Managing the Significant Challenge of Post-Cardiotomy Uncontrolled Hemorrhage: A Case Report and Literature Review
by Said Khallikane1*, Younes Aissaoui2, Ayoub Belhadj3, Abdessamad Abdou4, Noureddine Atmani5, Hamid Jalal6, Reda Mounir7, Hicham Kbiri8, Mehdi Didi8, Ayoub Dahioui9, Youssef Qamouss10
1Former anesthesiologist, Professor of Anesthesia-Intensive Medicine, Cardiothoracic Anesthesiologist Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco, Previous former anesthesiologist-intensivist, Hassan II Military Hospital, Layun 70000, Morocco, Anesthesiology-ICU-Emergency ex-former, Mohammed VI Hospital, Dakhla 73000, Morocco Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech, Morocco
2Head of Medical ICU, Professor of Anesthesiology-Critical Care, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco
3Head of Surgical ICU, Professor of Anesthesiology-Critical Care, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco
4Head of Cardiothoracic and Vascular Surgeon, Professor of Cardiac Surgery, mini-invasive Cardiac Surgery, Interventional Cardiovascular Surgery, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco
5Cardiothoracic and Vascular Surgeon, Professor of Cardiac Surgery, mini-invasive Cardiac Surgery, Interventional Cardiovascular Surgery, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000– Sidi Mohamed Beni Abdellah University, Faculty of Medicine and Pharmacy of Fes, Kingdom of Morocco
6Cardiologist, Cardio-echocardiographic, Professor of Cardiology, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Morocco
7Cardiothoracic and Vascular Surgeon, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000., Mohammed V University, Faculty of Medicine and Pharmacy of Rabat 10000, Kingdom of Morocco
8Anesthesiologist-Intensivist, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco
9Cardiothoracic and Vascular Surgery, trainee resident in Cardiac Surgery, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco
10Chief of Anesthesiology-ICU-Emergency Department, Anesthesiologist-Intensivist, Professor of Anesthesiology-Intensive Medicine, Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco
*Corresponding author: Said Khallikane, Former anesthesiologist, Professor of Anesthesia-Intensive Medicine, Cardiothoracic Anesthesiologist Avicenna Military Hospital, Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech 40000, Kingdom of Morocco, Previous former anesthesiologist-intensivist, Hassan II Military Hospital, Layun 70000, Morocco, Anesthesiology-ICU-Emergency ex-former, Mohammed VI Hospital, Dakhla 73000, Morocco Faculty of Medicine and Pharmacy, Cadi Ayyad University, Marrakech, Morocco
Received Date: 12 November 2024
Accepted Date: 18 November 2024
Published Date: 19 November 2024
Citation: Khallikane S, Aissaoui Y, Belhadj A, Abdou A, Atmani N, et al (2024) Managing the Significant Challenge of Post-Cardiotomy Uncontrolled Hemorrhage: A Case Report and Literature Review. Ann Case Report. 9: 2076. https://doi.org/10.29011/2574-7754.102076
Abstract
The use of post-cardiotomy extracorporeal life support (PC-ECLS) is on the rise in adult cardiac surgery for the treatment of refractory cardiogenic shock and cardiac arrest. Despite technological advancements and increased use, the outcomes are inconsistent, and significant challenges and complications persist. This summary examines a case study of a 64-year-old woman with severe mitral regurgitation and heart failure that did not respond to medical treatment. She underwent mechanical mitral valve replacement and tricuspid annuloplasty. Although the surgery was successful, the patient had difficulty coming off cardiopulmonary bypass, requiring central extracorporeal membrane oxygenation (ECMO) support. She then experienced severe bleeding complications, consumptive coagulopathy, and died from multi-organ failure within 24 hours after surgery. A review of the literature emphasizes the increasing use of PC-ECLS in acute cardiocirculatory problems after cardiac surgery, including its indications, complications, and outcomes. It discusses criteria for selecting patients, predictors of mortality, and the need for a specialized team to identify candidates early and initiate support promptly to reduce negative outcomes. It also explores controversies in timing and management strategies, highlighting the importance of multidisciplinary care and comprehensive training to improve patient outcomes. Despite progress, challenges remain in predicting outcomes and managing complications associated with PC-ECLS. Further research is needed to refine patient selection criteria, improve predictive models, and enhance procedural techniques to optimize survival and quality of life for patients needing PC-ECLS in cardiac surgical settings.
