Mapping Knowledge Domains of Diabetic Pressure Injuries: A 25-Year Bibliometric and Visualization Analysis
by Guilan Huang1, Shufen Liao1, Jinyan Li1, Shiyun Qin1, Xiaojun Chen1, Shuyan Zeng1, Qin Guo1, Qiuyi Ouyang1, Yongxiang Liu2, Xiaofang Chen1, Fengqiu Gong1*
1The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, 510080, China
2Department of Reproductive Medicine, the First Affiliated Hospital of Guangzhou University of Chinese Medicine, Guangzhou, 510405, China
*Corresponding Author: Fengqiu Gong, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, 510080, China
Received Date: 21 July 2025
Accepted Date: 28 July 2025
Published Date: 30 July 2025
Citation: Huang G, Liao S, Li J, Qin S, Chen X, et al. (2025) Mapping Knowledge Domains of Diabetic Pressure Injuries: A 25-Year Bibliometric and Visualization Analysis J Surg 10: 11398 https://doi.org/10.29011/2575-9760.011398
Abstract
Patients with diabetes are more susceptible to Pressure Injuries (PIs) due to chronic hyperglycemia, neuropathy, microvascular dysfunction, and immune impairment, which contribute to delayed and complex wound healing. This study systematically analyzes research trends, hotspots, and international collaboration patterns in the field of diabetic PIs using bibliometric methods. A total of 410 English-language publications were retrieved from the Web of Science Core Collection through December 5, 2024. CiteSpace, VOSviewer, R, and Bibliometric.com were employed to visualize publication trends, institutional and national distributions, author collaboration networks, high-frequency keywords, and co-citation patterns. Results show a significant increase in publications since 2018, with the United States leading in output and international collaboration, particularly with China and the United Kingdom. Research hotspots primarily focus on “pressure ulcers,” “diabetic foot ulcers,” “risk factors,” and “wound healing.” Cluster and burst keyword analyses revealed three major themes: chronic wound types, pathogenesis and epidemiology, and therapeutic strategies. Emerging research topics include biomaterials, critical care, and predictive modeling. This bibliometric study provides a comprehensive overview of the field, highlights influential contributors, and offers insights into evolving research priorities and future directions.
Keywords: Bibliometrics; Diabetes; Pressure Injury; Research Trends; Wound Healing
Introduction
Pressure Injuries (PIs), also known as pressure ulcers, are localized tissue damage caused by prolonged exposure to pressure, shear, and friction, particularly over bony prominences [1]. In patients with Diabetes Mellitus (DM), the risk and severity of PIs are significantly elevated due to a combination of metabolic and vascular factors, including chronic hyperglycemia, peripheral neuropathy, microangiopathy, and immune dysfunction. Thesefactors collectively contribute to impaired tissue perfusion, sensory dysfunction, and delayed wound healing. Consequently, patients with diabetes are not only more vulnerable to PIs but also face prolonged healing times, higher infection rates, increased mortality, and elevated healthcare costs. These clinical characteristics underscore the urgent need for in-depth research on the relationship between diabetes and pressure injuries [2-4]. In recent years, the global incidence of diabetes has continued to rise, and population aging has further accelerated research related to the disease. Notably, significant progress has been made in understanding the healing mechanisms of diabetic wounds. Many studies have investigated the molecular mechanisms underlying impaired diabetic wound healing and explored novel therapeutic approaches, including exosomes, antimicrobial hydrogels, and tissue engineering [5-7]. Despite continuous advances in this field, the rapid expansion of literature presents challenges in identifying research trends and integrating knowledge. Currently, there is a lack of quantitative analysis to systematically evaluate the research landscape, key topics, and collaboration networks in the field of diabetic pressure injury healing. Bibliometrics is a systematic and quantitative approach used to objectively assess developmental patterns, research structures, and dynamic changes within specific scientific fields. Unlike traditional systematic reviews, which focus on specific clinical or mechanistic issues, bibliometrics enables the construction of knowledge graphs, identification of core research contributors, and detection of research hotspots and emerging trends [8]. Given the continuous increase in basic and clinical studies on diabetic Pressure Injuries (PIs), a comprehensive bibliometric analysis is urgently needed to synthesize existing knowledge, identify key contributors, and guide future research directions. Therefore, this study aimed to conduct a comprehensive bibliometric analysis of the research landscape on diabetic pressure injuries using literature from the Web of Science Core Collection and visualization tools including CiteSpace, VOSviewer, and HistCite. The study investigates publication trends, geographic and institutional distributions, core authors and journals, as well as high-frequency keywords and their temporal evolution, aiming to provide a scientific foundation and reference for future basic, clinical, and translational research.
Materials and Methods
Data Sources and Search Strategy
In this study, English-language literature was retrieved from the Web Of Science (WoS) Core Collection using the search query: TS = (“pressure injury” OR “pressure ulcers” OR “pressure sore” OR “pressure sores” OR “pressure injuries”) AND TS = (“diabetes” OR “diabetic” OR “diabetic mellitus” OR “diabetes mellitus” OR “diabetics”). The search period covered the database’s inception through 5 December 2024. A total of 913 English-language articles were initially identified. Inclusion criteria comprised original research and review articles focused on pressure injuries in patients with type 2 diabetes mellitus (T2D). Exclusion criteria included conference abstracts, book chapters, and studies not directly related to diabetic pressure injuries. Two researchers independently screened the records according to predefined inclusion and exclusion criteria. Duplicate records were removed using the “Remove Duplicates” function in CiteSpace, resulting in 410 English-language articles included for further analysis (Figure 1).
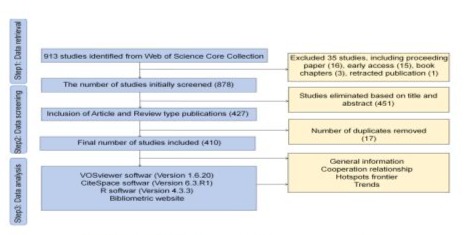
Figure 1: Flow chart of literature screening.
Bibliometric Analysis and Data Visualization
All included literature records were downloaded in the “Full Records and Cited References” format and exported as plain text files. CiteSpace (version 6.3 R1), VOSviewer (version 1.6.20), R (version 4.3.3), and the online platform Bibliometric. com were used for bibliometric analysis and data visualization. Using CiteSpace, this study generated visual knowledge maps illustrating co-occurrence, clustering, and burst detection of authors, institutions, countries/regions, and keywords, along with a dual-map overlay analysis of journals. The time slice was set to one year per slice, covering the period from 1999 to 2024. The threshold (Top N per slice) was set to 50; the pruning algorithm used was Pathfinder, with all other parameters set to default. The international collaboration network among countries was further analyzed and visualized using VOSviewer and Bibliometric.com.
