Motivation in Primary Care Physicians: A Theoretical Approach to the Dimensions and Indicators of Work Motivation in Catalonia, Spain
by Adriana Florez Uribe1*, Esperanza Villar Hoz2
1Primary Care Physician – Hospital of Palamós-SSIBE, PhD Student - University of Girona, Palamós, Girona, Catalonia, Spain
2Associate professor at the Faculty of Psychology, University of Girona, Girona, Catalonia, Spain
*Corresponding author: Adriana Florez Uribe, Primary Care Physician – Hospital of Palamós-SSIBE, PhD Student - University of Girona, Palamós, Girona, Catalonia, Spain
Received Date: 21 August, 2025
Accepted Date: 30 August, 2025
Published Date: 04 September, 2025
Citation: Florez A, Villar-Hoz E (2025) Motivation in Primary Care Physicians: A Theoretical Approach to the Dimensions and Indicators of Work Motivation in Catalonia, Spain. J Family Med Prim Care Open Acc 9: 289. https://doi.org/10.29011/2688-7460.100289
Abstract
Background: Retention of Primary Care Physicians (PCPs) is increasingly difficult, with many facing burnout and declining motivation. Motivation, while widely studied in occupational psychology, remains underexplored in primary healthcare settings. Aim: This study aimed to: (1) identify the motivational dimensions and indicators described in the scientific literature, and (2) explore the perceptions of healthcare managers regarding PCP motivation within the Catalan health system. Design & setting: A two-phase exploratory study combining a scoping review with a qualitative survey of healthcare managers in Catalonia, Spain. Method: The scoping review followed JBI and PRISMA guidelines, including 21 studies from 2000 onwards. The survey included open-ended questions sent to 24 managers; 9 responded. Thematic analysis was used to identify motivational indicators and systemic influences. Results: The literature identified three motivational indicators: goal-directed activity, affective impact, and personal values. Managers identified four contextual dimensions: care quality, organizational participation, collaborative work, and perceptions of health policy. A final synthesis integrated finding into a systemic motivational model. Conclusion: This study offers a conceptual foundation to develop tools and interventions aimed at improving motivation among primary health care medical personnel. By integrating theory and managerial insight, it highlights the need for systemic approaches that consider individual, organizational, and policy-level factors.
Keywords: Physicians; Primary care; Primary health care; Motivation; Personnel management; Occupational health program
How This Fits In
Previous research on work motivation has focused primarily on general occupational contexts, with limited theoretical frameworks specific to primary care. Motivation in Primary Care Physicians (PCPs) is often reduced to burnout and retention issues, lacking a comprehensive conceptual understanding. This study offers an integrative model combining theoretical insights and healthcare managers’ perspectives to identify motivational indicators and contextual dimensions. It provides a foundation for developing practical tools that can support clinicians’ engagement, well-being, and performance in primary care settings.
Introduction
In recent years, the retention of Primary Care Physicians (PCPs) has become increasingly difficult, with growing challenges in filling necessary positions to ensure adequate physician-to-patient ratios [1,2]. Evidence points toward growing burnout, demotivation, and demoralisation among professionals [3,4], with consequences at the individual level (e.g., burnout and job dissatisfaction), organisational level (e.g., absenteeism and attrition), and societal level (e.g., patient safety concerns [5] and increased healthcare costs [6]. Consequently, some governments and institutions are promoting research in this field to analyse the cause and seek solutions to a situation that could impact the quality of medical care provided [3].
Although work motivation has been widely studied in occupational psychology, it remains a relatively underexplored concept in primary healthcare. Traditionally, the medical profession has been viewed as intrinsically vocational, but recent reports suggest that vocational drive alone is insufficient to sustain PCP well-being and performance. Motivation must therefore be examined not only as a personal attribute but as a construct shaped by systemic, organisational, and policy-related factors. Nevertheless, statistics indicate that vocational drive alone is insufficient to prevent absenteeism and burnout among PCPs [7,8]. The 2024 report by the Spanish Society of Public Health (Sociedad Española de Salud Pública - SESPAS) highlights the need to design specific strategies to stimulate both vocation and motivation among this group to prevent workforce shortages [2].
Recent years have seen a progressive increase in research on occupational health and the quality of life of PCPs [9] with various strategies designed to address professional motivation from a systemic perspective. However, there is still some confusion regarding the definition and dimensions of the construct, which hinders its operationalisation and the design of measurement instruments and evaluation indicators to deepen understanding of motivational issues.
In this study, we adopted the definition of motivation proposed by Franco et al. [10]. According to their perspective, motivation in the work context is conceptualized as an individual’s willingness to exert and sustain effort toward achieving organizational goals, emphasizing both internal psychological processes and transactional dynamics. This approach highlights that worker motivation emerges from the interaction between individuals and their work environment, as well as the alignment between these interactions and the broader societal context [10].
Although we employed the definition of motivation proposed by Franco et al. [10], we also acknowledge that work motivation is fundamentally complex and composed of multiple dimensions. It encompasses a complex interplay of personal, organizational, and societal factors that extend beyond any single definition. That´s why we wanted to explore alternative definitions of motivation found in the literature and examined the motivational theories that support them. By grounding our research in this comprehensive framework while considering other relevant perspectives, we are able to explore the multifaceted nature of motivation and its determinants within organizational setting.
