Management and Treatment for Localized Pineal Germinoma in Adults: A Case Report
by Dahan D1*, Kupka D2, Curioni-Fontecedro A2, Gautron-Moura B2
1Department of Internal Medicine, Fribourg Hospital HFR, Switzerland
2Department of Internal Medicine, Division of Oncology, Fribourg Hospital HFR, Switzerland
*Corresponding author: Dahan D, Department of Internal Medicine, Fribourg Hospital HFR, Switzerland
Received Date: 30 January 2026
Accepted Date: 04 February 2026
Published Date: 06 February 2026
Citation: Dahan D, Kupka D, Curioni-Fontecedro A, Gautron-Moura (2026) Management and Treatment for Localized Pineal Germinoma in Adults: A Case Report. Ann Case Report. 11: 2522. DOI: https://doi.org/10.29011/2574-7754.102522
Abstract
Pineal gland germinomas are rare neoplasms that mainly affect children and adolescents. The standard treatment is chemotherapy followed by radiotherapy with whole brain irradiation (WVI) and boost to the tumor lesion. Proton therapy, with has some advantages and reduces the long-term side effects of radiation with high local control (PFS 95% and OS 100% at 28 months). This article describes a rare case of a localized pineal gland germinoma diagnosed in an adult treated with chemotherapy for 9 weeks followed by intracranial proton therapy (25 fractions) with a complete response.
Keywords: Intracerebral germinoma; Protontherapy; Case report
Background
Pineal germinomas are rare intracranial tumors. They represent the most common subtype of primary central nervous system (CNS) germ cell tumors (60%), with an incidence of approximately 1% in North America compared to 8-15% in Asia, suggesting a possible genetic predisposition that has not yet been identified. These tumors are diagnosed in adolescence, with a median age at diagnosis of 10-19 years, and are rare in adulthood, having a maleto-female ratio of 13-15:1. [1].
Standard treatment is chemotherapy followed by reduced-dose radiotherapy to the entire cerebroventricular system and tumor volume [2, 3]. Due to the location of the tumor and following radiation, the onset of long-term cognitive decline can occur. Proton therapy is now considered the safest form of radiotherapy, as it reduces the translation of the radiation beam and spares healthy brain tissue [4]. Here, we present the case of a young adult diagnosed with a localized pineal gland germinoma who was treated with chemotherapy followed by proton therapy.
Case Presentation
A 29-year-old Caucasian male presented with progressive onset of binocular diplopia and conjugate vertical gaze palsy. The patient consulted his primary care physician for these persistent neurological symptoms. His medical history was unremarkable, and clinical examination revealed no significant findings except for the presence of Parinaud’s syndrome and a class 3 obesity.
A brain MRI revealed a 15 x 10 x 12 mm mass in the pineal gland, exhibiting isointense signal characteristics on both T1 and T2 sequences, with intense enhancement and subtle heterogeneity following gadolinium injection. Radiological assessment of the spinal cord and conus medullaris was unremarkable, with no abnormal contrast enhancement. Lumbar puncture revealed no malignant cells, and the analysis of tumor markers (both in the serum and cerebrospinal fluid) showed a slight elevation in human chorionic gonadotropin (hCG), with normal alpha-fetoprotein (AFP) levels. Biopsy of the lesion confirmed the diagnosis of a pineal gland germinoma, demonstrating tumor markers consistent with germ cell origin (positive Mast/stem cell growth factor receptor (C-kit or CD117), weakly positive placental alkaline phosphatase (PLAP), partially positive beta human chorionic gonadotropin (β-HCG) and negative AFP).
The patient underwent curative chemotherapy according to the VIP protocol, administered every 3 weeks for 3 cycles. He tolerated the systemic treatment well, and a follow-up MRI of the brain at 1 month after completion of chemotherapy showed a partial response with a small area of residual contrast enhancement. Despite additional imaging sequences (phlebo-MRI and high-resolution 3DT2), this finding was suggestive of either a vascular structure or tumor rest. The patient then received ventricular radiotherapy (proton therapy) with sequential boost to the residual tumor.
Regarding radiotherapy, the patient received 24 Gy (15 fractions of 1.6 Gy/session) to the cerebral ventricles, followed by 40 Gy in sequential boost (10 fractions of 1.6 Gy/session) to the residual tumor tissue. Overall, the patient tolerated the proton therapy well, with no significant early or late toxicity from this treatment.
Initial screening for cardiovascular risk factors (previous to treatment with Cisplatin) revealed moderate hepatocellular injury (ASAT/ALAT ratio <1), prompting an abdominal ultrasound that identified fatty liver disease. Glycated hemoglobin was 5.9% and LDL-cholesterol was 2.65 mmol/L, leading to the implementation of dietary restrictions with a stable outcome over time. Follow-up ECGs during chemotherapy remained within normal limits, with no cardiac symptoms reported.