Results and Analysis
Global Research Landscape and National Collaboration Patterns in Diabetic Pressure Injury Studies
Of the 410 analyzed publications, 315 were original research articles and 95 were reviews, contributed by researchers across 44 countries. As shown in Figure 2A, the research output is primarily concentrated in North America, Europe, and parts of Asia. The United States ranked first with 160 publications (32.92%), followed by China (58, 11.93%) and Japan (22, 4.53%) (Supplementary Table 1). Figure 2B shows a steady increase in annual publication volume from 1999 to 2024, with a marked acceleration after 2018, indicating growing academic attention to this field. Among all contributimng countries, 20 countries issued more than five papers (Figure 2C-D). The top 10 countries were compared in terms of publication count, citation frequency, and international collaboration. The United States not only produced the highest number of publications but also had the highest citation count (6,176), demonstrating strong academic influence. Although China published fewer articles (58), its citation count has grown
rapidly (643), indicating increasing international recognition of its research output. Despite a relatively low number of publications, the United Kingdom had a high citation frequency, suggesting high research quality. In the international collaboration network, the United States had the closest ties with China and the United Kingdom and occupied a central position. Germany, although contributing only 15 publications, ranked first in centrality (0.47), highlighting its pivotal role in global scientific collaboration. Notably, Israel and Iran also ranked among the top ten, reflecting growing global attention to the risk assessment and management of diabetic pressure injury. Overall, North America, Europe, and several Asian countries have established a highly interactive, multinational scientific research network in this field (Supplementary Table 1).
|
Rank |
Countries |
Counts |
Year |
Centrality |
Citations |
Total link strength |
|
1 |
USA |
161 |
1999 |
0 |
6176 |
42 |
|
2 |
China |
58 |
2002 |
0 |
643 |
13 |
|
3 |
Japan |
22 |
2001 |
0.01 |
628 |
19 |
|
4 |
England |
21 |
2000 |
0.09 |
2286 |
31 |
|
5 |
Italy |
19 |
2003 |
0.01 |
616 |
27 |
|
6 |
Iran |
16 |
2014 |
0.07 |
274 |
6 |
|
7 |
Germany |
15 |
2001 |
0.47 |
565 |
28 |
|
8 |
Australia |
15 |
2005 |
0.07 |
616 |
24 |
|
9 |
Canada |
13 |
2000 |
0.14 |
392 |
7 |
|
10 |
Israel |
13 |
2009 |
0 |
541 |
10 |
Supplementary Table 1: The top 10 countries by number of published works.
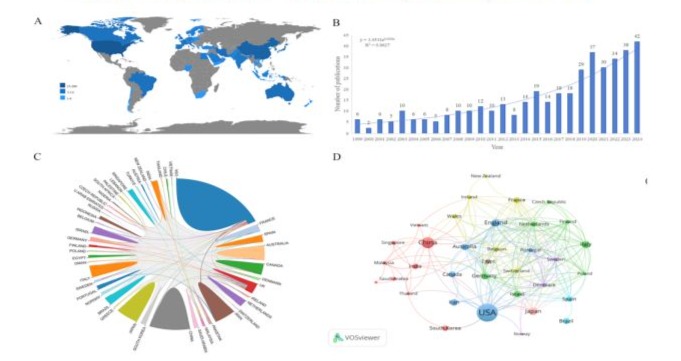
Figure 2: (A) Geographic distribution of diabetic pressure injury, period 1994 to 2024; (B) The number of publication frequency for each year from 1994 to 2024; (C) Global cooperation in publishing; (D) Analysis of countries/regions.
Author Collaboration and Co-Citation Patterns in Diabetic Pressure Injury Research
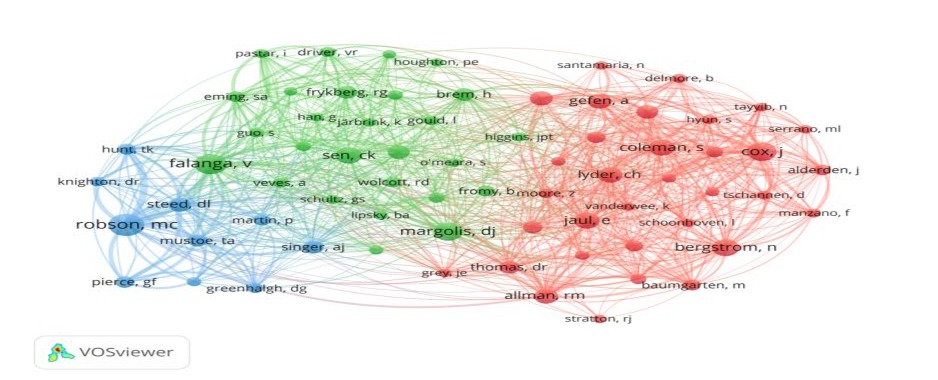
This study utilized CiteSpace to perform an author-level analysis of 410 publications related to diabetic pressure injury, aiming to identify prolific authors and their co-authorship networks. As shown in Figure 3, the co-authorship network comprises 312 nodes and 403 links, with a network density of 0.0083, indicating relatively limited collaboration among research teams. Authors with three or more publications were classified as highly productive. Representative authors include Fromy B, Abdellatif Ahmed, Saumet JL, Breitbart AS, Kerstein MD, Levy Ayelet, and Mason JM, each of whom formed multiple relatively independent collaborative subnetworks. These subnetworks show strong internal cohesion but weak inter-network collaboration, suggesting that the research field remains relatively fragmented. The research team led by Abdellatif Ahmed has made significant contributions to studies on the mechanisms of diabetic pressure injury and the development of novel therapies. The team led by Kerstein MD (1999) focused on chronic wound treatment strategies, including biotherapy, tissue engineering, and home care, and has had a lasting academic impact in this field. The weak connections among major author groups in the overall network further confirm that current collaborations are mostly localized and lack interdisciplinary integration. Supplementary Table 2 lists influential authors in the field, with an average citation rate of 26.93 per article, reflecting strong academic impact. We also conducted an author co-citation analysis. When two authors are cited together in the same publication, they are considered to share a co-citation relationship; the higher the co-citation frequency, the closer their conceptual linkage. To further identify core authors, we extracted 11,610 first-author citation records from 410 publications, resulting in 13,946 total citation events, with a minimum citation threshold of 15. As shown in Supplementary Figure 1, the co-citation analysis generated a network of 70 researchers grouped into three major clusters. The most frequently cited authors were Robson MC (79 citations), Falanga V (67), and Cox J (58).