Keywords: Cardiac Surgery; Post-Cardiotomy Extracorporeal Life Support (PC-ECLS); Cardiogenic Shock; Hemorrhage Post ECMO (Extracorporeal Membrane Oxygenation); Complications; Patient Selection; Mortality Predictor Factors.
Introduction
Unregulated bleeding following heart surgery, even with the best surgical intervention or implantation, is linked to higher mortality and overall health issues, including ischemic and infectious complications. Currently, there is no widely agreed-upon approach for the timing, most effective medical treatment, and prevention of uncontrolled hemorrhage after mitral and/or aortic valve reconstruction surgery complicated by infective endocarditis, or for promoting early detection and prompt decision-making about the need for implantation in preparation for emergency resternotomy, as well as the overall necessity for blood product transfusion. In modern intensive care settings, the likelihood of uncontrolled hemorrhage among patients with planned surgical corrections for serious valve issues and the risk of uncontrolled hemorrhage in patients who undergo extensive reconstructive surgery due to infective endocarditis share a common feature: psychological trauma for all patients who require postoperative emergency resternotomy and a high demand for blood products during resternotomy within the first 48 hours to 1 week following the procedure [1]. Postcardiotomy cardiogenic shock (PC-CS) is a major cause of mortality in cardiovascular surgery. Among patients with post-surgical PC syndrome, arterial blood loss from patients using an extracorporeal life support cannulation site is considered a dangerous complication, which, if combined with deep hypovolemia, raises the likelihood of hemorrhagic shock. Most patients who present with post-cardiopulmonary bypass or phlebotomy-related hemorrhage also need to re-establish CPB or phlebotomy through institutions using ECLS. Therefore, there is an intrinsic difficulty in the management of hemorrhage events occurring in patients supported by post-cardiotomy ECLS. This scenario is especially true in patients using a mechanical prosthetic valve, due to the need to monitor the international normalized ratio for both atrial fibrillation and anticoagulation related to the valve. In hemodynamically unstable patients at risk of developing hemorrhagic shock, the institution of heparin can be a difficult balance between stopping blood loss without increasing the risk of developing thromboembolic events. Here, with this case study, we present the dilemmas found in a clinical case where these circumstances collide [2].
Case Presentation
64-year-old female, with medical history of hypertension, hyperlipidemia, symptomatic mitral insufficiency presented initially with a history of repetitive episodes of acute cardiac insufficiency, worsening dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea. Despite optimization of medical therapy with sacubitril/valsartan, spironolactone, dapagliflozin, high-dose furosemide, bisoprolol, her symptoms continued to deteriorate. In her hospitalization in cardiology, the physical examination revealed signs of congestive heart failure, including elevated jugular venous pressure, bibasilar crackles, and a pansystolic murmur loudest at the apex radiating to the axilla. Transthoracic Echocardiography (TTE): Showed severe mitral regurgitation with a flail posterior leaflet, left ventricular dysfunction with an ejection fraction of 50%, tele-systolic diameter at 44mm, dilated left atrium and ventricle, and pulmonary hypertension with an estimated systolic pulmonary artery pressure of 60 mmHg. Transesophageal Echocardiography (TEE) has confirmed TTE findings and provided detailed assessment of the mitral valve pathology, including the mechanism and severity of regurgitation, as well as assessment of the tricuspid valve and right ventricular function. Given the severity of her symptoms and the progressive nature of her disease despite optimal medical therapy, she was scheduled for surgical intervention 3 months later after stabilization and complete decongestion with the addition of higher doses of