Lower Leg Muscle Hernia: A Systematic Review
by Si Heng Sharon Tan*, Brian Zhaojie Chin, Chintan Doshi, James Hoi
Po Hui, Andrew Kean Seng Lim
University Orthopaedics, Hand and Reconstructive Microsurgical Cluster, National University Health System, Singapore
*Corresponding author: Si Heng Sharon Tan, University Orthopaedics, Hand and Reconstructive Microsurgical Cluster, National University Health System, Singapore
Received Date: 09 October 2023
Accepted Date: 13 October 2023
Published Date: 16 October 2023
Citation: Tan SHS, Chin BZ, Doshi C, Hui JHP, Lim AKS (2023) Lower Leg Muscle Hernia: A Systematic Review. Ann Case Report. 8: 1477. https://doi.org/10.29011/2574-7754.101477
Abstract
Background: The review aims to review the published literature on lower leg muscle hernias.
Methods: A systematic review was conducted according to PRISMA guidelines. All studies that reported on lower leg muscle herniation were included.
Results: Lower leg muscle herniation occurs in predominantly males at an average age of 28.8 years (SD, 3.4 years). Most patients reported history of manual labour or sporting activities. The anterior compartment is predominantly affected (78.9%), followed by the lateral compartment (10.5%) and the superficial posterior compartment (10.5%). Tibialis anterior muscle herniation was predominantly found in younger patients (< 35 years old), as compared to older patients (>35 years old) who experienced herniation of varying muscles (e.g. soleus, peroneus, gastrocnemius). Fascial weakening at the point of muscle herniation was detected in 36.8% of included patients. Surgical management was performed in 78.9% of the patients, with the predominant surgery performed being fasciotomy, though recent reports also reported good outcomes with surgical repair in the presence of fascial defects in the lower limb without evidence of compartment syndrome. Resolution of symptoms (pain, muscle protuberance) and return to pre-herniation level of physical activities was reported in all studies.
Conclusions: Lower leg muscle herniation predominantly affects males in the third decade of life who are involved in manual labour or sporting activities. These predominantly affect the anterior compartment, with tibialis anterior being the predominant muscle involved in younger patients. Surgical management of both fasciotomy and surgical repair has led to good outcomes.
Keywords: Muscle Herniation; Exertional Compartment Syndrome; Surgical Repair; Fasciotomy
Introduction
Muscle hernias are abnormal protrusions of muscle through a fascial weakness or acquired fascial defect, with the lower leg being the most commonly involved extremity. Findings of lower limb muscle herniation typically involve the anterior compartment muscles, with the tibialis anterior muscle being the most commonly documented. Symptomatic lower leg muscle hernias, while rarely encountered in surgical practice, have previously been documented with varying presentations, chiefly soft tissue mass(es) and mass effects, pain, weakness, and chronic exertional compartment syndrome. Current literature is mixed on the modalities of imaging for diagnosis, where the choice of dynamic ultrasound versus magnetic resonance imaging (MRI) remains a debated topic. While most symptomatic presentations respond successfully to conservative treatment, recently published case reports on refractory lower leg muscle hernia highlight the need for surgery, with no consensus on the type of surgical technique (fasciotomy, anatomical repair, mesh repair). We performed a systematic review of published literature on lower leg muscle hernias to highlight patient demographics, presentations, diagnostic investigations, treatment methods, and functional outcomes. Additionally, we included a rare case of symptomatic bilateral, bicompartmental lower leg muscle hernia in a young male cross-country runner, managed in our institution with surgical repair into the cases available for systematic review
Material and Methods
A systematic review was performed according to PRISMA guidelines. Electronic searches were performed on PubMed, MedLine, and EMBASE to identify all relevant studies that reported on lower leg muscle herniation (Level I-IV). The following search terms (last performed on 30 September 2019) were combined using Boolean operators for PubMed: (muscle hernia OR muscular hernia) AND (leg OR lower limb) NOT (lumbar OR disc). Bibliographies of included studies and review articles identified were also hand-searched for additional eligible articles. Conference abstracts and unpublished data were considered to limit publication bias (only if sufficient results were available to conduct meaningful analyses). One patient with lower leg herniation that was treated in the authors’ institution was also included in the data analysis. Cadaveric studies, and studies describing muscle herniation in other anatomical regions, were excluded. This process was repeated twice independently. Each study’s data was then retrieved individually for patient demographics, injury characteristics, nerve involvement, investigations, management and functional or clinical outcomes.