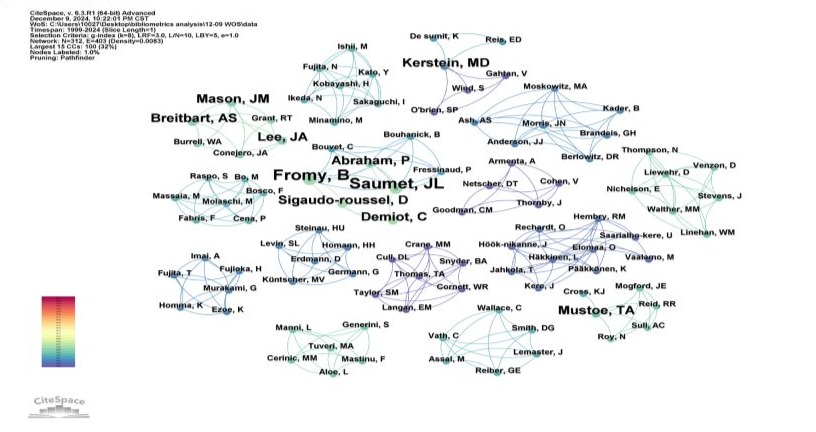
Figure 3: The visualized network of co-authorship of authors in the field of diabetic pressure injury researches. Nodes represent authors, the number of published papers is presented as the size of the node, and the connection represents the existence of a cooperative relationship between the two authors. The more collaborations you have, the thicker the connection. The denser the network of collaboration between authors, the closer the academic collaboration.
|
Rank |
Authors |
Counts |
Year |
Times Cited |
Times Cited |
H-Index |
|
(Total) |
(Average per item) |
|||||
|
1 |
Fromy, B |
4 |
2002 |
128 |
32 |
4 |
|
2 |
Abdellatif, Ahmed |
3 |
2020 |
23 |
7.67 |
3 |
|
3 |
Saumet, JL |
3 |
2002 |
117 |
39 |
3 |
|
4 |
Breitbart, AS |
3 |
2005 |
92 |
30.67 |
3 |
|
5 |
Kerstein, MD |
3 |
1999 |
144 |
48 |
3 |
|
6 |
Levy, Ayelet |
3 |
2016 |
83 |
27.67 |
3 |
|
7 |
Mason, JM |
3 |
2005 |
92 |
30.67 |
3 |
|
8 |
Demiot, C |
2 |
2006 |
55 |
27.5 |
2 |
|
9 |
Albert, Nancy M |
2 |
2017 |
11 |
5.5 |
1 |
|
10 |
Lyle, L Tiffany |
2 |
2021 |
9 |
4.5 |
2 |
Supplementary Table 2: The top 10 authors by number of published works.
Supplementary Figure 1
Core Terminologies and Evolving Trends in Diabetic Pressure Injury Literature
Keyword co-occurrence analysis is effective for identifying research hotspots and developmental trends in the field of diabetic pressure injury. In this study, we used CiteSpace to analyze keywords from 410 articles and generated a co-occurrence network after merging synonyms (Figure 4). The top 10 high-frequency keywords, each appearing more than 28 times, are listed in Table 1. Keyword frequency and first appearance year reflect the importance and evolution of each research topic. Core keywords such as “pressure ulcers”, “risk factors”, “diabetic foot ulcers”, “wound healing”, and “management” appear frequently and serve as key nodes in the co-occurrence network, forming the structural foundation of research hotspots and showing strong connectivity with related terms. Among these, “pressure ulcers” and “risk factors” are the most frequently occurring. “Pressure ulcers” reflect multi-dimensional discussions on chronic wounds and their clinical management, including risk factor identification, nursing interventions, animal model development, and pathological assessment criteria. “Risk factors” primarily relate to risk assessment and preventive strategies in elderly populations and individuals with chronic diseases [9-14]. Additionally, “diabetic foot ulcers” and “wound healing” have received increasing attention in recent studies, reflecting a growing concern for diabetes-related chronic wounds [9,12]. Network centrality analysis indicates that “pressure ulcers” and “diabetic foot ulcers” are structural hubs, playing a central role in maintaining network stability. In summary, current research continues to emphasize the pathogenesis and risk factors of pressure ulcers and chronic wounds, particularly among diabetic patients, the elderly, and long-term bedridden individuals. Simultaneously, increasing efforts have been directed toward understanding wound healing mechanisms and optimizing preventive strategies [10,15,16].
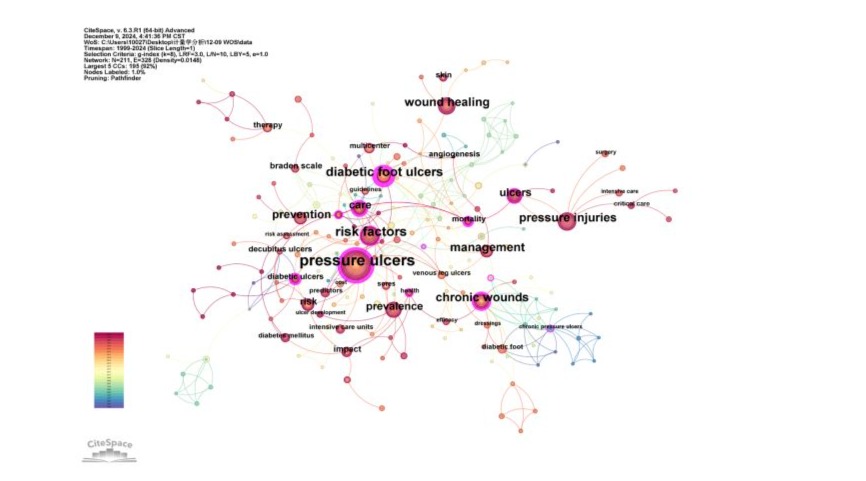
Figure 4: Keyword co-occurrence diagram. Each keyword is usually represented by a node, and the size of the node indicates how often the keyword appears in the literature; The co-occurrence relationship between keywords is represented by a line, and the thickness of the line indicates the number of co-occurrences, and the thicker the line, the higher the co-occurrence frequency of the two keywords, and the closer the relationship. Keywords with large nodes and more connections in the network usually represent research hotspots in the field, and these hot topics are the focus of current scholars.
|
Rank |
Keywords |
Count |
Year |
Centrality |
|
1 |
pressure ulcers |
159 |
2002 |
0.48 |
|
2 |
risk factors |
61 |
2003 |
0.2 |
|
3 |
diabetic foot ulcers |
50 |
2002 |
0.68 |
|
4 |
pressure injuries |
48 |
2017 |
0.1 |
|
5 |
chronic wounds |
46 |
2004 |
0.27 |
|
6 |
wound healing |
46 |
2014 |
0.08 |
|
7 |
management |
41 |
1999 |
0.03 |
|
8 |
prevention |
38 |
2009 |
0.07 |
|
9 |
prevalence |
32 |
2014 |
0.07 |
|
10 |
ulcers |
29 |
2017 |
0.13 |
Table 1: The top 10 high-frequency keywords in the research frequency of diabetic pressure injury from 1999 to 2024.