furosemide. The plan involved mechanical mitral valve replacement given that mitral valve repair was deemed unfeasible based on the TEE data and the surgical team's experience and tricuspid annuloplasty to address the valvular pathology and alleviate symptoms of heart failure. The patient underwent cardiac surgery via median sternotomy with cardiopulmonary bypass. Mechanical mitral valve replacement (size 29) and tricuspid annuloplasty using a 32-mm semi-rigid annuloplasty ring were performed. TEE provided detailed intraoperative assessment of the mitral and tricuspid valves, confirming the severity of regurgitation (Figure 1) (video 1), mechanism of valvular dysfunction, and the need for surgical intervention. It also allowed for real-time monitoring of cardiac function and assessment of the adequacy of the surgical repair (Figure 2,3) showing a reduction in sub aortic velocity-time integrals (VTI), indicative of left ventricular dysfunction and pulmonary hypertension through the analysis of the pulmonary regurgitation velocity. With a cross-clamp time of 60 minutes and a cardiopulmonary bypass (CPB) duration of 120 minutes however, the weaning from cardiopulmonary bypass was complex, requiring central extracorporeal membrane oxygenation (ECMO) support. Progressive doses of inotropic support including epinephrine Corotrope, norephedrine, and inhaled nitric oxide were administered due to persistent hemodynamic instability with evident signs of pulmonary hypertension including a hypokinetic and dilated right ventricle, paradoxical septum, significant pulmonary regurgitation with elevated mean pulmonary artery pressure (MPAP), systolic pulmonary artery pressure (SPAP), and diastolic pulmonary artery pressure (DPAP), despite high doses of inotropes and pulmonary vasodilators. The left ventricular function was clearly impaired with a hypokinetic left ventricle, which dilated after a few minutes of complete cessation of cardiopulmonary bypass support. Due to the inability to wean off cardiopulmonary bypass (CPB), And after verification via intraoperative transesophageal echocardiography (TEE) of the proper functioning of the mechanical valve (video 2,3,4), central ECMO was implemented with arterial cannulation at the left ventricular apex and venous atrial cannulation, aiming for bridge to recovery and to prevent recurrent pulmonary edema episodes on peripheral ECMO, given the high filling pressures estimated by deceleration time and the E/Vp ratio and the falling ETT has shown an absence of holosystolic aortic valve opening under veno-arterial ECMO after failure to wean from cardiopulmonary bypass, indicating severe ventricular dysfunction and the non-contribution of the heart to the cardiac output generated by mechanical circulatory support associated to proper function of the Saint-Jude-Medical bileaflet valve with a low mean transvalvular gradient, indicative of postoperative left ventricular dysfunction. (Figure 4,5)Unfortunately, the patient developed significant bleeding, the advanced laboratory tests, which took time to arrive because we do not have localized laboratory devices to guide initial therapeutic strategies, a massive transfusion of platelets, fresh frozen plasma, packed red blood cells and fibrinogen concentrates has been performed, prothrombin complex concentrates were not available. Given the hemostatic disorders with laboratory evidence of hypofibrinogenemia and thrombocytopenia, suggestive of coagulopathy and consumptive coagulopathy secondary to surgical trauma and cardiopulmonary bypass, and the need for a reoperation was not taken, the ECMO pump flow continued to decline despite increasing, due to venous line collapse following a decrease in volume (video 5,6). Despite aggressive resuscitative efforts, she succumbed to complications and expired 24 hours after surgery.
Video 1: Pre-cardiopulmonary bypass (CPB) intraoperative TEE showing a significant preoperative transvalvular gradient related to grade 3-4 mitral regurgitation.

Figure 1: Intraoperative TEE performed before CPB, showing a significant mean transvalvular gradient, indicative of grade 3-4 mitral regurgitation.