Results
Case Report
A 14-year-old male cross-country runner presented with a 3-month history of bilateral lateral leg pain exclusively occurring during running activities, localised to 10cm above the lateral malleolus bilaterally. Concomitantly, he also noted localised swelling at the lateral aspect of the bilateral lower legs that corresponded to the area of the pain. The pain and swelling were noted to be similar since its onset, with no worsening prior to his presentation. The patient denied any associated weakness or numbness, preceding trauma or injuries, infective symptoms, and personal or family history of malignancies. Clinical examination revealed bilateral localised swellings. Two swellings were present over the right lower limb: Each located 10cm and 13cm above the lateral malleolus respectively, and were 2cm and 1cm in diameter respectively (Figure 1). A similar 1cm soft, hemispherical, nontender swelling was noted over the left lower limb, located 10cm above the lateral malleolus. All masses were noted to be soft, hemispherical, non-tender, attached to the underlying muscles, more prominent on ankle dorsiflexion, not attached to the overlying skin and subcutaneous tissue, and had no overlying skin changes. Examination of the bilateral lower limbs were otherwise normal. The clinical impression was therefore possible bilateral muscle herniation. Ultrasound of the lower limbs then revealed bilateral lower limb swellings consistent with muscle herniations. The patient was then managed with a trial of nonsurgical management, including activity modification and antiinflammatories. However, the patient returned in 3 months with persistence of pain symptoms despite conservative management and was therefore keen for surgical intervention. Subsequently, the patient underwent surgical repair of bilateral calf hernia defects. The surgery was performed under general anaesthesia with the patient in supine position. A longitudinal incision was made directly over the swellings. Careful subcutaneous dissection was performed to identify the herniated muscle. The herniated muscles were noted to involve both the anterior and lateral compartments bilaterally. On further exploration of the fascial defect, it was noted that the proximal herniation occurred at the point where the perforating vessels were traversing through the fascia (Figure 2A, 3A) while the distal herniation occurred at the point where the superficial peroneal nerves were exiting through the fascia bilaterally (Figure 2B, 3B). For the proximal herniation, the perforating vessels were ligated, and the muscle herniation was then reduced by closing the fascial defect over the herniated muscle. For the distal herniation, careful dissection was performed to release the exiting nerve and the muscle herniation was reduced by closing the fascial defect over the herniated muscle with 1-0 Prolene sutures, with sufficient portal for the nerve to exit the fascia without strangulation (Figure 4A, 4B). Irrigation and wound closure were then performed. Following the surgery, the patient was monitored post-operatively and discharged well on the same day. He was allowed full weightbearing but advised to start his athletic activities of running only 3 weeks after the surgery. The patient was then reviewed in clinic post-operatively at regular intervals. 10 weeks following the surgery, the patient reported to have returned to full athletic activities including running, with no more recurrence of pain or swelling. There were no intraoperative or post-operative complications noted during the follow-up visits. The patient was followed-up until 1 year post-operatively and was noted to be doing well. The patient as well as his legal guardians consented for his data to be submitted for publication.

Figure 1: Proximal and distal points of muscle swellings in the right lower leg with incisions marked by skin marker. A single mass similar in size and site to the distal muscle swelling on the right leg was found on the contralateral leg.
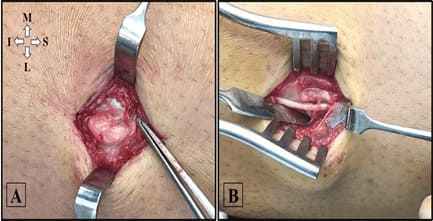
Figure 2: Intraoperative photos showing proximal anterior compartment muscle herniation (A) and distal lateral compartment herniation (B) in the left leg. M, Medial; L, Lateral; S, Superior; I, Inferior.
