Minimally Invasive Laparoscopic Management of a Huge Ovarian Cyst: A Clinical Case and Literature Review
by Elis Ismail1,2*, Emil Kovachev1,2, Stefan Kisiov1,2
1Department of Obstetrics and Gynecology, Medical university ”Prof.d-r Paraskev Stoyanov”Varna, Bulgaria
2SBAGAL”Prof. d-r Dimitar Stamatov”Varna, Gynecology clinic, Bulgaria
*Corresponding author: Elis Ismail, Department of Obstetrics and Gynecology, Medical university ”Prof.d-r Paraskev Stoyanov”Varna, Bulgaria
Received Date: 19 January 2026
Accepted Date: 23 January 2026
Published Date: 26 January 2026
Citation: Ismail E, Kovachev E, Kisiov S (2026) Minimally Invasive Laparoscopic Management of a Huge Ovarian Cyst: A Clinical Case and Literature Review. J Surg 11: 11548 https://doi.org/10.29011/2575-9760.011548
Abstract
Introduction: Pelvic masses affect up to 20% of women during their lifetime and encompass a spectrum of gynecologic and nongynecologic conditions. Adnexal masses-located in the fallopian tubes, ovaries, and adjacent adnexal structures-are predominantly benign. Ovarian cysts represent one of the most common gynecologic pathologies across all age groups and may be either benign or malignant. The most frequently encountered benign entities include simple serous (functional) cysts and endometriotic cysts, approximately 60% of cases are benign serous cysts, 25% are malignant, and 15% exhibit borderline malignant potential.
Case presentation: We present a 25-year-old nulliparous patient. For one month she had experienced a sensation of heaviness and discomfort in the lower abdomen (below the umbilicus). On inspection of the abdomen there was visible distension, with the abdominal contour rising above the level of the umbilicus. Ultrasonography showed a right ovarian cyst with hypoechoic contents, without a solid component and without intracystic papillary projections. The sonographic features suggested a benign lesion. The cyst measured 20 × 17 × 13 cm on ultrasound. Based on the ultrasound images and the normal tumor marker level, a minimally invasive approach was considered most appropriate for this patient. Insufflation with carbon dioxide and creation of the pneumoperitoneum were performed via Palmer’s point, the camera trocar was introduced through the Lee Huang point. The cyst contents were aspirated using a puncture needle, which allowed improved visualization of the pelvic anatomy. Following decompression of the cyst and reduction of its volume, visualization of the peritoneal cavity is markedly improved. Approximately 6 liters of clear serous fluid were drained from the cyst cavity. Following decompression, and considering the patient’s nulliparity and desire to preserve fertility, the cyst was carefully dissected with its capsule, maximizing preservation of healthy ovarian tissue.
Discussion: Surgical management is recommended for ovarian cysts exceeding 5 cm in diameter because of the increased risk of complications. Open-entry laparoscopy access to the peritoneal cavity is commonly achieved via a minilaparotomy. This open-entry approach enhances safety by obviating blind needle or sharp trocar insertions (e.g., Veress needle), thereby reducing the risk of major vascular or bowel injury. This technique is particularly advantageous in patients with suspected intra-abdominal adhesions or a history of prior laparotomy, where blind entry is associated with elevated risk. In our case, a screw-type trocar was inserted under direct laparoscopic (camera) visualization.
Conclusion: Laparoscopic management of huge benign ovarian cysts is a safe and effective alternative to laparotomy when appropriate patient selection is applied. Compared with the open approach, laparoscopy does not appear to increase perioperative complication rates and offers clear advantages including shorter hospital stay, faster postoperative recovery, and the potential for ovarian-sparing surgery - a critical benefit for reproductive age patients desiring future fertility.