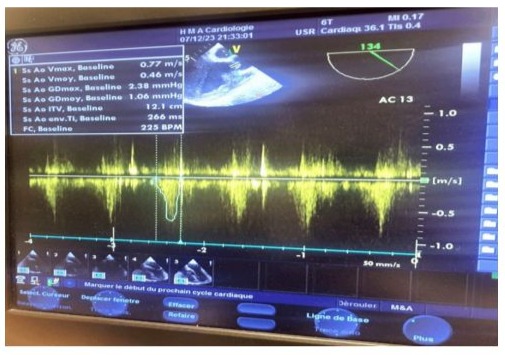
Figure 2: Pre-cardiopulmonary bypass (CPB) intraoperative TEE showing a reduction in subaortic velocity-time integrals (VTI), indicative of left ventricular dysfunction.
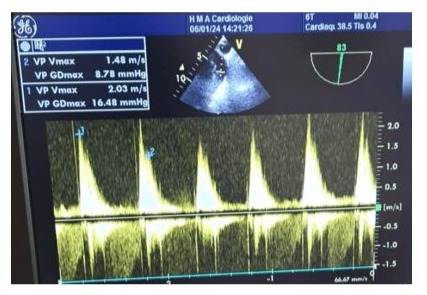
Figure 3: Pre-cardiopulmonary bypass (CPB) intraoperative TEE measurement of the protodiastolic and telediastolic gradients of pulmonary valve regurgitation by echocardiography.
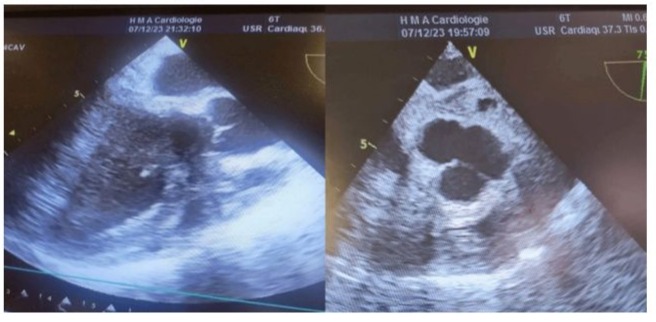
Figure 4: Midesophageal long-axis view at 120° (Left) and high esophageal view at 0° (Right) in TEE after native mitral valve replacement under PC-ECLS Showing an absence of holosystolic aortic valve opening under veno-arterial ECMO after failure to wean from cardiopulmonary bypass, indicating severe ventricular dysfunction and the non-contribution of the heart to the cardiac output generated by mechanical circulatory support.
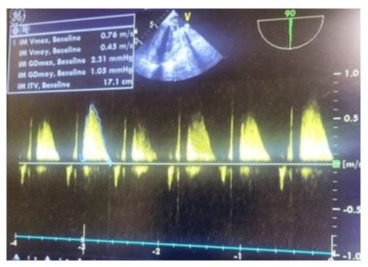
Figure 5: TEE after native mitral valve replacement with a mechanical valve, showing proper function of the Saint-Jude-Medical bileaflet valve with a low mean transvalvular gradient, indicative of postoperative left ventricular dysfunction.
Video 2: Postoperative TEE in a mid-esophageal view showing a functional St. Jude Medical bileaflet valve in the mitral position, with a minor washing jet leak.
Video 3: Postoperative TEE in a mid-esophageal view demonstrating the proper functionality of the bileaflet mechanical valve in the anti-anatomical mitral position, with good motion of both leaflets.
Video 4: Good motion of both leaflets of the Saint-Jude-Medical bileaflet valve seen in the postoperative trans-gastric view.
https://www.youtube.com/shorts/7my3nMZ3J1s?feature=share
Video 5: Mid-esophageal view on TEE showing severe postoperative biventricular hypokinesis with paradoxical septal motion and akinesia of the inferior and posterior walls of the left ventricle.