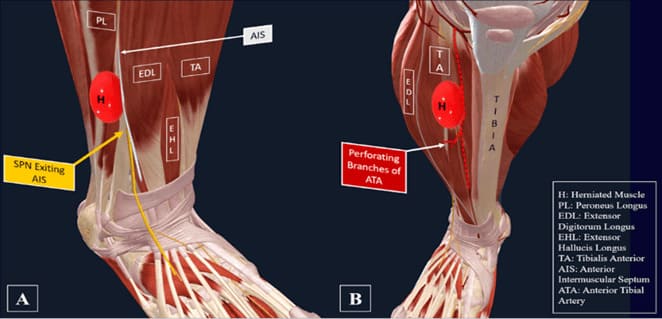
Figure 3: Virtual representation of bicompartmental swellings in the right lower leg. (A) Distal swelling where superficial peroneal nerve exits the anterior intermuscular septum; (B) Proximal swelling at the perforating branches of the anterior tibial artery.
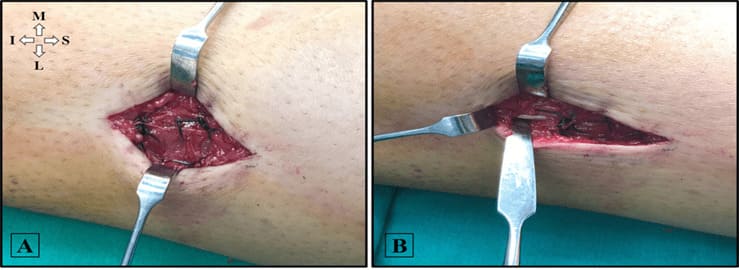
Figure 4: Intraoperative photos of direct fascial repair of proximal anterior compartment muscle herniation (A) and distal lateral compartment herniation (B) in the left leg with 1-0 Prolene sutures. M, Medial; L, Lateral; S, Superior; I, Inferior.
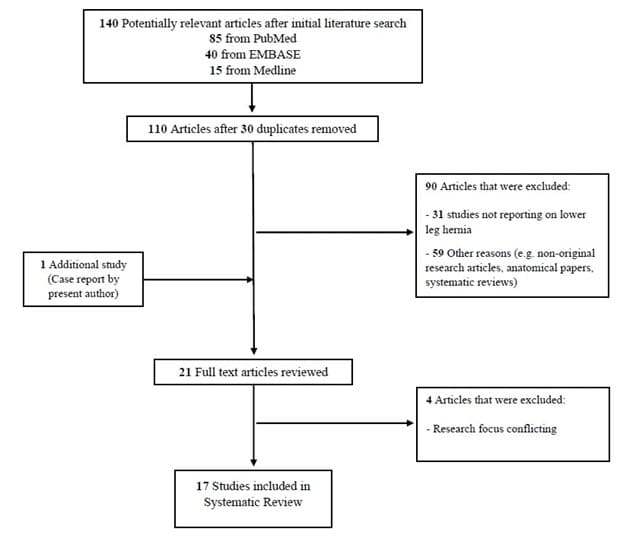
Figure 5: Flow diagram of the review and selection of cases.
Literature Selection
The search strategy identified 140 potentially relevant studies; titles were de-duplicated, and abstracts were screened. A further 5 studies were excluded for various reasons after review of 21 full-text articles (Figure 5). In all, a total of 17 primary references (including the present case report) comprising 56 patients with lower leg muscular hernia were included in this systematic review: 15 were case reports, 1 was a case series, and another was a pictorial essay. Baseline characteristics of included studies and study population are detailed in Table 1. Summary of investigations and treatment outcomes are detailed in Table 2.
