Multidisciplinary Diabetic Foot Clinic Initiative in A High-Volume Irish Tertiary Referral Center: A Quality Improvement Project
by Elkady R.1, Sevastianova K.2, Gallagher T.3, O’Donoghue A3, Kellegher E3, Cornally D.1, Hetmanau D.1, Ward P.4, Callanan I.5, Hurley H.1, Canavan R.6, Walsh S.R.7, Dowdall J.1, Feeney E.2, Barry M.1.
- Vascular surgery department, St. Vincent’s University Hospital, Dublin, Ireland.
- Infectious disease department, St. Vincent’s University Hospital, Dublin, Ireland.
- Podiatry department, St. Vincent’s University Hospital, Dublin, Ireland.
- Ability Maters, Orthotics, Dublin, Ireland.
- Clinical Audit department, St. Vincent’s University Hospital, Dublin, Ireland.
- Endocrinology department, St. Vincent’s Hospital Group, Dublin, Ireland.
- Lambe Institute for Translational Research, Discipline of Surgery, University of Galway, Galway, Ireland.
*Corresponding author: Ramy Elkady, Department of Vascular Surgery, St. Vincent’s university Hospital, Dublin, Ireland
Received Date: 11 December 2024
Accepted Date: 16 December 2024
Published Date: 18 December 2024
Citation: Elkady R, Sevastianova K, Gallen T, O’Donoghue A, Kellegher E, et al. (2024) Multidisciplinary Diabetic Foot Clinic Initiative in A High-Volume Irish Tertiary Referral Center: A Quality Improvement Project. J Surg 9: 11212 https://doi.org/10.29011/2575-9760.011212
Abstract:
Introduction: Diabetic foot disease is a complex multifactorial pathology that constitutes a large burden for both patients and physicians. It’s complications also places a substantial burden on the patient’s family. (1) The current set up in SVUH is very encouraging to set the foundation for a multidisciplinary team (MDT) input for this challenging cohort of patients.
Methodology: We aimed to set up an MDT diabetic foot clinic (DFC) utilizing the variety of disciplines available in our center. A formal email that invited the potential teams and a meeting to discuss the options available was convened. The project was met with great interest from the different team representatives. The Outpatient Antimicrobial Therapy (OPAT) clinic was chosen to incorporate the MDT DFC. This clinic is already set up for wound review and has some members from the teams needed to set up the clinic, so that with some minor adjustments it can encompass the full MDT foot care service.
Results: From January 2023 to July 2023, 26 clinic sessions were held. 31 patients were reviewed in the MDT DFC. 9 patients achieved complete wound healing (29%). Sixteen patients were changed to a chronic wound without a surgical intervention (52%). Three patients required minor amputation (10%). Nine patients had significant peripheral arterial disease (29%) (Mean absolute toe pressure of 36 mmHg) out of which, 6 had reconstructible options and underwent balloon angioplasty. New endocrinology referrals were sent for 6 patients (19%). Referrals were made to treating endocrinologists if the patients were found to have a poor glycemic control. Twelve new referrals were made for custom made footwear (39%).
Conclusion: We believe that as an initiative, the MDT DFC is a project that is showing great potential in a large volume center as SVUH. This would encourage to expand and formalize the project.
Keywords: Multidisiplinary care, MDT, Diabetic foot clinic, Diabetic foot ulcer, Lower limb salvage.
Introduction
Diabetic foot disease is a complex multifactorial pathology that is constitutes a large burden for both patient and physician and places a substantial burden on the patient’s family, and service providers [1]. St. Vincent’s University Hospital (SVUH) is a 600-bed tertiary referral center. Vascular services receive referrals from the local catchment area in South Dublin in addition to the 4 peripheral referring hospitals serving a total population of 1.1 million. This leads to a large number of daily referrals of patients with diabetic foot disease. Management of this large population of diabetic patients has proved challenging in terms of coordinating in-patient and follow-up out-patient care in a multi-disciplinary setting. The International Working group on Diabetic foot Guidelines (IWGDF) in 2023 have emphasized on the importance of interdisciplinary foot care clinics in reducing the risk of major and minor diabetesrelated lower extremity amputation [1]. Previous experience with establishing a multi-disciplinary diabetic foot clinic in St. Vincent’s University Hospital proved helpful in establishing this new venture. The teams include Vascular surgery, Infectious disease (ID), Endocrinology, Outpatient Parenteral Antimicrobial Therapy (OPAT), Podiatry, Tissue viability, Vascular Advanced Nurse Practitioner (ANP) and Orthotics.