Video 6: Midesophageal long-axis view at 120° showing limited opening of the aortic valve occurring only in proto-systole, a during postoperative echocardiography under PC-ECMO, due to severe hypovolemia related to uncontrolled massive hemorrhage associated to the severe left ventricle dysfonction given an appearance of left ventricular outflow tract obstruction.
Discussion
The goals of this review are to address controversial areas and provide guidance on post-cardiotomy extracorporeal life support (PC-ECLS) in adult patients. Recent data show an increase in its use due to advancements in technology and reduced costs. However, worldwide survival rates have not improved and may be influenced by the complexity of patients rather than management quality. PC-ECLS remains important for temporary support and can save lives [1,2]. This case study aims to review the literature on PC-ECLS, including complications. Use of ECLS is rising for acute cardiocirculatory compromises that do not respond to conventional treatments. Additionally, it is quickly becoming an essential therapy for supporting patients experiencing acute cardiocirculatory compromise during, before, or after surgery. Delivery of cardiac surgery in the modern era is often complex, with significant morbidity and mortality. Difficulties commonly encountered in the early postoperative period include left ventricular failure, right ventricular failure, coagulopathy, low cardiac output, acidosis, and hypothermia. Cardiotomy extracorporeal cardiopulmonary life support is becoming an increasingly utilized salvage therapy strategy for refractory postcardiotomy cardiogenic shock in adults, with potential validity beyond bridge-to-decision and other short-term devices. The most important clinical predictor of hemorrhage is anticoagulant exposure and operative blood loss without cause disruption [3,4]. Mechanical heart valve implantation provides durable and effective anticoagulation therapy; however, there are rare but serious associated complications. Additionally, after post-cardiotomy bleeding or uncontrolled hemorrhage following a mechanical mitral valve implantation surgery, the problem of bridging these patients for recovery in the Intensive Care Unit with post-cardiotomy extracorporeal life support, a machine that replaces the function of the heart and lungs by taking over the work of circulating blood and adding oxygen to the blood before putting it back into the body for the patient to provide a chance for recovery, the correct anticoagulant and antiplatelet policy, blood products, and management in these particular subgroups of patients have yet to be defined and prove to be important and clinically challenging. Herein, we present a case of an uncontrolled hemorrhage in an adult patient with mitral valve replacement under extracorporeal life support. Every effort could help and would not deny the chance of recovery. Deaths and complications are often a result of multiple organ failure and perioperative complications. Among these, and particularly relevant for these patients, are those related to the administration of oxygenated suction blood diverted from the heart-lung machine for cardiopulmonary bypass with extracorporeal venous-arterial support [5,6]. Hemorrhage occurs in 2% of patients after cardiac surgery, and almost 20% of patients receive blood transfusions. The incidence of hemorrhage is increasing, and patients are being treated with anticoagulation, platelets, and coagulation agents. Patients who are unable to stabilize can be shifted to extracorporeal membrane oxygenation. A study reported that adults with a median age of 60 years received post-cardiotomy extracorporeal life support. At a median of 10.2 hours post-operatively, laboratory tests revealed that these patients required blood products and platelet products. Patients initiated on extracorporeal life support have a poor prognosis; however, early appropriate treatment and identification of adverse factors may improve prognosis [7,8]. post-cardiotomy extracorporeal life support (PC-ECLS) refers to extracorporeal life support initiated in the operating room following a ventricular or myocardial function failure post-cardiac surgery. PC-ECLS improves ventricular assisted systolic function and perfusion of organs, expedites recovery of cardiac functions, and increases oxygen transport. Surgical site bleeding after primary cardiac surgery for PC-ECLS had mortality rates of 20%. Although excessive drainage of anticoagulant, acquired Von Willebrand syndrome, and underestimated thrombocytopenia may contribute to severe bleeding complications, patients' unstable physical conditions may amplify the postoperative clinical impact. Several