|
Study |
Study Type |
Cases (n) |
Sex (M:F) |
Mean Age (yr) |
Side involved |
Muscle Involved |
Sporting Activities / Manual Labor |
Previous Trauma to Site |
Presenting Signs and Symptoms |
|||
|
L |
R |
Palpable Mass |
Exertional Pain |
Neurovascular Compromise |
||||||||
|
Artul 2014 |
CR |
1 |
0:1 |
19 |
0 |
1 |
TA |
Y |
N |
Y |
N |
NR |
|
Bates 2011 |
CR |
1 |
1:0 |
14 |
1 |
1 |
TA |
NR |
N |
Y |
N |
NR |
|
Beggs 2003 |
PE |
6 |
3:3 |
30.7 |
NR |
NR |
TA |
NR |
NR |
Y |
N |
NR |
|
Bergmann 2012 |
CR |
1 |
1:0 |
42 |
0 |
1 |
Gastrocnemius |
N |
Y |
Y |
Y |
N |
|
Cormier 2017 |
CR |
1 |
0:1 |
40 |
0 |
1 |
Soleus |
Y |
N |
N |
Y |
N |
|
Dyson 2019 |
CR |
1 |
1:0 |
26 |
1 |
1 |
NR |
Y |
N |
Y |
Y |
NR |
|
Fernando 2011 |
CR |
1 |
1:0 |
14 |
0 |
1 |
TA |
Y |
N |
Y |
N |
NR |
|
Finestone 2014 |
CS |
36 |
34:2 |
24 |
NR |
NR |
NR |
NR |
NR |
NR |
Y |
NR |
|
Gupta 2008 |
CR |
1 |
1:0 |
26 |
1 |
0 |
NR |
Y |
Y |
Y |
Y |
NR |
|
Henning 2009 |
CR |
1 |
1:0 |
56 |
0 |
1 |
EDL |
Y |
N |
Y |
Y |
N |
|
Naffaa 2016 |
CR |
1 |
1:0 |
16 |
1 |
0 |
SM |
Y |
Y |
Y |
Y |
N |
|
Khaladkar 2016 |
CR |
1 |
1:0 |
23 |
1 |
0 |
TA |
Y |
N |
Y |
N |
NR |
|
Nguyen 2013 |
CR |
1 |
1:0 |
62 |
1 |
0 |
Peroneus |
Y |
N |
Y |
Y |
NR |
|
Rho 2008 |
CR |
1 |
1;0 |
21 |
1 |
1 |
TA |
Y |
N |
Y |
Y |
NR |
|
Sharma 2017 |
CR |
1 |
1:0 |
28 |
1 |
0 |
TA |
N |
Y |
Y |
Y |
NR |
|
Tan 2019 |
CR |
1 |
1:0 |
14 |
1 |
1 |
See Case Report |
Y |
Y (L) |
Y |
Y |
N |
|
Ulu 2013 |
CR |
1 |
1:0 |
34 |
1 |
0 |
TA |
Y |
NR |
Y |
Y |
N |
|
CR, Case Report; PE, Pictorial Essay; CS, Case Series; TA, Tibialis Anterior; EDL, Extensor Digitorum Longus; SM, Semimembranosus; Y, Yes; N, No; NR, Not Reported |
||||||||||||
Table 1: Baseline Characteristics of Included Studies.
|
Study |
Investigation Modalities |
Defect Size (cm) |
Compartment Pressure (mm Hg) |
SPN Involvement |
Treatment Prescribed |
Treatment Outcomes |
Followup (Weeks) |
||
|
USG |
DYN USG |
MRI |
|||||||
|
Artul 2014 |
Y |
Y |
N |
1 |
NR |
N |
NR |
NR |
NR |
|
Bates 2011 |
Y |
Y |
N |
NR |
NR |
N |
NR |
NR |
NR |
|
Beggs 2003 |
Y |
Y |
N |
NR |
NR |
N |
NR |
NR |
NR |
|
Bergmann 2012 |
Y |
N |
Y |
3 x 7 |
Resting: 40 Exercise: 80 |
N |
Mesh Repair |
Resolution of Symptoms; Resumed preinjury level of physical activities |
6 |
|
Cormier 2017 |
Y |
Y |
Y |
1.6 x 1.4 |
NR |
N |
Conservative |
Resolution of Symptoms; Resumed preinjury level of physical activities |
NR |
|
Dyson 2019 |
Y |
N |
Y |
2 x 3 |
NR |
Y |
GraftJacket® Repair |
Resolution of Symptoms; Resumed preinjury level of physical activities |
14 |
|
Fernando 2011 |
Y |
Y |
N |
NR |
NR |
N |
Conservative |
NR |
NR |
|
Finestone 2014 |
NR |
NR |
NR |
NR |
Resting: 55 ± 21 Exercise: 86 ± 24 Recovery: 40 ± 27 |
Y (n = 3) |
Fasciotomy |
Superficial Peroneal Nerve Injury due to surgical complications (n = 3); Improvement in pain and activity level across all patients |
NR |
|
Gupta 2008 |
N |
N |
N |
NR |
NR |
N |
Fasciotomy |
Resolution of Symptoms; Resumed preinjury level of physical activities |
92 |
|
Henning 2009 |
Y |
Y |
Y |
0.6 x 0.5 |
NR |
N |
Fasciotomy |
Resolution of Symptoms; Resumed preinjury level of physical activities |
24 |
|
Naffaa 2016 |
Y |
