Medical Management of Acromegaly in A Middle-Aged Woman with Pituitary Macroadenoma and Metabolic Comorbidities: A Case Report
by Abdelrahman Shehata1*,Ayesha Aijaz1, Ibrahim Ibrar1, Abia Gouher1,Muhammad Kamil Shahbaz1, Mahir Jallo2
1College of Medicine, Gulf Medical University, Ajman, UAE.
2Department of Internal Medicine, Thumbay University Hospital, Ajman, UAE.
*Corresponding author: Abdelrahman Shehata, College of Medicine, Gulf Medical University, Ajman, UAE.
Received Date: 24 August, 2025
Accepted Date: 01 September, 2025
Published Date: 03 September, 2025
Citation: Shehata A, Aijaz A, Ibrar I, Gouher A, Shahbaz MK, et al. (2025) Medical Management of Acromegaly in A Middle-Aged Woman with Pituitary Macroadenoma and Metabolic Comorbidities: A Case Report. Curr Trends Intern Med 9: 248. https://doi.org/10.29011/2638-003X.100248
Abstract
A 62-year-old Iraqi woman had metabolic comorbidities such as type 2 diabetes, hypertension, and dyslipidemia, in addition to acromegaly symptoms, which included progressive enlargement of the hands, feet, and face. After her doctor saw physical changes and performed relevant tests, she was diagnosed with acromegaly and pituitary macroadenoma. The diagnosis was confirmed by laboratory tests showing markedly high levels of growth hormone (GH) and insulin-like growth factor-1 (IGF-1). A 14 x 12 x 9 mm pituitary macroadenoma was discovered by MRI imaging; there were no optic chiasm compression or visual field abnormalities.
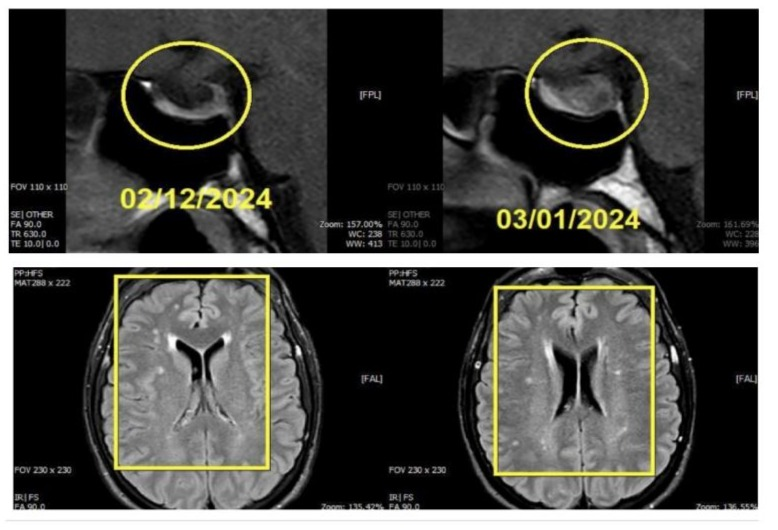
The patient chose medicinal care over surgical intervention. Sandostatin LAR (octreotide), a somatostatin analog, was prescribed to her with a steady increase in dosage. IGF-1 levels gradually decreased in follow-up lab tests, suggesting a successful course of treatment. A regressive phase of the disease was suggested by repeat MRI scans that showed cystic degeneration and a decrease in the size of the pituitary adenoma.
The instance emphasizes how critical it is to diagnose acromegaly as soon as possible and treat it appropriately, especially in people who are not candidates for surgery. By efficiently regulating hormone levels and decreasing tumor size, somatostatin analogs such as octreotide can enhance patient outcomes. Better management of the patient’s acromegaly also improved her metabolic comorbidities, highlighting the connection between metabolic and endocrine health. In order to maximize patient care, this case highlights the necessity of controlling acromegaly through a multidisciplinary strategy that combines endocrinological, radiological, and surgical competence.
Objectives
This case report aims to
- Diagnosis and Presentation: Create awareness to the subtle physical alterations and metabolic comorbidities such as diabetes and hypertension in the clinical presentation of acromegaly in a 62-year-old female with a pituitary macroadenoma.
- Diagnostic Workup: Show how to confirm acromegaly and pituitary macroadenoma using MRI imaging and biochemical assays (elevated IGF-1 and GH).
- Making a treatment decision: Examine available choices, giving particular attention to using somatostatin analogs (Sandostatin LAR) for patients who refuse surgery and the significance of dose escalation in response to response.