Keywords: Huge Ovarian Cyst; Large Ovarian Cyst; Laparoscopic Management; Minimal-Invasive Surgery
Introduction
Ovarian cysts represent one of the most common gynecologic pathologies across all age groups and may be either benign or malignant. The most frequently encountered benign entities include simple serous (functional) cysts and endometriotic cysts, approximately 60% of cases are benign serous cysts, 25% are malignant, and 15% exhibit borderline malignant potential [1]. Pelvic masses affect up to 20% of women during their lifetime and encompass a spectrum of gynecologic and non-gynecologic conditions. Adnexal masses-located in the fallopian tubes, ovaries, and adjacent adnexal structures-are predominantly benign. Clinical evaluation should include an assessment for symptoms indicative of malignancy, such as abdominal pain, abdominal distension, and early satiety; a family history of ovarian or breast cancer or known hereditary cancer syndromes confers increased malignant risk. In women of reproductive age, ectopic pregnancy must be excluded by measurement of β-Human Chorionic Gonadotropin (β-hCG). Transvaginal ultrasonography is the imaging modality of choice for characterization of adnexal masses with respect to size and complexity. Cysts exceeding 10 cm in diameter, lesions containing solid components, or those demonstrating increased color flow on Doppler ultrasonography are considered high risk for malignancy. When extra-ovarian disease is suspected, further cross-sectional imaging with Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) is indicated. Multimodal assessment strategies that integrate ultrasonographic features with serum biomarkerssuch as the Risk of Malignancy Index (RMI)-are valuable for differentiating and excluding malignant etiologies. Asymptomatic masses adjudicated as benign may be managed expectantly with surveillance. Symptomatic or emergent presentations (e.g., ectopic pregnancy, ovarian torsion) necessitate prompt consultation with an obstetrician–gynecologist, and any adnexal mass assessed as high risk for malignancy warrants referral to gynecologic oncology [2].
Huge ovarian cysts are conventionally managed by laparotomy. Serous ovarian cysts are typically asymptomatic when small and are often detected incidentally. Progressive enlargement may produce nonspecific symptoms attributable to mass effect on adjacent organs. The most common symptoms associated with large ovarian cysts include lower abdominal heaviness and discomfort, abdominal distension, constipation, urinary frequency/urgency, dyspareunia, and dysmenorrhea. Lesions measuring 4–10 cm (1.5–4 inches) are frequently classified as large and may warrant removal, although the indication depends on the cyst type and presenting symptoms. An ovarian cyst is typically regarded as “large” when its maximal diameter is greater than approximately 5 cm (≈2 inches), and some practitioners further classify lesions measuring between 5 cm and 10 cm as large. By contrast, “giant” or “huge” ovarian cystsalthough uncommon-are generally defined as those exceeding 15 cm (≈6 inches) in diameter; certain histologic subtypes, notably mucinous cystadenomas, can reach substantially larger sizes, at times attaining 30–50 cm (≈1–1.5 feet). Large ovarian cysts measuring >10 cm in maximal diameter generally require surgical excision, most commonly performed via a minimally invasive laparoscopic approach (cystectomy or oophorectomy), following appropriate preoperative imaging and oncologic risk assessment. During surgical management, it is essential-particularly in patients who desire future fertility-to preserve ovarian tissue. The surgical objective is to maximize preservation of ovarian reserve and reproductive potential by performing fertility-sparing procedures (e.g., cystectomy with careful preservation of normal ovarian parenchyma), minimizing excision of healthy ovarian tissue, employing meticulous hemostasis to reduce ischemic injury, and tailoring the extent of resection based on lesion characteristics and oncologic risk.
Case Presentation
We present a 25-year-old nulliparous patient. For one month she had experienced a sensation of heaviness and discomfort in the lower abdomen (below the umbilicus). She was diagnosed with an ovarian cyst and visited us for a second opinion because an open surgical approach had been recommended. On inspection of the abdomen there was visible distension, with the abdominal contour rising above the level of the umbilicus (Figure 1).

Figure 1: Image demonstrating the lower abdominal contour rising above the umbilicus.