Y |
Y |
2.5 |
NR |
N |
Conservative; Subsequent Fasciotomy |
Resolution of Symptoms; Resumed preinjury level of physical activities |
5 |
|
Khaladkar 2016 |
Y |
Y |
Y |
5.5 x 1.2 |
NR |
N |
Conservative |
NR |
NR |
|
Nguyen 2013 |
Y |
N |
Y |
2.5 x 2.0 |
NR |
Y |
Fasciotomy |
Mild exertional pain; Resumed preinjury level of physical activities |
52 |
|
Rho 2008 |
Y |
Y |
N |
NR |
NR |
N |
Conservative; Subsequent Fasciotomy |
NR |
NR |
|
Sharma 2017 |
Y |
Y |
N |
9.5 |
NR |
N |
NR |
NR |
NR |
|
Tan 2019 |
Y |
Y |
N |
2 x 1 |
NR |
Y |
Conservative; Subsequent Direct Repair |
Resolution of Symptoms; Resumed preinjury level of physical activities |
16 |
|
Ulu 2013 |
Y |
Y |
Y |
NR |
NR |
N |
Conservative |
Resolution of Symptoms; Resumed preinjury level of physical activities |
32 |
|
SPN, Superficial Peroneal Nerve; Y, Yes; N, No; NR, Not Reported |
|||||||||
Table 2: Pooled Results.
Patient Demographics
The present systematic review on 17 included studies as well as the additional case report comprised 57 lower leg muscle herniation patients, which were found to be predominantly male (87.7%). The weighted average age of presentation was at 28.8 years of age (SD, 3.4 years; 95% CI, 21.5 to 36.1 years). 11 out of 17 studies reported patients with history of manual labour or engagement in sporting activities [1-10]. 3.5% (n = 2) of the total study population were military service members [8,9]. 12.3% (n = 7) of included patients were noted to be athletes [1-3,5-7], of whom 42.9% (n = 3) were endurance athletes or long-distance runners [3,6], 14.3% (n = 1) were competitive at a collegiate level [7], and another 14.3% (n = 1) were competitive at professional level [5]. The average follow-up was 30.1 weeks (SD, 10.36 weeks; 95% CI, 5.61 to 54.64 weeks).
Injury Characteristics
Bilateral lower leg muscle herniation was reported in 7% of patients (n = 3) in 4 studies [4,9,11], including the present case report. Of note, no specific predictive factors for bilateral involvement were found on qualitative analysis. Compartment involvement was noted in 14 studies (19 patients) [1-3,6-15], consisting of predominantly anterior compartment muscle herniation (78.9%) [1,2,6,9-12,14,15], followed by lateral compartment (10.5%)8 and superficial posterior compartment (10.5%) [3,13]. The present case report is the only study which involves bi-compartmental muscle herniation in the lower leg. Herniation of the tibialis anterior muscle was predominantly found in younger patients (< 35 years old) [1,2,9-12,14,15], as compared to older patients (>35 years old) who experienced herniation of varying muscles (e.g. soleus, peroneus, gastrocnemius) [3,6,8,13].
Nerve Involvement
Superficial peroneal nerve involvement was rare, and diagnosed either sonographically or intraoperatively in only 10.5% of patients across 4 studies, including the present case report [4,8,16]. Fascial weakening at the point of muscle herniation was detected in 36.8% of included patients, either through radiological means or surgical exploration [1-15]. One study primarily focused on results of surgery and clinical management flowchart without reporting evidence of fascial weakening [16].
