Presentation
A 67-year-old male ex-smoker (15 pack-year history) was diagnosed in 2017 with adenocarcinoma of the prostate, staged pT3bN0R0, Gleason score 4+4=8. He underwent roboticassisted radical prostatectomy and pelvic lymph node dissection, followed by adjuvant radiotherapy and a one-year course of androgen deprivation therapy (ADT), completed in September 2018. During routine surveillance, his PSA level rose to 1.53-still within the “undetectable” threshold but higher than baseline. His PSA doubling time was calculated at 5.2 months. GnRH agonist (Leuprolide) therapy was restarted and metastatic work-up initiated.
A CT thorax revealed a solitary apical right lung nodule measuring 8 mm. PET scan showed faint FDG avidity with an SUV max of 1.1 and no other metastatic lesions. Repeat CT after six months showed interval growth of the nodule to 12 mm (Figure 1, 2).
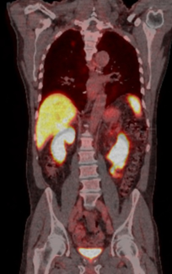
Figure 1: PET CT shows faint FDG avid in right upper lobe.
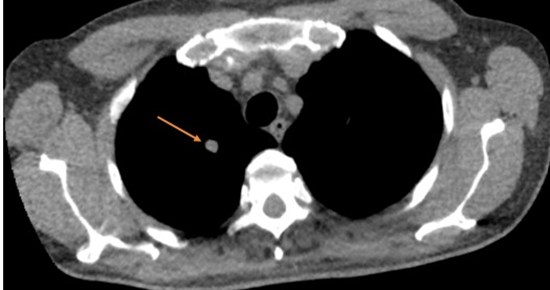
Figure 2: CT thorax Shows 12 mm solid nodule on right upper lobe
Multidisciplinary discussion recommended surgical biopsy. Therefore, CT guided biopsy of right upper lobe nodule taken. Histology confirmed metastatic prostate adenocarcinoma: tumour cells were positive for PSA and negative for TTF-1, CD56, chromogranin, and synaptophysin, with morphology consistent with prostatic origin (Figure 3).
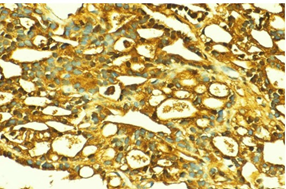
Figure 3: Immunohistochemical staining of the lung biopsy showing strong cytoplasmic positivity for prostate-specific antigen (PSA), confirming metastatic prostate adenocarcinoma. The brown staining highlights malignant glandular cells infiltrating lung parenchyma.
The case was discussed in MDM again and planned for urgent surgery. The patient underwent VATS resection of the right upper lobe. He made a full recovery, maintained weight (77 kg), and had an ECOG score of 0. His PSA dropped from 0.13 preoperatively to <0.03 within two weeks’ post-op, likely reflecting a combined effect of metastasectomy and Leuprolide.
Discussion
Pulmonary metastasis in prostate cancer typically occurs in widespread disease via hematogenous dissemination [2]. Isolated pulmonary lesions are clinical anomalies and may be misdiagnosed as primary lung cancer or benign nodules [1,3]. This patient’s nodule demonstrated low metabolic activity, further obscuring suspicion for malignancy.
Importantly, PSA-negative prostate adenocarcinoma complicates standard surveillance algorithms. PSA remains a key biomarker, but in rare cases such as this, imaging and histology are essential for accurate detection and staging [4]. The delayed onset of metastasis nearly six years after curative therapy highlights the need for long-term follow-up in high-risk patients regardless of PSA status [2].
Biopsy and immunohistochemistry were vital to distinguish primary lung cancer from metastatic prostate cancer-especially given the lesion’s faint FDG activity. Pathology confirmed its origin based on PSA positivity and prostate-specific morphological features [4,5]. After metastasectomy, undetectable PSA and stable clinical parameters suggested both therapeutic benefit and effective systemic control.
Treatment decisions in solitary metastasis remain nuanced. While ADT is standard for systemic recurrence, localized interventions such as surgery or stereotactic, radiotherapy may improve outcomes in select patients [6]. This case supports the integration of metastasectomy as a viable option when feasible, particularly in well-performing patients.
Conclusion
This case illustrates the rare occurrence of solitary pulmonary metastasis in a patient with high-grade, PSA-negative prostate cancer. It calls attention to the limitations of relying solely on PSA for monitoring and stresses the importance of advanced imaging and histopathological confirmation. Management of atypical metastasis requires a tailored, multidisciplinary approach-balancing systemic therapy with localized interventions. As prostate cancer follow-up extends years beyond initial therapy, clinicians must remain alert to late-stage unusual presentations. This report adds to the evolving understanding of metastatic pathways and guides future evaluation of solitary pulmonary lesions in prostate cancer survivors.
Conflict of Interest: We as authors declare that there is no conflict of interest regarding the publication of this article.
Patient Consent: Written informed consent was obtained from the patient for the publication of their clinical details and any accompanying images. The patient was informed that efforts would be made to conceal their identity, but anonymity could not be guaranteed. A signed copy of the consent form is available and can be provided to the journal upon request.
References
- Maru N, Ishikawa T, Nakano K, Utsumi T, et al. (2021) Solitary lung metastasis from primary prostate cancer with normal PSA levels: A case report. World Academy of Sciences Journal. 3: 74-78.
- Gee JR, Libertino JA. (2021) Multimodal therapy for high-risk prostate cancer with long-term follow-up. Int J Clin Oncol. 6: 125-129.
- Gemalmaz H, Gunaydin O, Demirci M, Çulhac N, et al. (2021) Isolated pulmonary metastasis metastasectomy after curative prostate cancer treatment. Bulletin of Urooncology. 20: 270-272.
- Shindo K, Fujimoto K, Akiyama Y, Moriyama T, et al. (2020) A rare case of PSA-negative metastasized prostate cancer to the stomach. Surgical Case Reports. 6: 234.
- Bratt O, Auvinen A, Godtman RA, Hellström M, Hugosson J, et al. (2023) Screening for prostate cancer: evidence and knowledge gaps. BMJ Oncology. 2: e000142.
- Watanabe K, Taira AV, Lin Y, Ikeda N, et al. (2025) Long-term outcomes of salvage HDR brachytherapy for prostate cancer recurrence. BMC Cancer. 25: 317.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.