Ultrasonography showed a right ovarian cyst with hypoechoic contents, without a solid component and without intracystic papillary projections. The sonographic features suggested a benign lesion. The cyst measured 20 × 17 × 13 cm on ultrasound. The uterus and left ovary were unremarkable. No free fluid was detected in the pouch of Douglas. The tumor marker CA-125 was within the normal range at 16 U/ml. Based on the ultrasound images and the normal tumor marker level, a minimally invasive approach was considered most appropriate for this patient. Undoubtedly, minimally invasive surgery is more conservative for the patient, as it avoids a large incision, results in less blood loss and postoperative pain, and allows a shorter hospital stay. The size of the cyst, particularly when it extends above the level of the umbilicus, is a limitation for the minimally invasive approach. Such large masses make laparoscopy more difficult to perform and more time-consuming. In these situations it is not possible to use the classic approach of introducing the camera through the umbilical ring. In this patient, insufflation with carbon dioxide and creation of the pneumoperitoneum were performed via Palmer’s point, which is located in the upper left abdomen, 3 cm below the costal margin (rib edge) in the midclavicular line (Figure 2). With this approach it is essential that the stomach be completely empty (e.g., by placement of a nasogastric tube). The camera trocar was introduced through the Lee Huang point, located at the midpoint of the midline between the sternum and the umbilicus. After the skin incision, the subcutaneous fat was dissected and a 10 mm screwshaped trocar was introduced under optical control with a rotating motion (Figure 3).
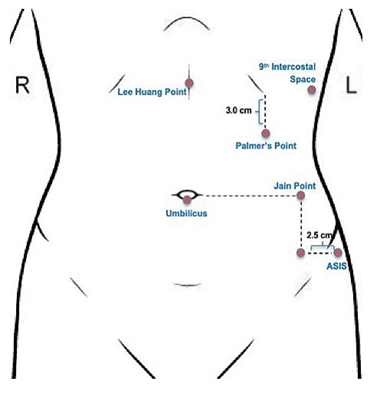
Figure 2: Abdominal wall-Plamer’s and Lee Huang points.
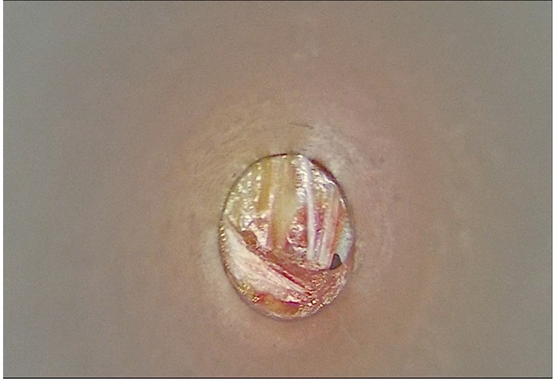
Figure 3: Screw-shaped trocar was introduced under optical control.
After introduction of the camera into the abdominal cavity, the next challenge was obtaining an adequate view (Figure 4). Given the large size of the cyst, it cast a constant shadow, which hindered the surgeon’s orientation with respect to the anatomy of the pelvis and abdominal cavity. A survey of the entire abdomen was performed and three 5 mm working trocars were introduced. After confirming that the cyst originated from the right ovary and that the uterus and left ovary were normal, cyst decompression was undertaken. The cyst contents were aspirated using a puncture needle, which allowed improved visualization of the pelvic anatomy (Figure 5). Following decompression of the cyst and reduction of its volume, visualization of the peritoneal cavity is markedly improved. Approximately 6 liters of clear serous fluid were drained from the cyst cavity. Following decompression, and considering the patient’s nulliparity and desire to preserve fertility, the cyst was carefully dissected with its capsule, maximizing preservation of healthy ovarian tissue (Figure 6 and 7). Via the minimally invasive approach an atraumatic right cystectomy was performed, preserving the right fallopian tube and part of the right ovarian parenchyma.
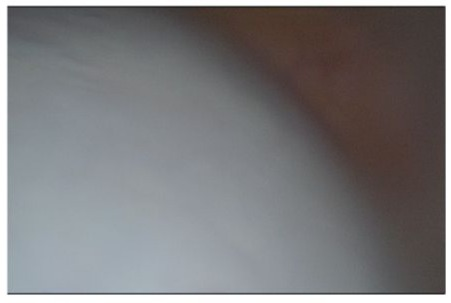
Figure 4: Laparoscopic view after insertion of the laparoscope
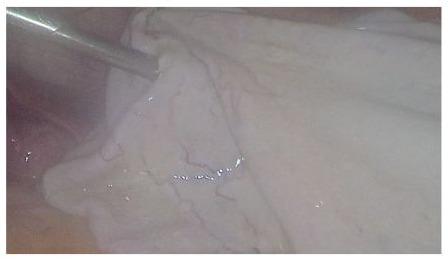
Figure 5: Aspiration of the cyst contents

Figure 6: Dissection of the cyst.