Moreover, the National Academy of Medicine (NAM) has called for systemic approaches to address professional disengagement, proposing interventions at three interrelated levels: The report emphasized the need to develop interventions that target various levels within the healthcare system: (1) frontline care professionals; (2) organizations responsible for health management; and (3) health policy frameworks [11].
In light of the understanding that motivation among PCPs may be a key factor in reducing turnover rates, improving professional well-being, and enhancing the quality of care, we used Ford’s Motivational System Theory [12] as our theorical framework to define motivational dimensions and indicators. A motivational indicator can be defined as a measurable sign or variable that reflects the presence, strength, or direction of an individual’s motivation within a particular context. These indicators provide evidence of how motivation manifests in observable behaviours, attitudes, or outcomes. In contrast, a motivational dimension refers to a specific aspect or component of motivation, such as personal goals, emotional arousal, or personal agency beliefs, which together constitute the multifaceted structure of motivation.
This study was undertaken, establishing two main objectives: (1) Identify the dimensions and indicators related to the motivation of physicians working in primary care, as reported in the scientific literature, beyond engagement; and (2) to analyse the perceptions of personnel managers in primary healthcare centres regarding PCP motivation, incorporating perspectives from the second level of the system in order to provide an integrated and systemic understanding of the phenomenon.
Materials and Methods
Data sources, search strategy, and study selection
This exploratory study was conducted in two sequential phases:
(1) a scoping review to identify theoretical frameworks and constructs related to Primary Care Physicians’ (PCPs) work motivation; and (2) a qualitative survey administered to healthcare managers in Catalonia to assess their perceptions of motivated behaviour and organisational determinants.
Phase 1
A scoping review was carried out following the recommendations of the Joanna Briggs Institute (JBI) [13] and reported in accordance with the PRISMA 2020 guidelines [14]. The objective was to identify the theoretical frameworks and dimensions currently being used in research to evaluate motivation of PCPs. The search was structured using the PCC framework (Population, Concept, and Context): the population was defined as PCPs, the concept focused on identifying the dimensions and indicators of work motivation, and the context was framed by the question—What are the indicators of motivated behaviour in the work of PCPs from a systemic approach?
The search was conducted between June and September 2023, using major databases such as MEDLINE/PubMed, Scopus, and Web of Science (WoS). Keywords such as “motivation*” AND “physician*” AND “workplace” were initially used, followed by a free-text search. The term “engagement” was excluded since a recent review on this topic already exists [15]. The search was limited to articles published after 2000, available in Spanish, English, or French. Only empirical studies that evaluated PCP motivation and included theoretical foundations were selected; unpublished works and grey literature were excluded. Titles and abstracts were screened to select articles fitting the review concept.
Following the initial search, each author independently screened the titles before combining their findings. A total of 512 articles were identified that matched the criteria regarding target population, publication date, study design, and language. These articles were manually checked to remove duplicates, resulting in 380 abstracts. Upon further review of the abstracts, 328 were excluded for not fulfilling the inclusion criteria. The full texts of the remaining 52 articles were then obtained and thoroughly reviewed, with 21 subsequently excluded for not meeting the inclusion criteria. A table was created to summarise the findings of the reviewed articles. The screening process included title and abstract review, followed by full-text assessment, and is illustrated in a PRISMA flow diagram (Figure 1).
The information obtained from the articles was recorded in two tables, available as Supplementary Table 1 and Supplementary Table 2. A thematic analysis of these tables was then conducted using ATLAS.ti 23 software, based on the data collected from the reviewed articles. The analytical approach combined inductive thematic identification of motivational theories (Table 1) with a deductive categorisation of motivational determinants, dimensions, and indicators based on three guiding categories: (1) personal and psychological determinants, (2) systemic and organisational determinants, and (3) motivational outcomes. Each identified indicator was then classified as one of three types: (a) goal-directed activity, (b) affective impact of work and working conditions, or (c) personal/prosocial meaning. These indicator types were determined deductively by mapping themes across studies and assessing conceptual convergence and are displayed in Table 2.
|
Motivational
Theory |
Definition
of Motivation |
Key
Bibliographic Fragments |
|
Self-Determination
Theory (SDT) |
Motivation
is seen as a continuum between autonomous motivation (self-directed actions
aligned with personal values) and controlled motivation (driven by external
or internal pressures). |
“Intrinsic
motivation: driven by genuine interest and enjoyment of an activity…
Prosocial motivation: desire to work for the benefit of others” [16];
“Autonomous motivation... vs. controlled motivation…” [17].
“Motivation is described as an external state that fosters a
specific behaviour, evidenced by internal responses.” [18] “Individuals are
intrinsically motivated and integrate intrinsic and extrinsic motivational
factors in their lifelong pursuit of well-being.”