Investigations
16 studies comprising 21 patients reported usage of imaging for diagnosis of muscle hernia [1-15], of which ultrasound and dynamic ultrasound were used in 100% (n = 21) and 80.1% (n = 17) of patients respectively to confirm diagnosis of muscle hernia. 8 studies comprising 8 patients (38.1%) utilized MRI for diagnosis due to inconclusive findings from ultrasonography [3,4,6-8,10,13,14]. 2 studies comprising 37 patients measured compartment pressures [13,16], with Bergmann et al. measuring resting and exercise compartmental pressures, and Finestone et al. measuring mean resting, exercise, and recovery compartmental pressures. Of note, 5 studies [5-9] which performed fasciotomies did not measure compartment pressures.
Management and Clinical/Functional Outcomes
Conservative management of muscle hernia was adopted in 5 case reports [1,3,7,9,10], with the primary methods of conservative management including rest from strenuous exercise, icing of affected site, prescription of compression garments, oral analgesics, and physical therapy. Similar to the present case report, 2 studies reported failure of conservative management which presented in the form of pain recurrence and/or repeated mass protuberance, requiring conversion to surgery [7,9]. In total, 9 studies comprising 45 patients (78.9%) involved surgical management of lower leg muscle herniation, chief of which 11 patients from 6 studies were treated with fasciotomies [5-9,16], 1 patient had a mesh repair [13], another had fascial graft repair [4], and the present study performed a direct repair. While 4 studies highlight evidence of compartment syndrome warranting fasciotomy [5,6,8,16], the case reports by Naffaa et al and Rho et al mentioned failure of conservative management as the chief reason for fasciotomy. Across all studies, resolution of symptoms (pain, muscle protuberance) and return to pre-herniation level of physical activities were reported regardless of conservative or surgical management. Of particular interest, 2 studies that share similarities with the present case report involved presence of fascial defects in the lower limb without evidence of compartment syndrome, and were repaired using GraftJacket and mesh due to the size of fascial defect [4,13]. Like our case report, the patients eventually had complete resolution of symptoms and return to pre-herniation level of physical activities.
Discussion
There are several principal findings of the current review. Firstly, lower leg muscle herniation has been found to occur in predominantly males at an average age of 28.8 years (SD, 3.4 years). Secondly, most patients reported history of manual labour or sporting activities. Thirdly, the anterior compartment is predominantly affected (78.9%), followed by the lateral compartment (10.5%) and the superficial posterior compartment (10.5%). Tibialis anterior muscle herniation was predominantly found in younger patients (< 35 years old), as compared to older patients (>35 years old) who experienced herniation of varying muscles (e.g. soleus, peroneus, gastrocnemius). Fourthly, fascial weakening at the point of muscle herniation was detected in 36.8% of included patients. Lastly, surgical management was performed in 78.9% of the patients, with the predominant surgery performed being fasciotomy, though recent reports also reported good outcomes with surgical repair in the presence of fascial defects in the lower limb without evidence of compartment syndrome. Resolution of symptoms (pain, muscle protuberance) and return to pre-herniation level of physical activities was reported in all studies. Amongst these, there are several findings that are novel to the study. Firstly, the study identified that the anterior compartment is predominantly affected (78.9%) in lower leg muscle herniation, followed by the lateral compartment (10.5%) and the superficial posterior compartment (10.5%). Secondly, the study identified that herniation of the tibialis anterior muscle was predominantly found in younger patients (< 35 years old), as compared to older patients (>35 years old) who experienced herniation of varying muscles (e.g. soleus, peroneus, gastrocnemius). Lastly and most importantly, the study identified that surgical repair of the lower leg muscle herniation in the presence of fascial defects in the lower limb without evidence of compartment syndrome, instead of fasciotomy, can lead to good outcomes. Indeed, while nonsymptomatic muscle hernias are often managed conservatively, prompt surgical referral is warranted for those with persistence or worsening of symptoms despite initial trial of conservative management [4,15,17]. Various surgical techniques for treatment of lower leg muscles have been stated in literature, including direct fascial repair [18-20], decompressive fasciotomy [5,21,22], and use of synthetic mesh [19,23]. This comprehensive, upto-date