Multistage development in 25 years of keyword evolution (1999-2024)
To more effectively refine research topics related to diabetic pressure injury, this study employed keyword clustering analysis using CiteSpace. Cluster numbers begin with #0 (the largest cluster) and decrease in size sequentially. Based on literature from 1999 to 2024, a keyword co-occurrence network was constructed using the Pathfinder algorithm with a 1-year time slice (Figure 5A). A total
of 10 clusters were identified, comprising 211 nodes and 328 links. The modularity (Q value) of 0.7639 indicates a well-defined clustering structure with reasonable separation. The average silhouette score was 0.8895/0.8937 (timeline chart), suggesting high internal consistency and strong reliability of the clusters. Keywords in cluster #0 include “diabetic foot ulcers”, “foot ulcers” “multicenter”, “platelet-rich plasma”, and “efficacy”. For details of keywords in other clusters, see Supplementary Table 3. These ten clusters can be grouped into three major research directions: (1) chronic wound types, including diabetic foot ulcers, diabetic ulcers, pressure ulcers, and pressure injuries. This line of research emphasizes innovative therapies, identification of key risk factors, and both technical and economic challenges associated with chronic wound management [17,18]. These studies underscore the clinical significance and societal burden of chronic wounds, providing valuable guidance for management and future investigations [14,19,20]. (2) Pathological mechanisms and epidemiology, covering complications, prevalence, risk factors, and endothelial dysfunction. The study examined the significant impact of chronic diseases (such as cardiovascular disease, diabetes, and kidney disease) and complications (including anemia, malnutrition, and incontinence) on the development of pressure ulcers in older adults. Studies indicate that chronic diseases significantly elevate the risk of pressure ulcers in the elderly, particularly in individuals with diabetes, and support the need for a multidisciplinary prevention strategy [9,21,22]. (3) Wound treatment and tissue repair, including topics such as biofilm formation and tissue regeneration. This research area focuses on the efficacy and mechanisms of novel biomaterials and molecular interventions [23]. Based on 410 publications from the Web of Science Core Collection, the CiteSpace keyword burst detection algorithm was applied to identify research highlights. After merging synonyms and setting the minimum burst duration to two years, 19 keywords with the highest burst intensities were identified (Figure 5B). Keywords with a burst intensity greater than 3.5 included “chronic pressure ulcers”, “risk”, “prevalence”, “pressure injuries”, and “ulcers”. Those with burst durations longer than four years were “chronic pressure ulcers” ,“chronic wounds”, “diabetic foot ulcers”, “prevalence”, and “predictors”. Keywords that remained active in recent years include “prevalence”, “predictors”, “pressure injuries”, “critical care”, “risk factors”, and “intensive care units”. The keyword time-zone map (Figure 5C) illustrates the dynamic evolution of research focus in this field over the past 25 years, which can be broadly categorized into three stages. During the first stage (1999-2007), keywords such as “management”, “care”, “diabetic foot ulcers”, “risk factors”, and “chronic wounds” reflected a primary emphasis on risk assessment and the treatment of pressure ulcers and chronic wounds [24,25]. In the second stage (2008-2015), the emergence of keywords like “prevention”, “therapy”, “wound healing”, “prevalence”, and “mortality” indicated a research shift toward epidemiological characteristics, predictive models, treatment strategies, and the economic burden of disease, contributing to the advancement of precision care [15,21,26,27]. In the most recent stage (2016-2024), research has increasingly focused on integrating risk prediction models with epidemiology, as highlighted by keywords such as “intensive care units”, “impact”, “predictors”, and “hospitalized patients”. Moreover, this phase marks a growing interest in novel therapeutic approaches, including nanostructured bioactive glass composite hydrogel membranes [28-30].
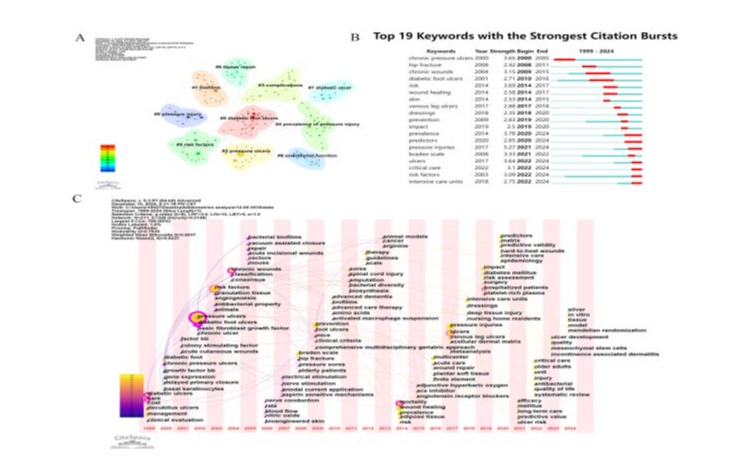
Figure 5: Analysis of keywords. (A) Keyword visualization clusters related to diabetic pressure injury; (B) The strongest citation burst; (C) The timeline viewer related to keywords.
|
Rank |
Cluster |
Size |
Slihouette |
Mean |
Top Terms (log-likelihood ratio, p-level) |
|
(Year) |
|||||
|
1 |
0 |
28 |
0.796 |
2010 |
diabetic foot ulcers ; foot ulcers; multicenter; platelet-rich plasma ; efficacy |
|
2 |
1 |
19 |
0.944 |
2013 |
biofilms; chronic wounds; polihexanide; identification; debridement |
|
3 |
2 |
19 |
0.961 |
2011 |
pressure ulcers ; hypertension; basic fibroblast growth factor; support surfaces; pressure sore |
|
4 |
3 |
18 |
0.808 |
2019 |
complications; trauma; diagnostic; vertebral fracture; caregiver |
|
5 |
4 |
18 |
0.796 |
2014 |
risk factor; wound healing; dehydration; pressure ulcer risk; prevalence of pressure injury |
|
6 |
5 |
17 |
0.831 |
2013 |
risk factors; epidemiology; older people; advanced dementia; public health |
|
7 |
6 |
14 |
0.948 |
2001 |
chronic pressure ulcers; extremity diabetic ulcers; growth factor bb; tissue repair; keratinocytes |
|
8 |
7 |
13 |
0.811 |
2014 |
diabetic ulcer; decubitus ulcer ; venous ulcer; cysteine; acceleration |
|
9 |
8 |
12 |
1 |
2006 |
endothelial function; vasodilation; blood flow; microcirculation; diabetes |
|
10 |
9 |
9 |
1 |
2020 |
pressure injury; icu; critical care; post-acute care; inpatient rehabilitation facilities |
Supplementary Table 3: Keyword cluster analysis based on co-occurrence data from diabetic pressure injury research using CiteSpace. Each row represents a keyword cluster ranked by size.
Institutional Collaboration Network Reveals Global Research Hubs and Evolving Partnership Trends
This study employs the Institution module in CiteSpace to analyze research institutions involved in diabetic pressure injury, with the threshold set at 8. As shown in Figure 6, the collaboration network comprises 184 nodes and 113 links, with a network density of 0.0067, indicating relatively weak inter-institutional collaboration. Leading institutions in publication volume include the Centre National de la Recherche Scientifique, Boston University, the University of California system, and Cardiff University. These institutions demonstrate strong expertise in clinical medicine, public health, and biomedical research. According to Supplementary Table 4, most top institutions are based in Europe and North America-particularly the United States, France, and the United Kingdom-highlighting the international nature of research in this field. The peak period of institutional collaboration occurred between 2000 and 2010, followed by a gradual expansion across regions and disciplines. Notably, participation from developing countries has increased in recent years; for instance, the Egyptian Knowledge Bank (EKB) has been active since 2011. Nevertheless, the current institutional collaboration network remains relatively fragmented. Strengthening cross-institutional and cross-regional collaboration is essential for advancing research and development in the field of diabetic pressure injury.