Aim
To establish an ambulatory multi-disciplinary diabetic foot clinic where the patient can be seen by all specialties on a single visit.
Methodology
The process of establishing the multi-disciplinary clinic started began by gauging the interest of all the members of the MDT. Interest among the involved specialties was gauged by e-mail invitation to a formal meeting to discuss the feasibility of the proposed clinic.
The suggested project was met with great interest from the different team representatives. On completion of all the meetings with the different stake holders, a few challenges were anticipated.
Allocating a day and time for the clinic became one of the most challenging issues. As a busy public hospital, adding an extra slot for a new clinic would not be an easy task, as most teams are already running a tight schedule, not to mention the need for administrative and clerical support. Furthermore, the outcomes and benefits from such clinics need to be clearly identified to avoid duplication of existing services. It was also important to accurately identify the target patient population to be served by the MDT clinic. It was suggested that as an initiative, we start with small patient numbers and then consider expansion of this service after trialing the project and identifying additional needs. A suggestion by the ID team that the clinic be incorporated within the weekly Outpatient Antimicrobial Therapy (OPAT) clinic was implemented. This clinic was already set up for management of diabetic foot ulcer (DFU) patients and already incorporated a wound review service and many of the staff involved in the care of DFU patients. Therefore, with the addition of more members of the involved teams it was possible to provide a comprehensive MDT foot care service.
Intervention
The following teams were involved in setting up the diabetic foot ulcer multi-disciplinary clinic: Vascular Surgery, Vascular Advanced Nurse Practitioner (ANP), Infectious disease, Endocrinology, Podiatry, Orthotics.
Template: A template was designed to input the patient’s data from each visit to ensure that no information is missing and to be used to track the progress made during the treatment. This template was completed for each patient every time they visited the clinic (Figure 1).
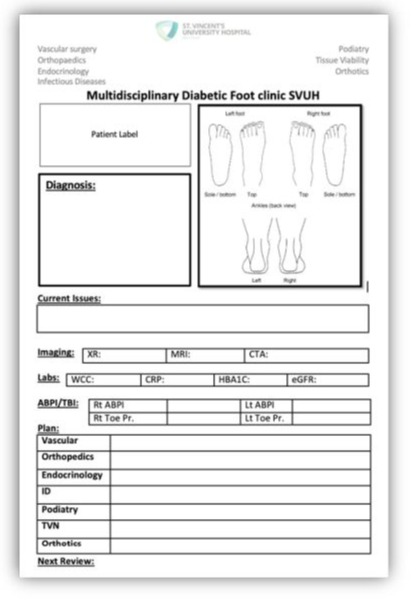
Figure 1: MDT DFC Template for each patient visit.
PICO
Population: Patients with a DF infection (DFI)/ Ulcer (DFU) who are receiving long-term antibiotics for treatment of osteomyelitis (intravenous or oral) with or without a previous surgical intervention.
Intervention: Interdisciplinary footcare from different specialties (OPAT, wound management, revascularization, risk factor control, patient education, prevention of new wound related complications and optimization to achieve wound healing).
Comparator: the number of patient episodes in the vascular outpatient department (OPD) at the same time interval of the year before the MDT DFC was running.
Outcomes
- Rapid access clinic: this is achieved by initiating treatment as inpatients and then discharging the patients followed by an early review (within 14 days) in the MDT DFC. This is then followed by either a weekly or a fortnightly review.
- Early identification of patients who are failing OPAT: Patients who are showing clinical deterioration or no sign of improvement despite the optimal antimicrobial administration.