literature review reflects no consensus to any specific treatment methods. Thus, treatment should be tailored specifically to individual, and take into consideration the severity of signs/ symptoms, location of herniation, size of defect, presence of fascial weakening and patient-centered factors (cosmesis, sport performances etc). Longitudinal fasciotomy has been lauded to be the commonest and safest surgical option for treatment of symptomatic muscle hernias of the leg [8,23,24]. However, its disadvantages can be easily overlooked. Fasciotomy enlarges the defect and eliminates risk of compartment syndrome, at the cost of potential neuromuscular damage8, formation of muscle adhesions [25], re-presentation of muscle hernia, and residual symptoms (common amongst runners) [24]. A study by Kramer et al. reported patients may have the worst clinical outcomes post-fasciotomy, such as incomplete pain resolution affecting performance [24]. Moreover, few studies in literature examine compartment pressures prior to performing fasciotomy on athletes with lower leg muscle hernia, further questioning if their technique is tailored to the individual, or simply adopting a fail-safe approach despite other viable surgical options which may offer the patient (often young and actively engaging in sporting activities) better performance. The current review examined the different surgical techniques for the management of muscle herniation and identified that resolution of symptoms (pain, muscle protuberance) and return to pre-herniation level of physical activities was reported in all studies. These positive outcomes following surgical repair of the fascial defects for muscle herniation in the current case as well as the two other reports are encouraging [4,13]. The good outcomes following the novel surgical management then suggest that surgical repair, instead of fasciotomy, could be used for fascial defects in the lower limb without evidence of compartment syndrome. Despite so, this systematic review faces its limitations. Most importantly, the small number of publications and sample size available limits the power of the conclusions drawn from the review. This is because there exist a limited number of publications in the available literature regarding muscle herniation. Fourteen out of sixteen of the studies included are also individual case reports. When subdivided into the different components for analysis, such as that of patient characteristics, injury characteristics, nerve involvement, investigations or management, each component then comprises even fewer number of patients that precludes robust analysis. The topic will therefore definitely benefit from further larger scale studies, to help guide the management of these patients better.
Conclusions
Lower leg muscle herniation predominantly affects males in the third decade of life who are involved in manual labour or sporting activities. These predominantly affect the anterior compartment, with tibialis anterior being the predominant muscle involved in younger patients. Surgical management of both fasciotomy and surgical repair has led to good outcomes.
Declarations
Ethical approval and consent to participate: No ethical approval is required for the study.
Consent for publication: Informed consent was obtained from the patient whose case was presented in the review.
Availability of data and materials: All data generated or analysed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Funding: No funding was received for the study.
Author’s contribution: TSH conceptualised the study, collected data, analysed data and drafted the manuscript. CBZ collected data, analysed data and drafted the manuscript. DC conceptualised the study and collected data. HJH conceptualised the study. Lim AKS conceptualised the study. All authors read and approved the final manuscript.
Acknowledgements: Not applicable.
References
- Alfageme F, Morales V, Garcia C, Miguelez AP, Dominguez E, et al (2011) Transfascial muscular hernia: an unusual cause for a “hide and seek” subcutaneous nodule. Dermatology online journal 17:4.
- Artul S, Habib G. (2014) The importance of dynamic ultrasound in the diagnosis of tibialis anterior muscle herniation. Critical ultrasound journal 6:14.
- Cormier DJ, Gellhorn AC, Singh JR. (2017) Soleus Muscle Herniation With Magnetic Resonance Imaging and Ultrasound Correlation in a Female Long-Distance Runner: A Case Report. PM & R : the journal of injury, function, and rehabilitation 9:529-32.
- Dyson K, Palan J, Mangwani J. (2019) Bilateral non-traumatic lower leg fascial defects causing peroneal muscle herniation and novel use of a GraftJacket to repair the fascial defect. Journal of clinical orthopaedics and trauma 10:879-83.
- Gupta RK, Singh D, Kansay R, Singh H. (2008) Cricket ball injury: a cause of symptomatic muscle hernia of the leg. British journal of sports medicine 42:1002-3.