Figure 6: Institutional Collaboration Mapping Analysis. Node size is proportional to the number of publications from each institution, while link thickness represents the strength of collaboration.
|
Rank |
Count |
Year |
Institutions |
|
1 |
5 |
2006 |
Centre National de la Recherche Scientifique (CNRS) |
|
2 |
5 |
2001 |
Boston University |
|
3 |
5 |
2018 |
University of California System |
|
4 |
5 |
2003 |
Cardiff University |
|
5 |
4 |
2003 |
Institut National de la Sante et de la Recherche Medicale (Inserm) |
|
6 |
4 |
2002 |
Icahn School of Medicine at Mount Sinai |
|
7 |
4 |
2004 |
Columbia University |
|
8 |
4 |
2005 |
Rutgers University New Brunswick |
|
9 |
4 |
2011 |
Egyptian Knowledge Bank (EKB) |
|
10 |
4 |
2009 |
Hebrew University of Jerusalem |
Supplementary Table 4: Top 10 institutions in the number of publications.
Core Journal Clusters and Citation Pathways in Diabetic Pressure Injury Research
Co-citation analysis identified the most influential journals in the field, with Wound Repair and Regeneration, International Journal of Wound Care, Journal of Wound Nursing, Advances in Skin and Wound Nursing, Plastic and Reconstructive Surgery, and Advances in Wound Care being the most frequently cited. Three major clusters emerged in the co-citation network (Figure 7A). The largest cluster (red) focuses on wound management and geriatrics, led by the International Wound Journal, and includes studies on various wound types, pathophysiology, and care strategies. The second cluster (green) centers on wound healing, dermatology, and reconstructive surgery, with Wound Repair and Regeneration and Plastic and Reconstructive Surgery as representative journals. The third cluster (blue) highlights innovations in wound care, including care technologies, product applications, and biomaterials, with Advances in Wound Care and Biomaterials as core journals. The overlay visualization (Figure 7B) depicts interdisciplinary knowledge flow among journals. The yellow path indicates frequent citations from molecular and immunology journals to those in health, nursing, and medicine, while the green path represents citations to clinical medical journals. The Health, Nursing, and Medicine category shows the highest citation impact in the field (Supplementary Table 5).
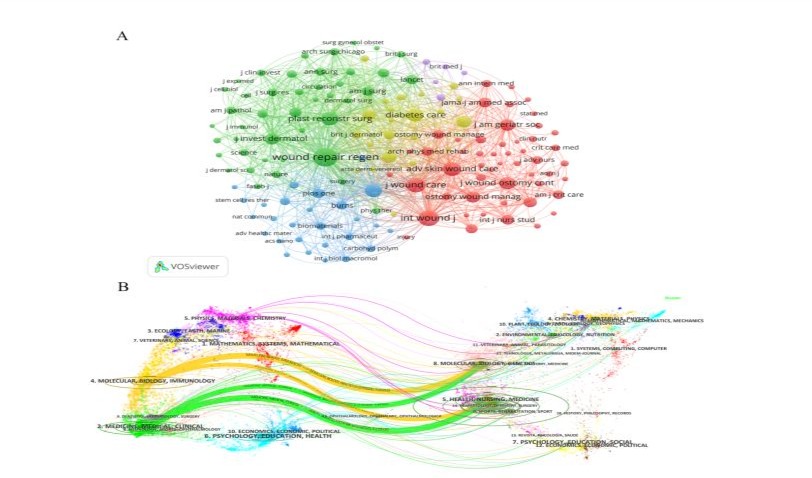
Figure 7: Analysisi of co-cited journals. The dual-map overlay of journals related to diabetic pressure injury. Different colors represent different clusters, and the larger the node, the more times it will be co-cited. The thicker the line, the stronger the relationship between them.
|
Citing region |
Cited region |
Z-score |
|
molecular, biology, immunology |
molecular, biology, genetics |
3.971 |
|
molecular, biology, immunology |
health, nursing, medicine |
1.985 |
|
medicine, medical, clinical |
molecular, biology, genetics |
2.935 |
|
medicine, medical, clinical |
health, nursing, medicine |
5.583 |
Supplementary Table 5: Citation trends at a domain level.
Co-Citation Cluster Analysis Reveals Core Themes And Temporal Evolution in Diabetic Pressure Injury Research
A co-citation analysis of 410 publications was conducted using CiteSpace, resulting in a network comprising 371 nodes and 637 links. Ten major topic clusters were identified, demonstrating a well-defined structure modularity Q = 0.9294; average silhouette = 0.9763), indicating high clustering quality (Figure 8A). The largest cluster, #0 “risk factor,” reflects strong co-citation intensity around riskrelated research. A lower cluster number generally corresponds to higher relative importance in diabetic pressure injury research. Early research hotspots focused on clusters such as #8 “age-related changes” (1997), #4 “accelerated healing” (2001), and #7 “stressinduced cutaneous vasodilation” (2002). Mid-stage topics were represented by clusters including #9 “care” (2007), #6 “elderly person” (2014), #2 “infected diabetic pressure ulcer” (2016), and #0 “risk factor” (2016). Recent hotspots have shifted toward #1 “retrospective cohort study” (2018), #3 “intensive care patients” (2020), and #5 “chronic wound study” (2021), reflecting an increasing emphasis on clinical evidence, critical care, and chronic wound management in diabetic patients. These clusters revealed several pivotal studies that significantly contributed to the understanding of diabetic pressure injury. For example, Han G (2017), Armstrong DG (2017), and Mervis JS (2019) produced influential findings that advanced research in this field. The top 10 most-cited publications (Table 2) are primarily concentrated in clusters #0, #1, #2, #3, and #6, reflecting the evolution of the knowledge base and shifts in research focus within the field.
The emergent analysis (Figure 8B) illustrates the evolving research focus and the influence of key publications in the field of diabetic pressure injury. Nussbaum et al. (2018) exhibited the strongest citation burst (intensity = 5.7, 2020-2022), underscoring the clinical and economic urgency of the disease. Other key emergent works, such as Jaul et al. (2018) (intensity = 5.47), and more recent studies by Wei M (2020), Mervis JS (2019), and Chaboyer WP (2018), highlight growing attention to issues including prevalence, risk prediction, and aging populations. Crimson nodes represent emergent literature identified by the Kleinberg algorithm, marking pivotal turning points in the research field. Emerging themes such as “risk factor,” “ICU patient,” and “retrospective cohort study” are primarily concentrated in clusters #0, #1, #2, #3, and #6 (Supplementary Figure 2). Notably, cluster #1 shows a strong citation connection to literature published in 2022, with a citation share exceeding 12%, indicating its cutting-edge relevance (Supplementary Table 6). Scholars such as Mervis JS and Edsberg LE have substantial influence in the field and represent leading contributors to ongoing research.