- Monitoring and Follow-Up: In order to evaluate the effectiveness of treatment and tumor reduction, it is crucial to regularly monitor IGF-1, GH levels, and imaging.
- Patient Outcomes: Document the patient’s positive response to treatment, such as decreased tumor size and enhanced metabolic regulation.
- Educational Value: As a resource for medical practitioners handling pituitary problems, this brief summary of acromegaly management is provided.
This case report emphasizes the necessity for a customized, interdisciplinary approach and attempts to improve knowledge of managing acromegaly, especially under challenging instances.
Background
Acromegaly is an uncommon endocrine condition brought on by an overabundance of growth hormone (GH), usually as a result of a pituitary adenoma that secretes GH. This results in increased insulin-like growth factor-1 (IGF-1) levels, which cause systemic problems like cardiovascular, metabolic, and musculoskeletal issues as well as progressive somatic alterations like larger hands, feet, and facial characteristics [1]. With an estimated prevalence of 40–70 instances per million, the illness is generally discovered late because of its subtle onset [2]. To reduce the increased morbidity and mortality linked to acromegaly, especially from cancer and cardiovascular disease, early identification and treatment are essential [3].
Transsphenoidal surgery is the main treatment for acromegaly; it is less successful for macroadenomas but curative for 80–90% of microadenomas [4]. Medical therapy is the foundation for individuals who are not candidates for surgery or who have a disease that has persisted after surgery. Octreotide and lanreotide are examples of somatostatin receptor ligands (SRLs), which are first-line medications that efficiently lower GH and IGF-1 levels and frequently reduce tumor size [5]. Other alternatives include dopamine agonists and GH receptor antagonists, such as pegvisomant, especially for people who are resistant to SRLs [6].
A 62-year-old woman with acromegaly and a pituitary macroadenoma is the subject of this case study, which emphasizes the difficulties in treating the illness when metabolic comorbidities are present and the patient declines surgery. It emphasizes how crucial customized therapy regimens are, as well as how SRLs help achieve tumor regression and metabolic control.
Patient demographic information
Age: 62
Gender: Female
Ethnicity: Iraq
Occupation: Administrator job in medical center
Clinical history
Symptoms
- She noticed gradual enlarged hands and feet
- She noticed that she can not be able to put her rings that used to fit
- She noticed that her shoe size has progressively increased from 39 to 41.
- She noticed gradual changes in her face’s shape, enlarged nose & thickened lips
- Excessive sweating and body odor with more oily skin
- A deepened husky voice
- Increased snoring
- Family history: Not contributory
- Lifestyle: Not contributory
Family history and lifestyle factors
Previous treatments
She is taking medications for her type 2 DM, hypertension, dyslipidemia, and thyroid nodule.
Presentation
We present the case of a 62-year-old woman from Iraq who was diagnosed with pituitary macroadenoma and acromegaly on January 6, 2024. Her medical history is significant for longstanding Type 2 Diabetes Mellitus, hypertension, dyslipidemia, and thyroid nodules, which had been challenging to manage despite multiple medications. Given the nature of her condition, surgical intervention was recommended as the optimal treatment option; however, the patient declined the procedure. Consequently, a tailored medical management plan was developed, and she was subsequently referred to Thumbay University Hospital, Ajman, for further specialized care.
Diagnostic assessment
List of diagnostic tests performed and their results, interpretations, and differential diagnoses.
Serum insulin-like growth factor-1 (IGF-1, somatomedin-C) was markedly elevated at 1,121 ng/mL (reference range: 59.5-179.0).
A growth hormone stimulation test demonstrated persistently elevated and paradoxically rising GH levels:
Growth hormone - Baseline: 8778.0 pg/mL
Growth hormone - 30 minutes: 7658.0 pg/mL
Growth hormone - 60 minutes: 12512.0 pg/mL Growth hormone - 90 minutes: 25607.0 pg/mL
Growth hormone - 120 minutes: 28350.0 pg/mL
Pituitary MRI revealed an enlarged pituitary gland due to a welldefined ovoid lesion predominantly involving the left lateral wing of the anterior lobe (adenohypophysis), measuring 14 × 12 × 9 mm. The lesion exhibited a heterogeneous texture, with mixed high and low signals on T2-weighted imaging (T2WI) and heterogeneous isointense to low signal on T1-weighted imaging (T1WI). Post-contrast series demonstrated faint heterogeneous enhancement, which was less than that of the adjacent normal pituitary parenchyma. The superior surface of the pituitary gland appeared elevated and convex, with mild rightward deviation of the pituitary stalk.