- Reducing the number of patient visits to the hospital to the different disciplines as the cases can be seen by different specialties at once.
- Easier communication between teams as the different team members meet and review the patient together and can make a joint decision and have that documented on the template form for the following visit.
- Clear information for the patients from the different specialties which can involve patient education regarding optimization and a clear understanding of the course of treatment.
- Limb/ Foot salvage: utilizing the above-mentioned outcomes and resources to reduce major adverse limb events (MALE) including above and below knee amputation.
Results
From January 2023 to July 2023, 26 clinic sessions were held (2-3 hours each session), 31 patients were reviewed in the MDT DFC (a total of 92 episodes of attendance during that period). These were patients who were initiated on intravenous antibiotics for treatment of osteomyelitis with or without a surgical intervention, the majority of which started as inpatients. Ten patients (32%) had undergone a previous amputation with remnant infection at the surgical site or in the proximal bone. Two patients (6%) were not on antibiotics but were deemed high risk patients for wound related complications and would benefit from the MDT input. Both patients benefited significantly from the early review (one was a newly diagnosed type 2 diabetic, who was still not familiar with managing his blood sugar levels and his glucose monitor, and this was significantly impacting wound healing. Through his attendance at the MDT DFC the patient was seen by the specialist DM nurse who educated the patient regarding glycemic control, managing his glucose monitor and educated on what to do if his glucose levels are high and medication adjustment is needed).
Over the course of six months of the MDT DFC, 9 patients achieved complete wound healing (29%) For sixteen patients their wound progressed to become a chronic wound and did not proceed to a surgical intervention (52%). These patients had either declined a surgical procedure or had no revascularization options and had started to show signs of healing despite impaired perfusion. Three patients required minor amputation (10%) (Failing OPAT). Nine patients (29%) had significant peripheral arterial disease (Mean absolute toe pressure of 36 mmHg) of whom, 6 had reconstruction options and underwent a successful plain balloon angioplasty procedure. Three patients (10%) were not diabetic but had complex foot pathology and were seen in the complex foot clinic to try and optimize their healing and achieve better outcomes.
Strict glycemic control is essential to achieving wound healing in DFU. HbA1c was checked for the patients attending the clinic and patients were referred to an endocrinologist if they were found to have an undiagnosed high HbA1c (>42). New endocrinology referrals were sent for 6 patients (19%). Referrals were also made to the current treating endocrinologists in the hospital group if the patients were found to have a poor glycemic control.
With regards to orthotics, patients whose wounds were healing were referred to the appropriate pathway for custom-made footwear. A total of 12 (39%) new referrals were made to the local suppliers or in the case of a full trans-metatarsal amputation to the National Rehabilitation Hospital (Tables 1,2).
|
Completely healed |
9 (29%) |
|
Chronic wound |
16 (52%) |
|
Minor amputation (Failing OPAT) |
3 (10%) |
|
Ischemic |
9 (29%) |
|
Revascularization (Angioplasty) |
6 (19%) |
|
Non-Diabetic but complex foot pathology |
3 (10%) |
|
New referral to Endocrinology |
6 (19%) |
|
New referral to Orthotics |
12 (39%) |
Table 1: Results.
|
Jan to July 2022 |
Jan to July 2023 (MDT clinic) |
|
|
No. of patients attending OPAT clinic |
76 |
108 (increase by 42%) |
|
No. of patients attending Vascular OPD |
333 |
377 (increased by 13%) |
Table 2: The comparator: The Number of patient episodes in OPD for six months 2022 vs 2023.
Discussion
The establishment of a MDT DFC in St. Vincent’s University Hospital helped to enrich the communication between the different disciplines involved in the care of the diabetic patient. The presence of the different stake holders, all at the same time reviewing each patient, helped to rationalize the clinical decisions being made. As a result, there were no delays in terms of identification of the patients who were failing antimicrobial management alone and require surgical intervention. Another major advantage of multi-disciplinary working was the MDT input for complex cases with delayed healing and no revascularization options. For those patients with limited surgical or endovascular options, open discussion between all involved clinicians reassured both patient and teams that all possible treatment options had been exhausted. The consistent feedback from all clinicians involved also served to provide reassurance to patients and their relatives.