Figure 7: Surgical separation of the cyst capsule with preservation into the peritoneal cavity. of ovarian parenchyma.
There were no postoperative complications, and the patient was discharged the following day.
Discussion
In literature other authors have described five cases of large ovarian cysts that were managed laparoscopically without complications. The patients’ ages ranged from 19 to 69 years, and tumor markers were within normal limits for all individuals. Ultrasound measured the maximal cyst diameters between 18 and 42 cm. All cysts were unilocular, although fine septations were present in some cases. Each patient underwent open-entry laparoscopy, following inspection of the cyst capsule, the cysts were decompressed laparoscopically, with 1–12 L evacuated (mean 5.2 L), after which laparoscopic oophorectomy was performed. Final histopathology identified benign serous cystadenoma in four patients and a benign mucinous cystadenoma in one. Blood loss was minimal and no perioperative complications were reported [3]. Open-entry laparoscopy access to the peritoneal cavity is commonly achieved via a minilaparotomy, in which a small incision is made and the fascia and parietal peritoneum are incised under direct vision prior to trocar placement. This open-entry approach enhances safety by obviating blind needle or sharp trocar insertions (e.g., Veress needle), thereby reducing the risk of major vascular or bowel injury. The use of threaded (screw) ports confers additional stability by securing the trocar to the abdominal wall and preventing port displacement during instrument exchanges. This technique is particularly advantageous in patients with suspected intra-abdominal adhesions or a history of prior laparotomy, where blind entry is associated with elevated risk. The scope of minimally invasive surgical techniques is considerable. Case reports have documented successful laparoscopic excision of an ovarian cyst measuring 38 × 35 × 24 cm in a 13-year-old patient. In the management of large ovarian cysts, surgeons should possess advanced expertise in minimally invasive approaches to optimize operative management of such large lesions and minimize the likelihood of conversion to an open procedure [4].
Surgical management is recommended for ovarian cysts exceeding 5 cm in diameter because of the increased risk of complications. Potential adverse events include adnexal torsion and cyst rupture with resultant hemoperitoneum. Ovarian torsion may necessitate loss of the entire adnexa and thereby substantially reduce the patient’s reproductive potential, an outcome that is particularly undesirable in young women of reproductive age. Rupture of the cyst capsule can precipitate rapid intraperitoneal hemorrhage owing to the rich arterial supply of the ovary (ovarian arteries), which may lead to acute blood loss with hemodynamic collapse and hypotension. In emergent presentations, definitive surgical management is frequently performed via laparotomy because there is insufficient time to pursue a minimally invasive approach, a situation that adversely affects the patient. Accordingly, prompt diagnosis and implementation of an individualized treatment plan are essential to achieve maximal tissue preservation and to minimize surgical trauma, with special attention to fertilitysparing strategies whenever oncologic risk assessment permits. Selection of the operative approach is predicated primarily on ultrasonographic findings, with MRI reserved for problem-solving or further characterization of indeterminate or complex adnexal masses. Preoperative assessment should integrate imaging (transvaginal/transabdominal ultrasound with Doppler ± MRI), serum tumor markers (CA-125 and Human Epididymis Protein 4 [HE4]) and composite algorithms such as the Risk of Ovarian Malignancy Algorithm (ROMA).