[19] |
|
Behavioral
Economics (Motivation Crowding Theory) |
Introduces
the effects of crowding-in (reinforcement of intrinsic motivation through
incentives) and crowding-out (reduction due to external control). |
“Intrinsic
motivation relies on willingness and self-determination… can be undermined if
an intervention is perceived as a lack of trust…” [20] |
|
Herzberg's
Motivation-Hygiene Theory |
Motivation
arises from motivating factors (achievements, recognition), not from hygiene
factors (salary, work conditions). |
“The
degree to which an individual is willing to exert effort and maintain that
effort to achieve organisational goals.” [21] |
|
Maslow's
Hierarchy of Needs |
Motivation
comes from the progressive satisfaction of needs, from physiological to
self-actualization. |
“Motivation
is defined as the process that awakens, energises, directs, and sustains
behaviour…” [22] |
|
Alderfer's
ERG Theory |
A
variation of Maslow’s theory in three levels: existence, relatedness, and
growth. |
“Motivation
is a process that activates and sustains goal-directed behaviour…” [23] |
|
Franco et al.'s Conceptual Model |
Emphasizes
the dynamic interaction between the individual and the work/social
environment. |
“It
is a dynamic psychological process resulting from the interaction between
individuals and their work environment.” [24] |
|
Public
Service Motivation (PSM) |
A
predisposition to respond to motives related to public and social service. |
“PSM:
Individual’s predisposition to respond to motives tied primarily or
exclusively to public institutions…” [25] |
|
Vroom's
Expectancy Theory |
People
evaluate expected rewards to decide whether the effort is worthwhile. |
“Work
motivation is the perception of a link between effort and rewards.” [26] |
|
Adams'
Equity Theory |
Motivation
is influenced by perceptions of fairness in the distribution of rewards. |
Included
in multiple theory reviews [27] |
|
McGregor’s
Theories X and Y |
Theory
X: the worker is passive and needs control. Theory Y: the worker is proactive
and seeks self-fulfilment. |
“A
motivated employee demonstrates interest, punctuality, dedication, and effort
to perform…” [26] |
|
WHO
- Health Workers for Change Model |
Emphasizes
health worker satisfaction as a key factor in motivation. |
“The
willingness to exert and maintain effort towards organisational goals.” [28] |
Table 1: Definition of the construct “Motivation” and theories used in research on PCPs.
|
Determinant |
Indicators |
Motivational Dimension |
Indicator Type |
Supporting Quote |
|
Basic psychological needs (SDT) |
Autonomy, competence, relatedness; work satisfaction |
Intrinsic / Autonomous |
Affective impact, Personal reasons |
“I feel that I have a great deal of choice in how I approach patient care” [17] |
|
Intrinsic aspirations / Vocation / Altruism |
Enjoyment, calling, empathy, desire to help others |
Intrinsic / Prosocial |
Personal reasons, Affective impact |
“Service, help/empathy, dedication” [30] |
|
Administrative burden / Bureaucracy |
Overload, loss of task meaning, pressure, limited feedback |
Mixed: Intrinsic / Extrinsic |
Affective impact |
“Low-functionality paperwork (red tape)” [31] |
|
Managerial / Supervisory support |
Recognition, trust, perception of support |
Relational / Organizational |
Affective impact, Personal reasons |
“Employees’ global beliefs about the extent to which supervisors value their contributions” [25] |
|
Incentives (economic and non-economic) |
Salary, training, promotion, recognition |
Extrinsic |
Goal-directed activity, Affective impact |
“Extra shift – task meaning changes – transactional mindset” [30] |
|
Public service motivation |
Commitment, compassion, civic duty, user orientation |
Prosocial |
Personal reasons |
“Desire to help others” [16] |
|
Interpersonal relations / Work climate |
Teamwork, patient appreciation, sense of belonging |
Relational |
Affective impact, Personal reasons |
“Good relationships with colleagues, patient appreciation” [23] |
|
Professional autonomy / Participation |
Teaching, mentoring, networks, prevention programs |
Intrinsic |
Goal-directed activity |
“Participation in non-financially incentivised activities” [32,33] |
|
Job satisfaction and wellbeing |
Pride, purpose, self-efficacy, burnout, job security |
Intrinsic |
Affective impact, Personal reasons |
“Pride in working for the organization” [24] |
|
Working conditions / Context |
Infrastructure, resources, job stability, role clarity |
Extrinsic |
Affective impact |
“No need to pay bribes to get things done” [34] |
|
Organizational commitment |
Retention intention, sense of belonging, institutional pride |
Organizational |
Personal reasons |
“I feel personal satisfaction when I do my job well” [26] |
|
Training and professional development |
Opportunities for improvement, evaluations |
Intrinsic / Extrinsic |
Goal-directed activity |
“Opportunity for further training” [35] |
|
Sociodemographic / Cultural factors |
Age, gender, location, values, cultural identity |
Contextual |
Personal reasons |
“Cultural norms and values, individual personality” [36] |
|
Emotional and familyrelated factors |
Personal life challenges, emotional strain, distance from family |
Personal / Contextual |
Affective impact, Personal reasons |
“Spouse living far away, difficult living conditions” [37] |
Table 2: Determinants, indicators, and motivational dimensions of motivated behaviour.