- Henning PT, Dahm DL, Smith J. (2009) Use of postexercise ultrasonography to identify a symptomatic extensor digitorum longus muscle hernia associated with running. PM & R : the journal of injury, function, and rehabilitation 2009;1:1109-11.
- Naffaa L, Moukaddam H, Samim M, Lemieux A, Smitaman E. (2017) Semimembranosus muscle herniation: a rare case with emphasis on muscle biomechanics. Skeletal radiology 46:373-8.
- Nguyen JT, Nguyen JL, Wheatley MJ, Nguyen TA. (2013) Muscle hernias of the leg: A case report and comprehensive review of the literature. The Canadian journal of plastic surgery = Journal canadien de chirurgie plastique 21:243-7.
- Rho NK, Kim WS, Kim YJ, Yoo KH, Kim BJ, et al (2008) The Use of Dynamic Ultrasonography for the Confirmation of Lower Leg Muscle Herniation. Ann Dermatol 20:190-2.
- Ulu MA, Cakmak M, Nas K. (2013) A case of tibialis anterior muscle herniation diagnosed by ultrasonography. Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi 59:73-5.
- Bates DG. (2001) Dynamic ultrasound findings of bilateral anterior tibialis muscle herniation in a pediatric patient. Pediatric radiology 31:753-5.
- Beggs I. (2003) Sonography of Muscle Hernias. American Journal of Roentgenology 180:395-9.
- Bergmann G, Ciritsis BD, Wanner GA, Simmen HP, Werner CML, et al (2012) Gastrocnemius muscle herniation as a rare differential diagnosis of ankle sprain: Case report and review of the literature. Patient safety in surgery 2012: 6 (no pagination).
- Khaladkar SM, Kondapavuluri SK, Kamal A, Kalra R, Kamal V. (2016) Detection of Myofascial Herniation on Dynamic Sonography and Magnetic Resonance Imaging. Case reports in radiology 2016:4245189.
- Sharma N, Kumar N, Verma R, Jhobta A (2017) Tibialis Anterior Muscle Hernia: A Case of Chronic, Dull Pain and Swelling in Leg Diagnosed by Dynamic Ultrasonography. Polish journal of radiology 82:293-5.
- Finestone AS, Noff M, Nassar Y, Moshe S, Agar G, et al (2014) Management of chronic exertional compartment syndrome and fascial hernias in the anterior lower leg with the forefoot rise test and limited fasciotomy. Foot & ankle international 35:285-92.
- Fouasson-Chailloux A, Menu P, Allorent J, Dauty M (2018) Determination of the predictive clinical parameters to diagnose chronic exertional compartment syndrome. European journal of sport science 18:279-85.
- Alhadeff J, Lee CK. (1995) Gastrocnemius muscle herniation at the knee causing peroneal nerve compression resembling sciatica. Spine 20:612-4.
- Lee HS, James M. (2006) Painful bilateral herniation of the anterior tibial muscle: a case report. Foot & ankle international 27:552-5.
- Angadi DS, Rampaul RS, Akthar I, Makdhoomi K. (2007) Bilateral muscle hernias of the anterior tibial muscle. Foot & ankle international 28:520.
- Berglund HT, Stocks GW. (1993) Muscle hernia in a recreational athlete. Orthopaedic review 22:1246-8.
- Dawar A, Dawar R, Gawri K, Gupta VJJoCR. (2012) Tibialis anterior muscle hernia: a rare cause of leg pain. 2:42-4.
- Bergmann G, Ciritsis BD, Wanner GA, Simmen HP, Werner CM, et al (2012) Gastrocnemius muscle herniation as a rare differential diagnosis of ankle sprain: case report and review of the literature. Patient safety in surgery 6:5.
- Kramer DE, Pace JL, Jarrett DY, Zurakowski D, Kocher MS, Micheli LJ. (2013) Diagnosis and management of symptomatic muscle herniation of the extremities: a retrospective review. The American journal of sports medicine 41:2174-80.
- Lewis J, Shaw A, Arrowsmith J, Stephen AJIE. (2008) The symptomatic tibialis anterior hernia: Case report and a new rationale for treatment. 1:4-6.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.