At the follow-up visit 6 months after radio-chemotherapy treatment, the patient reported mild and persistent visual disturbances, manifested by intermittent blurred vision after 6 to 7 hours of concentration, as well as persistent diplopia when gazing upward to the right and left. The patient underwent an ophthalmological examination, including optical coherence tomography (OCT) to assess the nerve fiber layer and ganglion cells in the retina, in order to evaluate the optic nerve and retina. The results were found to be at the lower limit of normal and this was interpreted as a possible sequel to the original tumor, and recovery is unlikely.
Post-therapy endocrinological evaluation of the pituitary axes revealed no significant changes, except for a mild elevation in prolactin levels, recorded at 18 µmol/L (normal range: 4-15 µmol/L), which was attributed to a physiological increase. The patient currently undergoes endocrinological follow-up.
Follow-up brain MRI at 3 and 6 months after end of treatment showed stability of a small area of contrast enhancement in the anterior pineal region, with no evidence of germinoma recurrence interpreted as a vascular lesion, and further complete response. Serum tumor markers, including HCG, were normal after chemotherapy as well as alpha-fetoprotein, which remained in normal limits. Following the European Reference Network for rare adult solid cancers (EURACAN) guidelines (2) and after multidisciplinary consultation, radiological surveillance will proceed with quarterly brain MRIs for the first year, followed by semiannual imaging if no recurrence is detected.
Discussion
We present a rare case of a localized germinoma of the pineal gland diagnosed in an adult with typical symptoms such as diplopia and conjugated /vertical gaze paralysis due to tumor compression of the tectal plate [2, 5]. Biologically, the tumor is non-secreting (normal levels of alpha-fetoprotein and slightly increased levels of hCG in blood and CSF) as in general [3, 5].
According to the literature, the choice of chemotherapy protocol in adults is not clearly defined due to the rarity of this pathological entity. Most of the publications found in adults are based on the SIOP protocol (4 cycles), which is developed for pediatric patients (Figure 1, 2). Upon multidisciplinary discussion, and in analogy to the testicular protocol, we have applied the VIP protocol (3 cycles) to this patient to minimize the possible side effects of systemic treatment (Table 1).
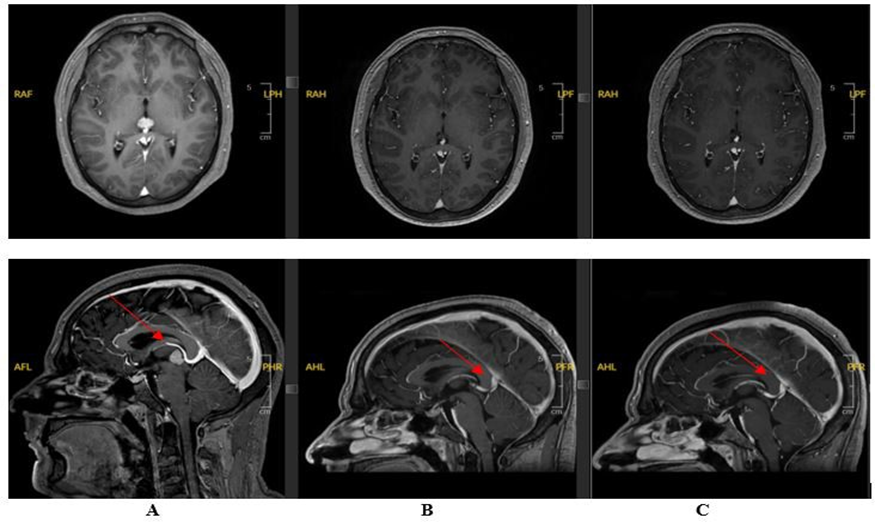
Figure 1: Cerebral MRI: A : At the time of diagnosis; B : 1 month after chemotherapy and before proton therapy and C: 3 months after proton therapy.
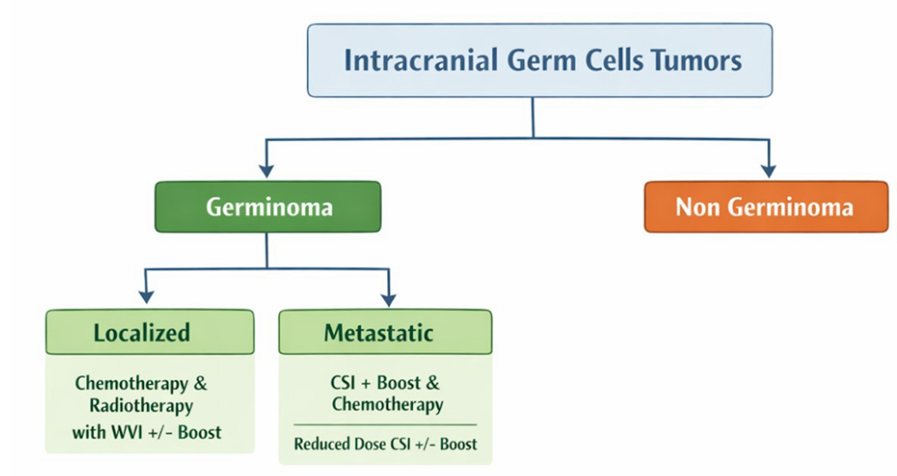
Figure 2: Current management of intracranial germinoma adapted from EANO, SNO and EURACAN consensus review. CSI – craniospinal irradiation and WVI – Whole-brain irradiation.
|
Criteria |
VIP Protocol |
SIOP Protocol |
|
Key chemotherapy |
Etoposide |
Etoposide |
|
Ifosfamide |
Ifosfamide |
|
|
Cisplatin |
Carboplatin |
|
|
Interval treatment |
Every 3 weeks |
Every 3 weeks (alternating carboplatinetoposide and ifosfamide-etoposide) |
|
Treatment Duration |
Variable, typically 3 to 4 cycles |
Variable, often 4 to 6 cycles depending on protocol |
Table 1: Comparison between the VIP and SIOP chemotherapy protocols for germinoma treatment.