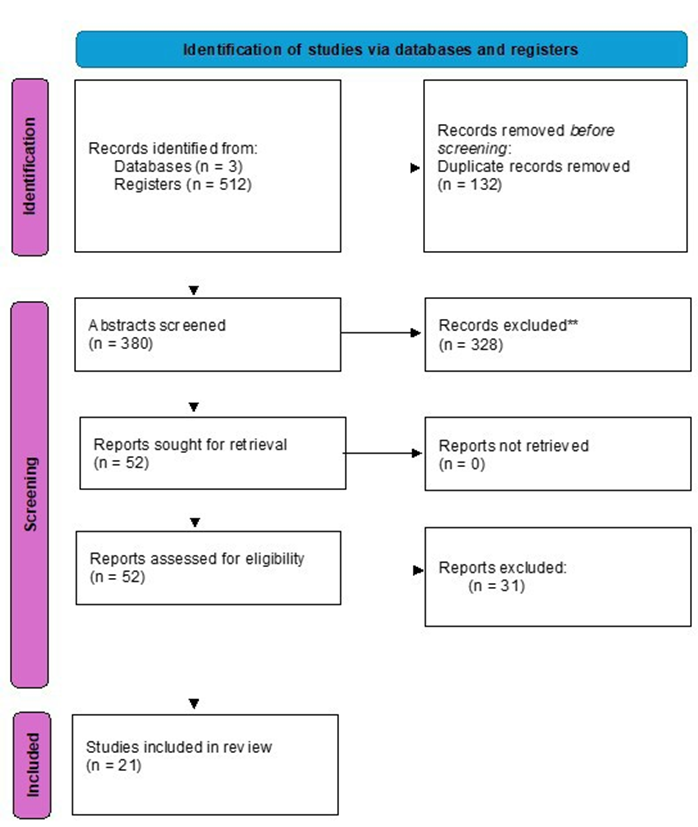
Figure 1: PRISMA 2020 Flow diagram [14].
The diagram illustrates the process of identification, screening, eligibility assessment, and inclusion of studies in the scoping review, following PRISMA 2020 guidelines for the Flow diagram. The number of records identified, screened, excluded, and included at each stage is indicated in the corresponding boxes.
Phase 2
This study was conducted in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The research project was presented to the SSIBE Research Commission and was approved on 2 November 2023 Commission (approval code: 55923/23). The committee forwarded it for presentation and approval by the CEIm-Girona (Comité de Ética de la Investigación con Medicamentos) which subsequently approved the project for implementation (CEIm code: 2023.228).
A purposive sampling strategy was used to recruit participants from publicly funded, privately managed healthcare organisations in Catalonia. The target population included professionals working as directors of primary healthcare centers, members of medical unions, and human resources staff (the Consorci de Salut i Social de Catalunya and the Associació d‘Entitats Sanitàries i Socials) were selected based on their involvement in staff supervision, organisational decision-making, or policy influence to assess the perspective of the second level of the system: organizations responsible for health management [11]. The sample was chosen from employees who are part of the publicly funded but privately managed health care of the Catalan healthcare system that administers Primary Healthcare Centres (Primary Healthcare Centres are the basic management unit of the healthcare system in Spain).
Participants were not previously aware of the study. They were informed about the project’s objectives through an information sheet (Appendix 1). The survey was sent to 24 individuals for completion of whom 9 completed the survey (response rate: 37.5%).
A structured online survey was administered using the RedCap programme. Participants received a detailed information sheet and were informed that completion of the survey implied informed consent. A link generated via RedCap was distributed through institutional email. A first invitation email was sent, followed by a reminder after 15 days. Respondents were given a total of 1.5 months to complete the survey. The survey included six openended questions focused on: (1) perceived indicators of motivation; (2) motivational dimensions; (3) organisational or contextual determinants; and (4) mechanisms for evaluating psychosocial risk. There were no word limits, responses were anonymous, and it wasn’t mandatory to answer all items. Open-ended questions were selected to provide respondents with the freedom to describe their experiences in their own words. All responses were anonymised and analysed in accordance with ethical research principles. Although no formal pre-test was conducted, the survey was reviewed by both researchers involved in the study to ensure face validity.
Raw responses were exported to Excel and imported into ATLAS. ti 23. Two researchers independently reviewed the responses using thematic analysis. Initial codes were developed inductively, grouped into categories through consensus, and triangulated with the results of the scoping review.
Organisational Context
Catalonia’s primary care system is structured around multidisciplinary teams in Primary Healthcare Centres (CAPs), serving populations of 10,000–25,000 residents. Staff typically include general practitioners, nurses, social workers, and administrative personnel. Employment is salaried under either direct public contracts or delegated management agreements with regional providers. Governance involves coordination between health departments and institutional managers. A full description is provided in the Supplementary Material.
Data extraction and risk of bias
Phase 1
The search was conducted independently by each author, AF and EV, using MeSH terms and manual searches. Discrepancies were discussed and resolved through consensus.
Phase 2
Using the RedCap programme, AF extracted the literal responses from the surveys into an Excel table. Subsequently, AF and EV independently reviewed and analysed the data, resolving any discrepancies through discussion and agreement. Atlas.ti 23 software was employed to interpret the collected information.
Patient and public involvement
Phase 1
This phase involved no patients or public.
Phase 2
Phase 2 had no patient involvement. An anonymous survey was administered to primary care medical personnel managers. Respondents received an information sheet detailing the study’s objectives. The survey’s first item asked if they had read and understood the information before proceeding. Participants were informed that completion of the survey implied informed consent. Selecting this item was considered as the consent to participate.
The information sheet (Appendix 1) and survey (Appendix 2) are available for review.
Results
Understanding motivation and theories underpinning research on the motivation of PCPs based on the reviewed literature. With the aim of evaluating the different concepts used to define motivation at work in PCPs and the underlying motivational theories, the studies were categorized according to the motivational theory. The findings can be seen in Table 1.