studies have reported the use of contemporary postoperative bleeding management in patients who receive ECLS for complications of mechanical circulatory support or endure uncontrolled postoperative bleeding complications after cardiac or non-cardiac vascular surgery. In the present study, we focused on an adult patient with a mechanical mitral valve replacement and tricuspid valve repair, who underwent PC-ECLS due to refractory cardiogenic shock following cardiotomy, with an inability to wean from cardiopulmonary bypass (CPB) and uncontrolled massive bleeding from the surgical site. Central extracorporeal support (PC-ECLS) was used to effectively manage the uncontrolled massive bleeding and provide hemodynamic support, which temporarily achieved hemodynamic stability despite massive transfusion, administration of platelets, fresh frozen plasma (FFP), and fibrinogen, based on laboratory results. The patient had a high level of fibrin/fibrinogen degenerative blood clotting, which was manifested by a high global blood clotting time. Since it was difficult to identify the cause of excessive destruction of fibrin/fibrinogen using the standard laboratory blood tests, we see the use of special tests for quantitative analysis of damage to fibrin/fibrinogen clots in severely bleeding cardiac patients undergoing heart surgery. This may facilitate the complex diagnosis of coagulopathy and should contribute to obtaining timely information on the etiology of impaired coagulopathy, thereby choosing the most appropriate algorithm for blood transfusion therapy and qualifying for the best surgical correction [9,10]. Early application of PC-ECLS may effectively manage the uncontrolled massive pericardial bleeding and maintain the hemodynamic status in adult patients with post-cardiotomy mechanical heart valve implantation and may provide adequate time to manage the surgical sites, coagulopathy, or debridement of surrounding hematoma with the threshold for reoperation. The decrease in the incidence of surgical site bleeding and improved rigidity of the trauma may enable early chest closure during the perioperative period [11,12]. Cardiac surgery often results in a significant increase in blood loss associated with insufficient preoperative hematological preparation, damage to multiple organ functions due to ischemia and hypoxemia during extracorporeal circulation, and postoperative factors. Therefore, the control of hemorrhagic diathesis and postoperative uncontrolled hemorrhage using various hemostatic techniques is one of the most acute and important problems in the practice of cardiac surgery. This problem is especially acute in patients with mechanical heart circulation support. Post-cardiotomy extracorporeal life support is a commonly used mechanical circulatory support device to sustain cardiac and pulmonary function in the perioperative period of high risk and complicated cardiac surgery. However, it may provoke multiorgan dysfunction, unfavourable outcomes, severe and recalcitrant hemorrhage, and a high level of adhesion and/or coagulopathy after DE cannulation. In addition, there is still no consensus on how to control anticoagulation after DE cannulation in patients with coagulopathy [13,14].
Conclusions
PC-ECLS represents an invaluable and irreplaceable tool in cardiac surgery settings. When treating patients with PC-ECLS, settings must be checked. The most important cause of bleeding in patients with PC-ECLS is the anticoagulation drugs that are given due to mechanical prosthesis in the heart. When a patient with a PC-ECLS unit is taken to the operating room, settings should be checked again. Therefore, emergency prophylactic anticoagulation must be planned. In this way, bleeding in the prosthetic valve and pump chambers can be avoided. Hypocalcemia must be avoided, hypofibrinogenemia must be prevented, and optimal pH and platelet count, which have a significant effect on coagulation function, should be maintained. The amount of heparin given to patients with PC-ECLS must be measured. Early detection of complications and implementation of effective interventions can improve patient prognosis. Different results are being introduced to the literature regarding the P1/2 ratio, heparin level, and anti-Xa level, and there are no standard levels associated with each Center. In major open-heart surgery and congenital cardiac surgery, the use of PC-ECLS is frequently increasing. Our purpose in the surgical and intensive care team should be to predict this at an early stage and have accurate knowledge of the PC-ECLS device settings to prevent complications and avoid any sequelae.
Conflicts of Interest Disclosure: The authors declare that they have no conflicts of interest.