Standardized ultrasound reporting using the O-RADS (Ovarian-Adnexal Reporting and Data System) classification facilitates objective stratification of malignancy risk and guides management decisions. A multimodal risk assessment that combines O-RADS category, sonographic features (size, unilocular vs multilocular architecture, solid components, papillary projections, wall irregularity, septations, and vascular flow), and biomarker results should determine whether a minimally invasive or open surgical strategy is appropriate. Lesions categorized as low risk by O-RADS with normal tumor markers and no radiologic signs of extra-ovarian disease are generally suitable for minimally invasive, fertility-sparing procedures (e.g., laparoscopic cystectomy with use of specimen retrieval bag and measures to avoid spillage), provided the operating team has adequate expertise. Conversely, masses with high-risk sonographic characteristics, elevated biomarkers/ROMA score, large size, or radiologic evidence of extra-ovarian spread warrant gynecologic-oncology consultation and are more appropriately managed by an open approach that permits formal oncologic staging and minimizes the risk of intraoperative tumor dissemination. Other practical considerations influencing the choice of approach include the patient’s age and reproductive desires, prior abdominal surgery/adhesions, availability of intraoperative frozen section, and institutional/ surgeon experience with complex minimally invasive oncologic procedures. Ultimately, individualized preoperative counseling and multidisciplinary planning are essential to balance oncologic safety with tissue preservation and minimal surgical morbidity [58].
Conclusion
Small asymptomatic cysts need to be monitored, but larger complex or solid tumors must all be thoroughly examined to rule out malignancy. Early diagnosis and preservation of the ovary should be the aim of treatment. Although guidelines exist for the treatment of adnexal masses in adults, there is limited information available in the literature regarding adolescents. Therefore, it is crucial to establish an appropriate surgical plan that preserves fertility in this vulnerable age group [9]. There is still no consensus for the size limitation of ovarian cysts decided to be a contraindication for laparoscopic management. With advancing techniques, proper patients selection, and availability of experts in gynecologic endoscopy, it is possible to remove giant cyst by laparoscopy [3]. Laparoscopic management of huge benign ovarian cysts is a safe and effective alternative to laparotomy when appropriate patient selection is applied. Compared with the open approach, laparoscopy does not appear to increase perioperative complication rates and offers clear advantages including shorter hospital stay, faster postoperative recovery, and the potential for ovarian-sparing surgery - a critical benefit for reproductive age patients desiring future fertility. Optimal outcomes depend on surgeon expertise, meticulous technique to minimize spillage and haemorrhage, and readiness to convert to laparotomy or involve gynecologic oncology when intraoperative findings raise concern for malignancy.
References
- Fady S.Moiety, Osama El Ashkar, Abdel Fattah Agameya. Laparoscopic ovarian cystecomy for a huge ovarian cystic mass : A case report and review of literature EBWHJ 2018. 10.21608/ebwhj.2018.5642.
- Wheeler V, Umstead B, Chadwick C (2023) Adnexal Masses: Diagnosis and Management. Am Fam Physician 108: 580-587.
- Alobaid A, Memon A, Alobaid S, Aldakhil L (2013) Laparoscopic management of huge ovarian cysts. Obstet Gynecol Int 2013: 380854.
- Zhao H, Zhao S, Zhang S (2025) Laparoscopic treatment of giant ovarian cystic tumors in children: Case report. Medicine (Baltimore) 104: e42920.
- Cannella R, Lanza C, Pellegrino G (2026) RADS ALPHABET: news and tips for young and general radiologists. Insights Imaging 17: 9.
- Andreotti RF, Timmerman D, Strachowski LM (2019) O-RADS US Risk Stratification and Management System: A Consensus Guideline from the ACR Ovarian-Adnexal Reporting and Data System Committee. Radiology 294: 168-185.
- Timmerman D, Ameye L, Fischerova D (2010) Simple ultrasound rules to distinguish between benign and malignant adnexal masses before surgery: prospective validation by IOTA group. BMJ 341: c6839.
- Moore RG, McMeekin DS, Brown AK (2009) A novel multiple marker bioassay utilizing HE4 and CA125 for the prediction of ovarian cancer in patients with a pelvic mass. Gynecol Oncol 112: 40-46.
- Agarwal M, Singh S, Sinha S (2025) Comprehensive Evaluation of Ovarian Growths in Young Women. Gynecol Minim Invasive Ther 14: 145-151.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.