The most commonly used theoretical frameworks to define work motivation among medical personnel were Self-Determination Theory (SDT), Herzberg’s Motivation-Hygiene Theory, the Motivation Crowding Theory based on behavioural economics (Frey, 1997), [29] and the conceptual model by Franco et al. (Health Worker Motivation) [10]. Approximately 30% of the studies employed a mixed-method approach, using more than one theory, while 17% of the articles lacked a well-argued justification for their choice of theoretical framework.
Determinants, indicators, and outcomes of motivated behaviour in PCPs according to the reviewed literature
To systematise the analysis, the information has been structured into three categories, consistent with the conceptual model proposed by the NAM to explain the well-being of medical personnel [11]: (1) systemic factors acting as determinants/motivators (working conditions, healthcare policies, and regulations); (2) individual factors (dimensions and indicators of motivation); and (3) outcomes and consequences at individual, organisational, and societal levels. While the distinction between these three categories serves an explanatory purpose, it is important to note that personal factors and outcomes are also systemic in nature. The results of the evaluated information are summarised in Table 2.
The thematic analysis of the Supplementary Table 2 suggests three types of indicators: (1) goal-directed activity (effort or dedication invested in achieving personal/organisational objectives); (2) the affective impact of work and working conditions (enjoyment, satisfaction, well-being); and (3) the personal reasons or values underlying the performance of work (public service, user orientation, incentives), which the literature refers to as intrinsic versus extrinsic motivation.
Recognition, which includes both social recognition and acknowledgment by supervisors, stands out as being mentioned in 66% of the studies reviewed. Contributions to the community was referenced as an indicator in 58% of studies, whereas 33% cited prosocial behaviour and altruism. Competence was identified as an indicator in 41% of the studies, and autonomy was mentioned in 33%. Opportunity for teaching, training, and research were identified as a motivational indicator in 25% of the studies.
The indicators of motivated behaviour according to primary care managers
Literal survey results were recorded in an Excel table for analysis. Although the survey was distributed to 24 people, only 9 responses were received, survey participation was 37.5%. Information from nine surveys was analysed in total, with no responses excluded. The data collected were analysed using the Atlas.ti 23 program to identify the most relevant themes; the results are presented in Table 3.
Category | Function |
Quality of care | Refers to actions aimed at promoting patient well-being, participating in training activities to update scientific knowledge, and recording and evaluating population health control indicators
|
Organisational participation | Refers to voluntary participation in professional activities not directly related to patient care
|
Collaborative work | Refers to individual actions that impact the collective
|
Healthcare policies | Reflects professionals’ perceptions of the healthcare system
|
Table 3: Indicators of motivated behaviour in PCPs according to health managers.
Low motivation, a recent decline in motivation, or demotivation within the PCP group were observed by 88% of respondents. Workload pressure was identified as a factor contributing to demotivation by 77% of respondents. Absenteeism was described as an indicator of demotivation by 33% of respondents. Health managers were enquired regarding the evaluation of psychosocial risks, and 55% responded that such assessments are either not carried out or have not been conducted for a long time.
Synthesis of Determinants and Indicators Based on Information from both Sources (Literature and Surveys)
A triangulation process was then performed, comparing themes from this phase with those identified in the scoping review. This integrative step enabled the derivation of four overarching motivational dimensions: Care Quality Orientation, Organisational Belonging, Collaborative Practice, and Health Policy Engagement, which structured the synthesis presented in Table 4.
Motivational Dimension | Grouped Determinants | Associated Indicators | Type of Indicator |
Care Quality Orientation | Professional ethics, patientcentredness, clinical autonomy | Commitment to care, intrinsic drive | Personal/prosocial meaning |
Organisational Belonging | Recognition, team climate, leadership | Job satisfaction, perceived value | Affective impact |
Collaborative Practice | Shared decision-making, peer interaction | Communication, collaboration frequency | Goal-directed activity |
Health Policy Engagement | Policy clarity, institutional alignment, governance | Policy awareness, participation in reforms | Personal/prosocial meaning |
Table 4: Determinants and Indicators of motivation.
To support theoretical coherence, the motivational dimensions and indicators synthesised in Table 4 were defined in accordance with Ford’s (1992) [12] conceptualisation. This framing ensured that the dimensions emerged not only from empirical triangulation between phases but also from established theoretical foundations.
Discussion
This study addresses the complex and multi-level nature of work motivation among Primary Care Physicians (PCPs), advancing current knowledge by integrating findings from a scoping review and qualitative insights from healthcare managers. The research confirms that motivation is not merely a function of individual attitudes or vocational ideals, but rather a product of the interaction between personal, organisational, and systemic factors. This perspective aligns with models that conceptualise motivation across three interdependent levels: healthcare workers, organisations, and policy environments [11].
Our findings indicate that motivation assessment tools should prioritize motivational indicators—such as prosocial motivation, empowerment, and collaborative work—rather than focusing solely on psychosocial work-related factors, which are typically addressed through occupational risk prevention frameworks. Fostering a supportive organizational culture, where PCPs are empowered to contribute safely to institutional improvements, is critical for sustaining motivation and reducing turnover, absenteeism, and burnout.
The results from Phase 1 revealed that existing literature often lacks a unified theoretical framework. While Self-Determination Theory is frequently referenced, many studies rely on mixed models or conceptual ambiguity. Our synthesis, however, was informed by established theories—including Franco et al.’s model—which emphasise the interplay of intrinsic and extrinsic motivators [10]. This phase also clarified that personal factors and motivational outcomes often overlap and are better represented within integrated motivational dimensions and their respective indicators, rather than as isolated analytical categories.