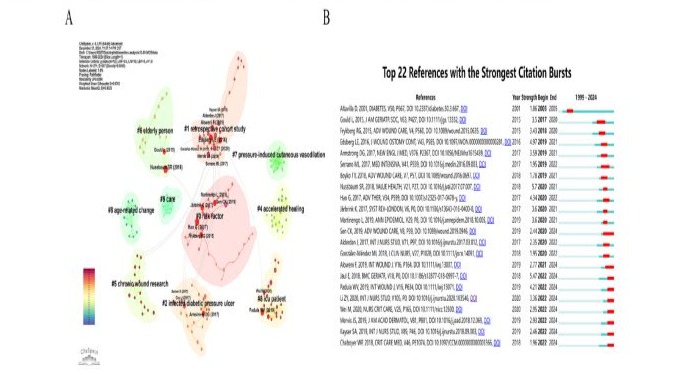
Figure 8: Co-citation cluster analysis and citation burst detection of references in diabetic pressure injury research.
|
Rank |
Counts |
Centrality |
Cited References |
Cluster# |
|
1 |
11 |
0.08 |
Nussbaum SR, 2018, |
0 |
|
2 |
11 |
0.03 |
Han G, 2017, |
1 |
|
3 |
11 |
0 |
Jaul E, 2018, |
6 |
|
4 |
10 |
0.07 |
Padula WV, 2019, |
3 |
|
5 |
8 |
0.08 |
Li ZY, 2020, |
0 |
|
6 |
8 |
0.07 |
Aloweni F, 2019, |
2 |
|
7 |
8 |
0.05 |
Gould L, 2015, |
6 |
|
8 |
8 |
0.01 |
Sen CK, 2019, |
1 |
|
9 |
7 |
0.6 |
Mervis JS, 2019, |
1 |
|
10 |
7 |
0.06 |
Frykberg RG, 2015, |
0 |
Table 2: Top 10 most frequently co-cited references.
|
Coverage |
GCS |
LCS |
Bibliography |
|
12 |
8 |
0 |
Amini, M (2022.0-JAN) Factors affecting the incidence and prevalence of pressure ulcers in covid-19 patients admitted with a braden scale below 14 in the intensive care unit: retrospective cohort study.INTERNATIONAL WOUND JOURNAL, V19, P16 DOI 10.1111/iwj.13804 |
|
11 |
33 |
0 |
Chung, M (2022.0-JAN) Risk factors for pressure injuries in adult patients: a narrative synthesis. INTERNATIONAL JOURNAL OF ENVIRONMENTAL RESEARCH AND PUBLIC HEALTH, V19, P17 DOI 10.3390/ijerph19020761 |
|
6 |
29 |
0 |
Cox, J (2022.0-JAN) Pressure injuries in critical care patients in us hospitals results of the international pressure ulcer prevalence survey.JOURNAL OF WOUND OSTOMY AND CONTINENCE NURSING DOI 10.1097/ WON.0000000000000834 |
|
4 |
8 |
0 |
Yang, Q (2022.0-JAN) Incidence and risk factors associated with hospital-acquired pressure ulcers following total hip arthroplasty: |
|
a retrospective nationwide inpatient sample database study.JOURNAL OF TISSUE VIABILITY DOI 10.1016/j. jtv.2022.01.004 |
|||
|
4 |
7 |
0 |
Xu, W (2022.0-JAN) A nomogram prediction of pressure injury in critical ill patients: a retrospective cohort study. INTERNATIONAL WOUND JOURNAL DOI 10.1111/iwj.13680 |
Supplementary Table 6: Citing articles of cluster #1 retrospective cohort study.

Supplementary Figure 2
Discussion
Pressure Injuries (PIs) in patients with Diabetes Mellitus (DM) remain a significant clinical challenge. Owing to vascular and metabolic dysfunction, individuals with DM are more prone to chronic, non-healing PIs, leading to elevated infection rates and substantial healthcare burdens. This study presents a bibliometric analysis of 410 publications from the Web of Science Core Collection, providing a comprehensive overview of research trends and emerging hotspots in the field. The findings indicate a continuous growth in literature on Diabetic Pressure Injury (DPI) from 1999 to 2024, reflecting increasing global attention to this clinical issue. During the early stage (1999-2010), research primarily focused on identifying risk factors for pressure injuries, with diabetes recognized as a major contributor to delayed wound healing. Subsequently, risk prediction models were introduced to explore the association between pre-existing diabetes and postoperative complications or chronic conditions in patients with pressure injuries. Between 2018 and 2024, the field experienced rapid development, with a notable increase in publication output, peaking in 2024. This phase also witnessed the introduction of multidisciplinary approaches-such as Mendelian randomization and finite element analysis-to investigate the mechanisms linking diabetes to pressure injury risk. The bibliometric analysis revealed marked regional disparities. Research was mainly concentrated in North America, Europe, and parts of Asia, with the United States, Germany, the United Kingdom, and China leading in publication output. This dominance may be attributed to well-established biomedical infrastructures and robust health data systems in these countries. However, a gap remains between China and Western nations in terms of highly cited institutions, underscoring the need for deeper research and broader international collaboration. Although Latin America and parts of Africa have contributed to the field, overall research activity in these regions remains limited [27]. In terms of academic influence, Kerstein MD (1999) ranks first in citation impact, with 144 citations. His team’s work on chronic wound treatment-spanning biologic therapies, tissue engineering, and home care-has exerted a lasting influence. Similarly, Fromy B (2002) and Saumet JL (2002), cited 128 and 117 times respectively, laid important foundations for the field in the early 2000s. In contrast, more recent contributors such as Levy Ayelet (2016) and Albert Nancy M (2017) are beginning to demonstrate academic influence, although their citation counts are still in the early accumulation phase due to the recency of their publications. Current literature primarily focuses on the epidemiology, risk factors, economic burden, and management strategies of chronic wounds and Pressure Injuries (PIs) [21,27,31]. A meta-analysis of 67 studies identified several risk factors significantly associated with PIs-including non-blanchable erythema, low Body Mass Index (BMI<18.5), anemia, hypoalbuminemia, and diabetes-emphasizing the importance of evidence-based nursing interventions in PI prevention. Additionally, high-risk factors for perioperative PIs-such as cardiovascular and respiratory diseases, diabetes, anemia, and prolonged operative time-have been summarized, with individualized prevention strategies recommended for high-risk populations, including orthopedic and COVID-19 patients. During the COVID-19 pandemic, a retrospective cohort study of ICU patients reported a PI incidence as high as 79.7%, which was significantly associated with hospital stay duration, Braden score, diabetes, and fecal incontinence, highlighting the need for heightened PI prevention during public health emergencies [3235]. Diabetic patients are at higher risk of developing PIs and chronic non-healing wounds, with clinical studies showing a 1.5- to 2-fold increased risk compared to non-diabetic individuals [3,4]. In the author collaboration network, the team led by Fromy B and Saumet JL elucidated the impairment of Pressure-Induced Vasodilation (PIV) in diabetes and aging, highlighting its physiological relevance in PI prevention. PIV, a protective mechanism that enhances skin perfusion under low-pressure conditions, is diminished under hyperglycemic states. Animal studies further demonstrated that aldose reductase inhibitors, such as Sorbinil, improve both PIV and neurological function, suggesting potential therapeutic applications [36]. Co-citation analysis indicates that highly cited articles typically form the core of the knowledge structure, representing