These findings were consistent with a pituitary macroadenoma. The hypothalamus and optic chiasm appeared normal.
It demonstrated normal morphology of the cerebral and cerebellar hemispheres, with scattered foci of altered signal intensity in the subcortical and deep supratentorial frontoparietal white matter bilaterally. These lesions exhibited high T2/FLAIR signal intensity, isointense T1 signal, and no diffusion restriction on DWI/ADC, suggestive of chronic white matter ischemia.
The ventricular system was normal in size, shape, and position. The brainstem exhibited normal morphology and signal intensity, and the brain cisterns in the posterior cranial fossa and supratentorial region were well-visualized.
Therapeutic intervention (abia)
Description of treatments administered, treatment responses, side effects, and other relevant details.
From February 6, 2024, the patient was initiated on Sandostatin LAR 20 mg administered intramuscularly (I/M) at 28-day intervals for a duration of three months, concluding on April 4, 2024. Following the second dose, laboratory investigations revealed a growth hormone (GH) level of 1908.00 pg/mL and an insulin-like growth factor 1 (IGF-1, Somatomedin-C) level of 310.60 ng/mL.
Given the persistence of elevated IGF-1 levels, the treatment regimen was escalated to Sandostatin LAR 30 mg, administered from May 5 to July 4, 2024, at the same 28-day intervals. A laboratory evaluation on June 28, 2024, demonstrated a further reduction in IGF-1 to 292.90 ng/mL.
Subsequently, the dosage was increased to Sandostatin LAR 40 mg, administered from August 5 to October 4, 2024, with IGF-1 reassessed on August 9, showing a decrease to 238.00 ng/mL. The patient continued on Sandostatin LAR 40 mg, and by November 9, 2024, IGF-1 had further declined to 120.00 ng/mL, achieving normalization.
Outcomes, prognosis, and follow up
The patient was followed up from January 2024 onwards after opting for medical therapy as a choice over surgery. Sandostatin LAR (Octreotide) was prescribed as part of the regimen, with gradual increase according to lab values and improvement clinically. The patient began with 20 mg (Feb–Apr 2024), 30 mg (May–July 2024), and 40 mg (Aug–Dec 2024). Lab work was done at intervals, with radiological follow-up regarding tumor size modification and response to therapy. Research indicates that somatostatin receptor ligands (SRL) like Octreotide can reduce tumor volume in 36–75% of cases [7].
Biochemical control also increased with time, as indicated through reductions in IGF-1 and GH levels. Clinically, stabilization of symptoms, with partial metabolic control improvement and facial feature slowing, resulted. Improvement notwithstanding, however, long-term condition for acromegaly necessitated continued monitoring and long-term care. The final result for the patient constituted a successful response to dose increase therapy, confirming that medical therapy can be a viable alternative for patients not willing or able to undergo surgery (Mayo Clinic Proceedings, 2022).
Discussion
The late diagnosis of the patient highlights the challenge of recognising acromegaly as symptoms develop slowly and are not detected for many years despite repeated medical visits. The choice of medical over surgical treatment is a reflection of individualized treatment regimens, particularly for elderly patients or those with metabolic co-morbidities that increase surgical risk. While transsphenoidal surgery is the initial line of treatment, with 80– 90% remission for microadenomas, medical therapy is a crucial alternative for those with macroadenomas, those who are not candidates for surgery, or those who decline surgery [8]. For this patient, Octreotide (Sandostatin LAR) successfully reduced tumor volume and normalized IGF-1, highlighting the effectiveness of somatostatin receptor ligands (SRLs) for managing acromegaly. Despite the effectiveness, however, there are several limitations that must be kept in mind. One is variability of response to SRL, with partial biochemical control occurring for some patients, necessitating adjunctive therapies or dose adjustments [9]. Longterm safety considerations are significant, as SRL therapy is linked to side effects including gastrointestinal symptoms, gallstone formation, and potential alterations in glucose metabolism, necessitating ongoing surveillance [10]. A further limitation is the brief follow-up duration for this case, which restricts the assessment of long-term sustainability of the achieved improvements, as long-term monitoring for disease recurrence or drug resistance is necessary. Another point is that monotherapy with octreotide alone is all that this case entailed, but some patients will require combination therapy with pegvisomant (a receptor antagonist for GH) or with cabergoline (a dopamine agonist) for best control of disease [11].