From the surveys conducted with Healthcare Managers we could identify four main determinants of motivated behavior: Care quality: Active involvement in improving patient care and health outcomes. These indicators align with Grant’s concept of prosocial motivation [38], which centres on the desire to promote and protect the well-being of others. Organizational participation: Engagement in non-clinical activities like projects, training, and institutional improvement. Collaborative work: Positive interactions with colleagues and management in a safe environment. This indicator corresponds to the concept of motivation for well-being proposed by Fleury [39], which advocates designing strategies to enhance empowerment with the aim of fostering individuals’ intrinsic motivation to engage in projects and activities that improve their well-being. Perceptions of health policies: How PCPs view and are affected by healthcare regulations and systemic factors. Such an environment should enable professionals to contribute to institutional improvement without fear of reprisal [40]. Similarly, parallels were found between the literature and survey results regarding the importance of meeting the basic needs of medical staff, in line with classical need-based theories of motivation [41].
As a result, from the synthesis of the scoping review and healthcare managers’ perceptions, motivation in PCPs can be understood through three primary indicators: 1. Goal-directed activity: Effort and dedication toward achieving personal, organizational and patient care objectives. 2. Affective impact: Emotional responses to work, including job satisfaction, enjoyment, and well-being. 3. Personal values: Intrinsic/extrinsic reasons for working, such as public service, altruism, professional identity, or external incentives.
This integrative model underscores the need for a systemic approach to assessing and enhancing PCP motivation. Interventions must move beyond individual-level factors and address the organisational culture and policy context in which PCPs operate. Motivational assessment tools should therefore include multidimensional indicators, rather than focusing solely on psychosocial risks as is common in occupational health assessments. Practically, healthcare managers can use these insights to design targeted strategies that enhance intrinsic motivation, foster empowerment, and build trust within teams. Doing so may help mitigate burnout, improve job satisfaction, and strengthen retention in primary care settings.
Despite growing interest in the topic, significant gaps remain in our understanding of PCP motivation. Further research is needed to refine the construct of motivation, develop validated assessment tools, and evaluate the effectiveness of interventions designed to enhance motivation at the systemic level. Future studies should also explore the impact of different healthcare system structures and policy environments on PCP motivation to inform contextspecific management strategies.
Limitations
In reflecting on the limitations of this study, several key considerations must be acknowledged to provide appropriate context for the interpretation of our findings and to guide future research directions.
The relatively low response rate among healthcare managers in the survey phase may limit the representativeness of the qualitative findings and constrain the generalisability of the results to broader primary care settings. Due to the small sample size, data saturation was not fully achieved. However, the findings offer a valuable initial insight that can be complemented by future studies with broader coverage.
These limitations underscore the need for cautious interpretation of the study’s findings and highlight the importance of further research employing larger, more representative samples and longitudinal designs to validate and extend these results.
Conclusion
This study identified three principal indicators of motivation in primary care physicians—goal orientation, affective impact, and personal values—and delineated four key dimensions underpinning motivated behaviour: care quality, organisational participation, collaborative work, and perceptions of health policies. These findings provide a theoretical foundation for the development of targeted assessment tools and management strategies to address motivation in primary care settings.
Our results underscore the need to clarify and operationalise the construct of motivation in primary care, moving beyond traditional assumptions of vocational drive to incorporate systemic and organisational factors. By integrating both literature review and healthcare managers’ perspectives, this study offers a comprehensive framework that can inform interventions aimed at reducing turnover, absenteeism, and professional attrition.
Future research should focus on validating the proposed dimensions and indicators across diverse healthcare contexts and on developing robust, context-sensitive tools for the assessment of motivation among primary care physicians. Ultimately, a clearer understanding and measurement of motivation will support more effective personnel management and contribute to the sustainability and quality of primary healthcare delivery.
Other Information
Contributorship Statement
AF and EV conceptualised and designed the study. Stage 1: AF and EV reviewed titles, abstracts and full-text papers for eligibility. Disagreements were resolved through discussion. Stage 2: AF was responsible for data extraction, and all data extraction was verified by EV. AF and EV prepared, reviewed, and edited the manuscript. AF is the guarantor.
Competing Interest: The authors declare no competing interests.
Funding/Support
The authors received no financial support for the research, authorship and/or publication of this article. The SSIBE research institute provided access to the RedCap database.
Data Sharing Statement
The data collected in the study are available in the RedCap database. All data relevant to the study are included in the article or uploaded as online supplemental information. All data underlying the results are available as part of the article and no additional source data are required.
Ethic Statements
This study was conducted in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The research protocol was reviewed and approved by the SSIBE Research Commission (approval code: 55923/23) and subsequently by the CEIm-Girona (Comité de Ética de la Investigación con Medicamentos; CEIm code: 2023.228). As the survey was conducted anonymously, written informed consent was not required; however, all participants received an information sheet and confirmed their understanding in order to be able to start the survey.
References
- Anderson M, Pitchforth E, Edwards N, Alderwick H, McGuire A, et al. (2022) United Kingdom: health system review. Health Syst Transit 24: 1-194.
- López-Valcárcel B, Barber P (2024) What do we know and what should we know about the imbalances of doctors in Spain? Diagnosis and proposals. SESPAS Report 2024. Gac Sanit 38: 102366. [Article in Spanish].