foundational theoretical, methodological, or practical contributions. As shown in Supplementary Table 6, the most frequently cited studies are those by Nussbaum SR (2018), Han G (2017), and Jaul E (2018) [37]. Jaul emphasized that the development of Pressure Injuries (PIs) is a multifactorial process involving limited mobility, tissue hypoperfusion, and chronic comorbidities such as diabetes, cardiovascular disease, chronic kidney disease, neurodegenerative disorders, and malnutrition. These conditions significantly increase PI risk in older adults by accelerating functional decline and impairing immune response and tissue repair. Specifically, diabetic neuropathy, sarcopenia, and chronic anemia contribute to sensory loss, tissue hypoxia, and immunosuppression, further complicating wound healing [9]. Han G further noted that normal wound healing depends on tightly regulated phases, including inflammation, proliferation, and remodeling. However, in individuals with diabetes, this process is severely disrupted by factors such as hyperglycemia, impaired angiogenesis, oxidative stress, neuropathy, immune dysregulation, and the accumulation of Advanced Glycation End-Products (AGEs), resulting in exacerbated tissue damage and delayed wound closure [38]. Currently, research on the treatment and management of Pressure Injuries (PIs) is increasingly focused on the efficacy and mechanisms of novel biomaterials and molecular interventions.
For instance, a type I collagen matrix embedded with the antimicrobial agent Polyhexamethylenediamine (PCMP) significantly promotes wound healing, reducing the average wound area by 73% and achieving complete closure in 37% of cases [39]. Basic Fibroblast Growth Factor (bFGF) significantly accelerates the healing of pressure ulcers and demonstrates superior outcomes in granulation tissue formation and epithelialization compared to controls, indicating strong clinical potential [40]. Gene transfection with Platelet-Derived Growth Factor B (PDGF-B) significantly enhances angiogenesis and collagen remodeling, offering valuable therapeutic potential for diabetic wound repair.23 Grave et al. reviewed the global epidemiology and economic burden of chronic wounds and advocated for improved health policies and resource allocation to enhance the systematization and accessibility of chronic wound care [27]. Alam, W. proposed a multi-layered strategy based on the TIME framework (tissue status, inflammation/ infection control, moisture balance, and wound edge advancement), emphasizing the importance of nutritional support and palliative care [31]. With advances in medical science and technology, researchers are exploring more precise treatment strategies by integrating epidemiological analysis and risk prediction models, aiming to develop novel therapeutic approaches for refractory wounds. Among these, molecular targeting, genetic association studies, and biomechanical modeling have gained increasing attention. In biomechanics, Levy and Ayele applied finite element analysis to assess the effects of various protective strategies in reducing tissue stress and deformation in individuals with diabetes and other high-risk groups [41]. Han et al. also evaluated advanced wound therapies, including growth factor treatments, skin substitutes, Negative Pressure Wound Therapy (NPWT), and Hyperbaric Oxygen Therapy (HBOT). Despite promising results in some studies, high costs, limited large-scale clinical validation, and inconsistent insurance coverage remain major barriers to widespread adoption [38]. This study employed bibliometric methods to systematically analyze academic development trends, collaboration networks, and knowledge structures in the field of diabetic pressure injury research. Future research should incorporate additional database resources and utilize diverse analytical tools to construct a more comprehensive perspective, thereby facilitating the development of effective prevention strategies and ultimately improving the quality of life for diabetic patients. This study also acknowledges that current evaluation methods may not fully capture the field’s dynamic evolution. Therefore, future studies may consider integrating qualitative research approaches to enable in-depth exploration and multidimensional understanding of the topic, thereby expanding the cognitive boundaries of emerging issues.
Acknowledgments: The authors thank colleagues for their academic advices.
Funding: This work was supported by grants from the Medical Scientifc Research Foundation of Guangdong Province of China (Grant ID A2025221) and Administration of Traditional Chinese Medicine of Guangdong Province (Grant no. 20241103).
Conflict of interest: The authors declare no conflict of interest.
Data availability statement: All data are presented in this article/ Supplementary Material.
Ethics approval and consent to participate: Not applicable.
References
- Allman RM (1997) Pressure ulcer prevalence, incidence, risk factors, and impact. Clin Geriatr Med 13: 421-436.
- Alfonso AR, Kantar RS, Ramly EP, Daar DA, Rifkin WJ, et al. (2019) Diabetes is associated with an increased risk of wound complications and readmission in patients with surgically managed pressure ulcers. Wound Repair Regen 27: 249-256.
- Liu P, He W, Chen HL (2012) Diabetes mellitus as a risk factor for surgery-related pressure ulcers: a meta-analysis. J Wound Ostomy Continence Nurs 39: 495-499.
- Nasiri E, Mollaei A, Birami M, Lotfi M, Rafiei MH (2021) The risk of surgery-related pressure ulcer in diabetics: A systematic review and meta-analysis. Ann Med Surg (Lond) 65: 102336.
- Parella K, Moody K, Wortel D, Colegrove H, Elser JA (2023) HOXA3 accelerates wound healing in diabetic and aged non-diabetic mammals. Sci Rep 13: 9923.
- Song Y, You Y, Xu X, Lu J, Huang X, et al. (2023) Adipose-Derived Mesenchymal Stem Cell-Derived Exosomes Biopotentiated Extracellular Matrix Hydrogels Accelerate Diabetic Wound Healing and Skin Regeneration. Adv Sci (Weinh) 2023;10: e2304023.
- Cruz TB, Carvalho FA, Matafome PN, Soares RA, Santos NC et al. (2021) ( Mice with Type 2 Diabetes Present Significant Alterations in Their Tissue Biomechanical Properties and Histological Features. Biomedicines 10.
- Roldan-Valadez E, Salazar-Ruiz SY, Ibarra-Contreras R, Rios C (2019) Current concepts on bibliometrics: a brief review about impact factor, Eigenfactor score, CiteScore, SCImago Journal Rank, SourceNormalised Impact per Paper, H-index, and alternative metrics. Ir J Med Sci 188: 939-951.
- Jaul E, Barron J, Rosenzweig JP, Menczel J (2018) An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr 18: 305.