Participants Consent: All participants have given their explicit consent for the publication of personal data concerning themselves and their colleagues as part of this study. They understand that this data may include information that could identify them in the context of the research findings. They have been informed about the purpose of this publication, the type of data that will be disclosed, and the potential implications. They acknowledge that this information will be publicly accessible after publication. They confirm that their consent is voluntary and that they have the right to withdraw it at any time prior to publication.
Authors Contributions: All authors contributed to the production of this article. They also declare that they have read and approved the final version of this manuscript.
References
- Malik A, Rehman FU, Shah KU, Naz SS, Qaisar S. (2021) Hemostatic strategies for uncontrolled bleeding: A comprehensive update. J Biomed Mater Res B Appl Biomater. 109:1465-1477.
- Rustenbach CJ, Djordjevic I, David L, Ivanov B, Gerfer S, et al (2022) Risk factors associated with in-hospital mortality for patients with ECLS due to postcardiotomy cardiogenic shock after isolated coronary surgery. Artif Organs. 46:1158-1164.
- Cho L, Kibbe MR, Bakaeen F, Aggarwal NR, Davis MB, Karmalou T, et al(2021) Cardiac Surgery in Women in the Current Era: What Are the Gaps in Care? Circulation. 144:1172-1185.
- Vervoort D, Swain JD, Pezzella AT, Kpodonu J. (2021) Cardiac Surgery in Low- and Middle-Income Countries: A State-of-the-Art Review. Ann Thorac Surg. 111:1394-1400.
- IJsselhof RJ, Slieker MG, Hazekamp MG, Accord R, van Wetten H, et al (2020). Mitral Valve Replacement With the 15-mm Mechanical Valve: A 20-Year Multicenter Experience. Ann Thorac Surg. 110:956-961.
- Kargoli F, Pagnesi M, Rahgozar K, Goldberg Y, Ho E, Chau M, et al (2021) Current Devices and Complications Related to Transcatheter Mitral Valve Replacement: The Bumpy Road to the Top. Front Cardiovasc Med. 8:639058.
- Tanner TG, Colvin MO. (2020) Pulmonary Complications of Cardiac Surgery. Lung. 198:889-896.
- Devereaux PJ, Szczeklik W. (2020) Myocardial injury after non-cardiac surgery: diagnosis and management. Eur Heart J. 41:3083-3091.
- Vilar R, Fish RJ, Casini A, Neerman-Arbez M. (2020) Fibrin(ogen) in human disease: both friend and foe. Haematologica. 105:284-296.
- Katayama, T, Yokoyama, N, Watanabe, Y, Koyama, S, Kawashima, H, et al (2024). Coagulation, fibrinolysis and platelet drop in patients undergoing transfemoral transcatheter aortic valve implantation. Catheterization and cardiovascular interventions: official journal of the Society for Cardiac Angiography & Interventions.
- Schaefer AK, Latus M, Riebandt J, Goliasch G, Bernardi MH, et al (2023) Bleeding and thrombotic events in post-cardiotomy extracorporeal life support. Eur J Cardiothorac Surg. 63: ezad072.
- Bonacchi M, Cabrucci F, Bugetti M, Dokollari A, Parise O, et al (2021) Outcomes' predictors in Post-Cardiac Surgery Extracorporeal Life Support. An observational prospective cohort study. Int J Surg. 82:56-63.
- Kowalewski M, Zieliński K, Brodie D, MacLaren G, Whitman G, et al (2021) Venoarterial Extracorporeal Membrane Oxygenation for Postcardiotomy Shock-Analysis of the Extracorporeal Life Support Organization Registry. Crit Care Med. 49:1107-1117.
- Bari G, Mariani S, van Bussel BCT, Ravaux J, Di Mauro M, et al (2024) Post-cardiotomy extracorporeal life support: A cohort of cannulation in the general ward. Artif Organs. 48:1355-1365.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.