- Beech J, Fraser C, Gardner G, Buzelli L, Williamson S, et al. (2023) Stressed and overworked. The Health Foundation.
- Pujol-de Castro A, Valerio-Rao G, Vaquero-Cepeda P, Catalá-López F (2024) Prevalence of burnout syndrome in physicians working in Spain: systematic review and meta-analysis. Gac Sanit 38: 102384. [Article in Spanish].
- de Lima Garcia C, de Abreu LC, Souza Ramos JL, Dibai de Castro CF, Neves Smiderle FR, et al. (2019) Influence of burnout on patient safety: systematic review and meta-analysis. Medicina (Kaunas) 55: 553.
- Han S, Shanafelt TD, Sinsky CA, Awad KM, Dyrbye LN, et al. (2019) Estimating the attributable cost of physician burnout in the United States. Ann Intern Med 170: 784-790.
- Baron RA (1991) Motivation in work settings: reflections on the core of organizational research. Motiv Emot 15: 1-8.
- Nguyen MT, Honcharov V, Ballard D, Satterwhite S, McDermott AM, et al. (2024) Primary care physicians’ experiences with and adaptations to time constraints. JAMA Netw Open 7: e248827.
- Florez A, Villar-Hoz E (2024) Role of motivation and well-being indicators in interventions to improve well-being at work among primary care physicians: a systematic review. BMJ Open 14: e075799.
- Franco L, Bennett S, Kanfer R (2002) Public sector health worker motivation and health sector reform: a conceptual framework. Soc Sci Med 54: 1255-1266.
- National Academies of Sciences, Engineering, and Medicine (2019) Taking action against clinician burnout: a systems approach to professional well-being. Washington (DC): The National Academies Press.
- Ford ME (1992) Motivating humans: goals, emotions, and personal agency beliefs. Thousand Oaks, CA: Sage.
- Peters MDJ, Godfrey C, McInerney P, Munn Z (2020) Chapter 11: Scoping reviews (2020 version). In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, et al. (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLOS Med 372: n71.
- Prenestini A, Palumbo R, Grilli R, Lega F (2023) Exploring physician engagement in health care organizations: a scoping review. BMC Health Serv Res 23: 1029.
- Yordanov D, Oxholm AS, Gyrd-Hansen D, Pedersen LB (2022) Mapping general practitioners’ motivation: it is not all about the money. DaCHE Discussion Papers.
- Moller AC, Olafsen AH, Jager AJ, Kao AC, Williams GC (2022) Motivational mechanisms underlying physicians’ occupational health: a self-determination theory perspective. Med Care Res Rev 79: 255266.
- Xu X, Zhou L, Ampon-Wireko S, Quansah PE (2023) Assessing the mediating role of motivation in the relationship between perceived management support and perceived job satisfaction among family doctors in Jiangsu province, China. Hum Resour Health 21: 71.
- Tak HJ, Curlin FA, Yoon JD (2017) Association of intrinsic motivating factors and markers of physician well-being: a national physician survey. J Gen Intern Med 32: 739-746.
- Pedersen LB, Andersen MKK, Jensen UT, Waldorff FB, Jacobsen CB (2018) Can external interventions crowd in intrinsic motivation? A cluster randomised field experiment on mandatory accreditation of general practice in Denmark. Soc Sci Med 211: 224-233.
- Ojakaa D, Olango S, Jarvis J (2014) Factors affecting motivation and retention of primary health care workers in three disparate regions in Kenya. Hum Resour Health 12: 33.
- Malik A, Yamamoto S, Haque S, Aminul M, Butt N, et al. (2018) Developing and assessing a tool to measure motivation among physicians in Lahore, Pakistan. PLoS One 13: e0204956.
- Barikani A, Javadi M, Mohammad A, Firooze B, Shahnazi M (2012) Satisfaction and motivation of general physicians toward their career. Glob J Health Sci 5: 166-173.
- Hotchkiss DR, Banteyerga H, Tharaney M (2015) Job satisfaction and motivation among public sector health workers: evidence from Ethiopia. Hum Resour Health 13: 83.
- Del Estal-García MC, Melián-González S (2021) Public Service Motivation of the professionals of the primary care centers: What is more important the environment or the perceived supervisor support? Aten Primaria 53: 101995. [Article in Spanish].
- Kumar P, Mehra A, Inder D, Sharma N (2016) Organizational commitment and intrinsic motivation of regular and contractual primary health care providers. J Fam Med Prim Care 5: 94-100.
- Montoya R, García A (2001) Motivación del equipo básico de atención integral en salud como factor que contribuye al logro de los objetivos del nuevo modelo de atención integral. Rev Cienc Adm Financ Segur Soc 9: 71-90.
- Agyepong IA, Anafi P, Asiamah E, Ansah EK, Ashon DA, et al. (2004) Health worker (internal customer) satisfaction and motivation in the public sector in Ghana. Int J Health Plann Manage 19: 319-336.
- Frey B (1997) Not Just for the Money. An Economic Theory of Personal Motivation. Cheltenham: Edward Elgar Publishing.
- Berdud M, Casasés JM, Nieto J (2016) Incentives and intrinsic motivation in healthcare. Gac Sanit 30: 408-414.
- Ballart X, Ferrairó F, Iruela A (2023) Administrative burden, motivation and well-being among primary care physicians: comparison of management models. Gac Sanit 37: 102306. [Article in Spanish].