- Morton LM, Phillips TJ (2016) Wound healing and treating wounds: Differential diagnosis and evaluation of chronic wounds. J Am Acad Dermatol. 74: 589-605; quiz 605-586.
- Nunan R, Harding KG, Martin P (2014) Clinical challenges of chronic wounds: searching for an optimal animal model to recapitulate their complexity. Dis Model Mech 7: 1205-1213.
- Tschannen D, Bates O, Talsma A, Guo Y (2012) Patient-specific and surgical characteristics in the development of pressure ulcers. Am J Crit Care 21: 116-125.
- Alderden J, Rondinelli J, Pepper G, Cummins M, Whitney J (2017) Risk factors for pressure injuries among critical care patients: A systematic review. Int J Nurs Stud 71: 97-114.
- Powers JG, Higham C, Broussard K, Phillips TJ (2016) Wound healing and treating wounds: Chronic wound care and management. J Am Acad Dermatol. 74: 607-625.
- Boateng J, Catanzano O (2015) Advanced Therapeutic Dressings for Effective Wound Healing--A Review. J Pharm Sci 104: 3653-3680.
- Duscher D, Neofytou E, Wong VW, Maan ZN, Rennert RC et al. (2015) Transdermal deferoxamine prevents pressure-induced diabetic ulcers. Proc Natl Acad Sci U S A 112: 94-99.
- Uchi H, Igarashi A, Urabe K, Koga T, Nakayama J, et al. (2009) Clinical efficacy of basic fibroblast growth factor (bFGF) for diabetic ulcer. Eur J Dermato l19: 461-468.
- Gardner SE, Frantz RA, Schmidt FL (1999) Effect of electrical stimulation on chronic wound healing: a meta-analysis. Wound Repair Regen 7: 495-503.
- Coleman S, Gorecki C, Nelson EA, Closs SJ, Defloor T, et al. (2013) Patient risk factors for pressure ulcer development: systematic review. Int J Nurs Stud. 50: 974-1003.
- Lo ZJ, Lim X, Eng D, Car J, Hong Q, et al. (2020) Clinical and economic burden of wound care in the tropics: a 5-year institutional population health review. Int Wound J 17: 790-803.
- Afzali Borojeny L, Albatineh AN, Hasanpour Dehkordi A, Ghanei Gheshlagh R. (2020) The Incidence of Pressure Ulcers and its Associations in Different Wards of the Hospital: A Systematic Review and Meta-Analysis. Int J Prev Med 11: 171.
- Demiot C, Tartas M, Fromy B, Abraham P, Saumet JL, et.al. (2006) Aldose reductase pathway inhibition improved vascular and C-fiber functions, allowing for pressure-induced vasodilation restoration during severe diabetic neuropathy. Diabetes 55: 1478-1483.
- Lee JA, Conejero JA, Mason JM, Parrett BM, Wear-Maggitti KD, et al. (2005) Lentiviral transfection with the PDGF-B gene improves diabetic wound healing. Plast Reconstr Surg 116: 532-538.
- Hajhosseini B, Longaker MT, Gurtner GC (2020) Pressure Injury. Ann Surg 271: 671-679.
- Cox J (2017) Pressure Injury Risk Factors in Adult Critical Care Patients: A Review of the Literature. Ostomy Wound Manage 63: 3043.
- Ranzani OT, Simpson ES, Japiassu AM, Noritomi DT, Amil Critical Care G (2016) The Challenge of Predicting Pressure Ulcers in Critically Ill Patients. A Multicenter Cohort Study. Ann Am Thorac Socv13: 17751783.
- Graves N, Phillips CJ, Harding K (2022) A narrative review of the epidemiology and economics of chronic wounds. Br J Dermatol 187: 141-148.
- Huang C, Luo P, Zhu X, Li N, Ouyang K, et al. (2024) Causal effect of obesity and adiposity distribution on the risk of pressure ulcers and potential mediation by type 2 diabetes mellitus: insights from multivariable mendelian randomization and mediation analysis. Arch Dermatol Res 316: 550.
- Cox J (2020) Risk Factors for Pressure Injury Development Among Critical Care Patients. Crit Care Nurs Clin North Am 32: 473-488.
- Bargavi P, Balakumar S, Raghunandhakumar S (2024) Multi-functional bandage - bioactive glass/metal oxides/alginate composites based regenerative membrane facilitating re-epithelialization in diabetic wounds with sustained drug delivery and anti-bactericidal efficacy. Int J Biol Macromol 262: 130054.
- Alam W, Hasson J, Reed M (2921) Clinical approach to chronic wound management in older adults. J Am Geriatr Soc 69: 2327-2334.
- Chung ML, Widdel M, Kirchhoff J, Sellin J, Jelali M, et al. (2022) Risk Factors for Pressure Injuries in Adult Patients: A Narrative Synthesis. Int J Environ Res Public Health 19.
- Haisley M, Sorensen JA, Sollie M (2020) Postoperative pressure injuries in adults having surgery under general anaesthesia: systematic review of perioperative risk factors. Br J Surg 107: 338-347.
- Amini M, Mansouri F, Vafaee K, Janbakhsh A, Mahdavikian S, et al. (2022) Factors affecting the incidence and prevalence of pressure ulcers in COVID-19 patients admitted with a Braden scale below 14 in the intensive care unit: Retrospective cohort study. Int Wound J. 19: 2039-2054.
- Ding L, Hu X, Wei L, Sun M, Sun G, et al. (2022) Risk factors for hospital-acquired and community-acquired pressure injuries: a multicentre mixed case-control study. BMJ Open 12: e057624.
- Fouchard M, Misery L, Le Garrec R, Sigaudo-Roussel D, Fromy B. (2019) Alteration of Pressure-Induced Vasodilation in Aging and Diabetes, a Neuro-Vascular Damage. Front Physiol 10: 862.
- Nussbaum SR, Carter MJ, Fife CE, DaVanzo J, Haught R, et al (2018) An Economic Evaluation of the Impact, Cost, and Medicare Policy Implications of Chronic Nonhealing Wounds. Value Health 21: 27-32.
- Han G, Ceilley R (2017) Chronic Wound Healing: A Review of Current Management and Treatments. Adv Ther 34: 599-610.
- Oropallo AR (2019) Use of Native Type I Collagen Matrix Plus Polyhexamethylene Biguanide for Chronic Wound Treatment. Plast Reconstr Surg Glob Open 7: e2047.
- Ohura T, Nakajo T, Moriguchi T, Oka H, Tachi M, Jr., et al. (2011) Clinical efficacy of basic fibroblast growth factor on pressure ulcers: case-control pairing study using a new evaluation method. Wound Repair Regen 19: 542-551.
- Levy A, Schwartz D, Gefen A (2017) The contribution of a directional preference of stiffness to the efficacy of prophylactic sacral dressings in protecting healthy and diabetic tissues from pressure injury: computational modelling studies. Int Wound J 14: 1370-1377.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.