The patient received 3 cycles of chemotherapy (cisplatin, etoposide and ifosfamide) followed by irradiation by spot-scanning proton therapy (PBS), with a total dose of 40Gy with a good radiological outcome.
Pineal gland germinomas have an excellent survival rate (>90%) without recurrence after treatment, even in patients with disseminated disease, according to the two E&NA studies. [3] They are highly sensitive to radiotherapy and chemotherapy, rendering surgical resection not indicated [5].
From 1950 to 1990, the standard of care was craniospinal irradiation alone with tumor bed boosting with excellent therapeutic responses (5-year event-free survival rate 97% in the SIOP CNS GCT 96 study). [3, 6].
Due to the substantial irradiation of surrounding healthy brain tissue associated with standard treatment protocols, patients often experience a range of long-term sequelae, including cognitive decline and the development of secondary malignant neoplasms over time. Additionally, patients treated with such protocols are 25 times more likely to experience a stroke by the age of 25 [3].
In order to mitigate radiation-induced damage, particularly to healthy brain structures, current treatment includes induction chemotherapy to reduce the tumor size, followed by reduced-dose cerebral and ventricular radiotherapy. Chemotherapy alone is not recommended as this might lead to an increased risk of disease recurrence up to 50% [3].
Because of its dosimetric advantages over other forms of radiation, combined with better preservation of surrounding healthy tissue, proton therapy is increasingly recommended as radiation modality in this scenario. (4)(3) Studies have shown excellent initial results with PFS of 95% and OS of 100% after 28-months of follow-up
[4].
Radiotherapy to the pineal gland may affect the hypothalamicpituitary axis, leading to potential endocrine dysfunction, including long-term hypopituitarism. Therefore, regular endocrine monitoring and close specialist follow-up during and after treatment are essential. (2) In our case, the patient did not experience any significant changes to the pituitary axes post-therapy.
Conclusion
Given the favorable prognosis and rarity of this disease, cases might be treated with different modalities, and this is especially true for the choice of systemic treatment in adults.
Clinical trials for this disease would be ideal, but due to the low incidence, case reports might be of help to share experiences with these cases. An international tumor registry is warranted to collect data and enable standardisation for management of this rare tumor entity, and particularly for adults.
List of Abbreviations
CNS – Central nervous system; CSI – Craniospinal irradiation; GCT – Germ cells tumors; IV – Intravenous; MRI – Magnetic resonance imaging; OS – Overall survivor; PFS – Progression free-survival; WVI – Whole-brain irradiation
PBT – Proton therapy; OCT – Optical coherence tomography; ECG – Electrocardiograms; PLAP – Placental alkaline phosphatase; HUG – Geneva University Hospital; β-HCG – Beta human chorionic gonadotropin; C-kit – Mast/stem cell growth factor receptor.
Declaration
Authors declare no conflicts of interest.
Consent for Publication Obtained from patient. Availability of Data and Materials
Data available upon request.
Competing Interests
None.
Funding
No external funding sources.
Authors’ Contribution
All authors contributed equally.
Acknowledgments
We thank our healthcare team for their support.
Authors’ Interests
No competing interests.
References
- Goodwin TL, Sainani K, Fisher PG. (2009). Incidence patterns of central nervous system germ cell tumors: A SEER study. J Pediatr Hematol Oncol. 31: 541-544.
- Lombardi G, Poliani PL, Manara R, Berhouma M, Minniti G, et al. (2022). Diagnosis and Treatment of Pineal Region Tumors in Adults: A EURACAN Overview. Cancers (Basel). 14: 1-21.
- Frappaz D, Dhall G, Murray MJ, Goldman S, Conter CF, et al. (2021). Management and Future Development of Intracranial Germ. 24: 1-12.
- Correia D, Terribilini D, Zepter S, Pica A, Bizzocchi N, et al. (2019). Whole-ventricular irradiation for intracranial germ cell tumors: Dosimetric comparison of pencil beam scanned protons, intensitymodulated radiotherapy and volumetric-modulated arc therapy. Clin Transl Radiat Oncol. 15: 53-61.
- Cohen D, Litofsky NS. (2023). Diagnosis and Management of Pineal Germinoma: From Eye to Brain. Eye Brain. 15: 45-61.
- Rogers SJ, Mosleh-Shirazi MA, Saran FH. (2005). Radiotherapy of localised intracranial germinoma: Time to sever historical ties? Lancet Oncol. 6: 509-519.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.