- Sicsic J, Le Vaillant M, Franc C (2012) Intrinsic and extrinsic motivations in primary care: an explanatory study among French general practitioners. Health Policy 108: 140-148.
- Sicsic J, Le Vaillant M, Franc C (2014) Building a composite score of general practitioners’ intrinsic motivation: a comparison of methods. Int J Qual Health Care 26: 167-173.
- Peters DH, Chakraborty S, Mahapatra P, Steinhardt L (2010) Job satisfaction and motivation of health workers in public and private sectors: cross-sectional analysis from two Indian states. Hum Resour Health 8: 27.
- Dieleman M, Cuong PV, Anh LV, Martineau T (2003) Identifying factors for job motivation of rural health workers in North Viet Nam. Hum Resour Health 1: 10.
- Mathauer I, Imhoff I (2006) Health worker motivation in Africa: the role of non-financial incentives and human resource management tools. Hum Resour Health 4: 24.
- Dieleman M, Toonen J, Touré H, Martineau T (2006) The match between motivation and performance management of health sector workers in Mali. Hum Resour Health 4: 2.
- Grant AM, Berg JM (2010) Prosocial motivation at work: how making a difference makes a difference. In: Cameron K, Spreitzer G, editors. Handbook of Positive Organizational Scholarship. Oxford: Oxford University Press; p. 28-44.
Appendix 1:
● Participant Information Sheet
Study Title:
- Fleury J (1996) Wellness motivation theory: an exploration of theoretical relevance. Nurs Res 45: 277-283.
- Floyd D, Prentice-Dunn S, Rogers R (2000) A meta-analysis of research on protection motivation theory. J Appl Soc Psychol 30: 407429.
- Acquah A, Nsiah T, Antie E, Otoo B (2021) Literature review on theories motivation. EPRA Int J Econ Bus Rev 25-29.
DESIGNING A SCALE TO ASSESS WORK MOTIVATION IN PRIMARY CARE PHYSICIANS
We are reaching out to invite you to participate, entirely voluntarily, in a study conducted with individuals who, like you, are involved in the management of medical services. Our goal is to ensure that you have the correct and sufficient information to evaluate and decide whether you wish to participate.
Please read this information sheet carefully, and we will address any questions you may have. It is important to understand that this study will not involve any treatment or diagnostic tests. However, Spanish legislation and ethical principles of confidentiality require that you be informed of the study details and provide your consent to participate.
We would also like to inform you that this study arises from the investigator’s initiative and is conducted without financial compensation. Below, we have outlined the purpose of the study and its key aspects.
Why is this study necessary?
In recent years, retaining primary care physicians in their positions and filling all required posts to maintain an appropriate physician-patient ratio has become increasingly challenging. We believe that developing a scale directly focused on the group in question could provide more tailored insights to design interventions addressing the current issues of burnout and turnover among primary care professionals and the potential consequences for patient care quality.
What characteristics should patients have to participate in the study?
Based on the information provided earlier, participants in this initial phase are individuals involved in medical management.
What are the study objectives, and what diagnostic tests or treatments will be conducted?
The study aims at designing an instrument for assessing work motivation in primary care physicians. Participation will not involve any special diagnostic tests or treatments. An anonymous survey will be administered, without any identifiers that could reveal the participant’s identity. The survey consists of open-ended questions to identify the determinants and dimensions of work motivation among primary care physicians.
What are the benefits and risks of participating in this study?
This study poses no specific risks or benefits for you. It simply seeks to collect data on your perceptions of the motivation of primary care physicians. However, your participation will contribute to a better understanding of this issue, enabling future research.
What happens if I decide to withdraw from the study?
If you choose to participate, you should know that your involvement is entirely voluntary, and you can withdraw at any time without any explanation.
How will my data confidentiality be ensured?
No personal data will be collected, and it will not be possible to identify you at any point. All data collected and analysed will remain anonymous and strictly confidential, in compliance with the General Data Protection Regulation (GDPR) and Organic Law 3/2018 of 5 December, concerning Personal Data Protection and the Guarantee of Digital Rights.
Who should I contact for any questions or issues?
For further information or to report any events during the study, please contact Adriana Flórez via the research department phone number: 972 609226. Any modifications to the project that may affect your rights or participation will be communicated.
During or after the study, to exercise your rights of access, rectification, opposition, limitation of processing, portability, or erasure, you can contact the Fundació Hospital de Palamós – Serveis de Salut Integrats Baix Empordà via the website’s information and procedures/data protection rights section available at www.ssibe.cat, via email at areajuridica@ssibe.cat, or by mail to the Área Jurídica C. Hospital, 17–19, planta 2, de Palamós (17230).
Additional information on data protection policies can be found at www.ssibe.cat. To contact the Data Protection Officer, email dpd@ssibe.cat. If you disagree with how the entity handles your data or believe your rights have been violated, you are also entitled to file a complaint.
Appendix 2:
- What is your personal perception of work motivation among primary care physicians?
- What behaviours or attitudes do you think reflect motivated conduct among primary care physicians?
- What psychosocial risk evaluation measures are currently implemented?
- What factors do you believe influence the motivation of primary care physicians?
- What motivational dimensions do you think contribute to the motivation of primary care physicians?
- What indicators would you evaluate to determine whether primary care physicians are motivated?
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.