For individuals with partial responses to SRLs, alternative therapy should be utilized. Pegvisomant, a GH receptor antagonist, has been effective at normalizing IGF-1, either as monotherapy alone, or as a combination with SRLs, in 80–90% of patients, but is restricted due to high cost and necessity for regular monitoring for liver enzymes [12] Pasireotide, a second-generation SRL, has also been shown to have better control for IGF-1 [13] compared with Octreotide but with greater risk for hyperglycemia [14]. More recently, progress has also been made with oral preparations for SRLs, such as Mycapssa® (octreotide oral capsules), with encouraging biochemical control and greater patient convenience, but with variability for absorption as a drawback [15]. One novel therapy currently being tested is Paltusotine, a once-daily oral nonpeptide SRL, with encouraging normalization for IGF-1 with few side effects, as part of ongoing Phase 3 trials (PATHFNDR-1 and PATHFNDR-2, 2024) [16].
Implications for this case highlight the importance of a multidisciplinary team consisting of endocrinologists, radiologists, and neurosurgeons for optimal outcomes. With continued improvements in medical therapy, new pharmacological agents such as paltusotine and newer oral SRLs have potential for practice-changing improvement with better, more convenient, and better-tolerated therapy for managing acromegaly. Refinement of personalized strategies for those with partial responses to currently available therapies, as well as those not currently amenable to surgery, will depend on further research.
Conclusion
This case highlights the importance of early detection and individualized treatment strategies for acromegaly. While surgery remains the first-line choice for therapy, medical therapy with somatostatin receptor ligands and dose escalation therapy may provide optimal control for nonsurgical candidates (Mayo Clinic Proceedings, 2022) [8]. The findings highlight the necessity for continued screening and multidisciplinary treatment, particularly for those with metabolic comorbidities.
Continued development in medical therapy, including newer preparations of SRL and second-line therapy, offers encouraging options for long-term control of the condition (Pituitary Society Consensus Guidelines, 2024). The case is a helpful model for optimization of treatment protocols for difficult cases of acromegaly, highlighting the role of individualized therapy and careful monitoring toward improvement in patient outcomes.
References
- Melmed S (1990) Acromegaly. N Engl J Med. 322:966-977.
- Gadelha MR, Kasuki L, Lim DST, Fleseriu M (2019) Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr Rev. 40:268-332.
- Holdaway IM, Bolland MJ, Gamble GD (2008) A meta-analysis of the effect of lowering serum levels of GH and IGF-1 on mortality in acromegaly. Eur J Endocrinol.159:89-95.
- Giustina A, Barkhoudarian G, Beckers A, Ben-Shlomo A, Biermasz N, et al. (2020) Multidisciplinary management of acromegaly: a consensus. Rev Endocr Metab Disord. 21:667-678.
- Fleseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, et al. (2016) Hormonal replacement in hypopituitarism in adults: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 101:3888-3921.
- Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, et al. (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 99:3933-3951.
- Melmed S (2006) Medical progress: Acromegaly. N Engl J Med. 355:2558-2573.
- Ershadinia N, Tritos NA (2022) Diagnosis and Treatment of Acromegaly: An Update. Mayo Clin Proc. 97:333-346.
- Giustina A, Barkhoudarian G, Beckers A, Ben-Shlomo A, Biermasz N, et al. (2020) Multidisciplinary management of acromegaly: A consensus. Rev Endocr Metab Disord. 21:667-678.
- Fleseriu M, Langlois F, Lim DST, Varlamov EV, Melmed S (2022) Acromegaly: pathogenesis, diagnosis, and management. Lancet Diabetes Endocrinol. 10:804-826.
- Gadelha MR, Kasuki L, Lim DST, Fleseriu M (2019) Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr Rev. 40:268-332.
- Puig-Domingo M, Bernabéu I, Picó A, Biagetti B, Gil J, et al. (2021) Pasireotide in the Personalized Treatment of Acromegaly. Front Endocrinol (Lausanne). 12:648411.
- Samson SL (2024) Is diabetes with acromegaly for life? Pituitary. 27:433-436.
- Biermasz N, Fleseriu M, Dreval AV, Pokramovich Y, Bondar I, et al. (2021) Oral octreotide capsules lowered incidence and improved severity of acromegaly symptoms compared to injectable somatostatin receptor ligands—results from the MPOWERED trial. Endocrine Abstracts. 5:A522-A523.
- Gillian McGovern, Associate Editor (2024) FDA accepts NDA for paltusotine to treat adult patients with acromegaly. Pharmacy Times.
- Giustina A, Biermasz N, Casanueva FF, Fleseriu M, Mortini P, et al. (2024) Consensus on criteria for acromegaly diagnosis and remission. Pituitary. 27:7-22.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.