One of the main aims of this project, was to improve continuity of care. The template developed in the course of this project had a significant role in achieving this target. The template was short, therefore not time consuming to fill, yet precise. From one form, all the relevant up to date information can be collected, and this aided in the decision-making process as it demonstrated the progress being made from the perspective of each of the involved disciplines. It also served purpose of being a data collection form for future research. The forms were scanned after every clinic and circulated to all team members though the hospital email. This helped update all teams with the outcomes and helped populate an online database through the email. This pilot project identified the possible utilization of this clinic as a rapid access complex foot clinic. As the project became more established, the MDT DFC assisted in earlier discharges for complex cases as the close MDT surveillance that was offered in the clinic helped function as a safety net for those patients who are at higher risk of deterioration.
The comparison between the number of patient episodes between 2022 and 2023 showed some interesting findings. A significant increase in the number of DF patient episodes in the OPAT clinic from January to July 2023 (The MDT DFC), this reflected on a reduction in the percentage increase in the number of patients attending the general Vascular OPD (13% compared to 42%) (Table 2). When we assessed the overall service and compared 2022 to 2023, we found an overall rise in the numbers. Part of the rise in the numbers was attributed to the services being back to full capacity after the COVID-19 pandemic, as winter of 2022 was a period that the health services in Ireland were still impacted by the pandemic. We concluded that the MDT DFC led to a relative reduction in the number of patients attending the general vascular OPD and we predict that if this project was not running, we would have expected a higher percentage increase in the numbers in the vascular OPD. We also predict that if this service was given more capacity, it would have caused an absolute reduction in patient foot fall to the hospital. We believe that the role of managerial support for such projects is one the most important pillars to help achieve the set targets. Having the appropriate settings, available staff, and above all adequate resources would have aided this project to achieve more of the set targets. There were some limitations to this project. The first and the most challenging, was the absence of a specialized foot and ankle surgeon from the MDT team. The role of foot reconstruction in diabetic foot disease is difficult to overstate. We believed that this would be one of the important pillars of the MDT DFC, specifically to achieve more foot salvage and reconstruction. The IWGDF suggests a level 2 care diabetic foot service should involve an orthopedic surgeon [2]. We are currently addressing this deficit.
Another major challenge was consistent availability of qualified staff. Like many public hospitals, the different departments are not adequately staffed to meet the increasing demands of diabetic foot management. This deficit became more obvious during periods of staff sick leave or annual leave. Finally, the process of filling the template paper form, followed by the need to scan and e-mail it for distribution was time-consuming and tedious. It also risked missing data points. This could be improved by incorporating an electronic version of the template into the clinical portal of the hospital data management system which would allow it to be searchable and immediately available.
Conclusion
This pilot project was a success in identifying the potential for a formalized multi-disciplinary foot clinic to manage diabetic foot complications in a large volume tertiary referral centre such as St. Vincent’s University Hospital. Ultimately, we believe that will result in better limb preservation with fewer major lower limb amputations. The future plan would be to design a business case to formalize and resource the project on all levels. This could be achieved by providing the clinic with a dedicated geographical base and time slot supported by the requisite administrative and clerical staff to ensure its efficiency and success.
Figure 2: Painting of the different team members in the MDT DFC sketched by one of our patients as a sign of appreciation of the team’s effort in the clinic.
References
- Bus SA, Sacco ICN, Monteiro-Soares M, Raspovic A, Paton J, et al. (2023) Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2023 update). Diab Metab Res Rev 2023; e3651.
- Senneville É, Albalawi Z, Van Asten SA, Abbas ZG, Allison G, et al. (2023) Guidelines on the diagnosis and treatment of foot infection in persons with diabetes (IWGDF/IDSA 2023). Diab Metab Res Rev 2023.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.