Liver Abscess : Management in the General Surgery Department of the Ziguinchor Regional Hospital, About 36 Cases
by Mohamed Doukoure1,4*, Mohamed Dieng1, Fatoumata Binta Diallo2, Cheikh Ahmed Badji3, Ismael Racine Bayo4, Souleymane Mangane3, Mamadou Ndiaye3,5, Abdourahmane Ndong4, Oumar Sow3,5, Cheikh Diouf1,5, Ibrahima Konate4
1Department of Surgery, Hospital Regional from Ziguinchor, Senegal
2Imaging Department, Hospital Regionalfrom Ziguinchor, Senegal
3Department of Surgery, Hospital of Peace from Ziguinchor, Senegal
4Department of Surgery, Gaston Berger University of Saint-Louis (UGB), Senegal
5Department of Surgery, Assane Seck University of Ziguinchor, Senegal
*Corresponding Author: Mohamed Doukouré, Department of Surgery, Gaston Berger University of Saint-Louis (UGB), Senegal
Received Date: 10 December 2025
Accepted Date: 16 December 2025
Published Date: 18 December 2025
Citation: Doukoure M, Dieng M, Diallo FB, et al. (2025) Liver Abscess : Management in the General Surgery Department of the Ziguinchor Regional Hospital, About 36 Cases. J Surg 10:11514 https://doi.org/10.29011/2575-9760.011514
Summary
Introduction: The aim of this study was to evaluate the management of liver abscesses in our department. Methodology: we conducted a retrospective, cross-sectional, descriptive study over 18 months, including patients over 15 years of age.
Results: We recorded 36 cases of liver abscess. The average age was 44.7 years, with a ratio of 2.3. Alcohol consumption was noted in 30.6% (n:11). Common signs included abdominal pain, either 47.2% (n:17) and hepatomegaly in 61.1%(n:22). The average kinetics of white blood cells was 33431.6 elements/mm3 and 97.73mg/l for CRP. The abdominal ultrasound was performed at 61.1% (n:22) and lan abdominal CT scan in 58.3% (n:21). In total, the right lobe of the liver was affected in 61.1% (n:22). Amoebic serology was positive in one patient, and cytobacteriological examination isolated a pathogen in three patients (E. coli, S. epidermidis, K. pneumoniae). Dual antibiotic therapy combined metronidazole. The drainage was ultrasound-guided in 69.4% (n: 25) and surgery was performed in a total of 30.5% (n:11) cases. The average length of hospital stay was 7.8 days. Patient progress has three months was favorable in 80.6% (n:29).
Conclusion: Liver abscesses are common in our practice. They affected adults. Fontan’s triad was frequently observed. Antibiotic therapy combined with drainage was the mainstay of treatment.
Keywords: Abscess; Drainage; Liver; Ziguinchor
Introduction
Liver abscess is a relatively rare condition; age and underlying health conditions (immunodeficiency) may increase the risk [1]. They are generally of parasitic or bacterial origin and exceptionally fungal [2]. In the West, bacterial liver abscesses are the most common, with a mortality rate close to 15%; in Africa, amoebic infection remains frequent [3]. Morphological and microbiological data establish the diagnosis [4]. Treatment relies on antibiotic therapy, ultrasound-guided drainage, and surgery in some cases [5].
Methodology
We conducted a retrospective (12 months), cross-sectional (6 months), and descriptive study over 18 months (January 1, 2024, to June 30, 2025). The study included patients over 15 years of age who were hospitalized and treated for liver abscesses in the general surgery department of the Ziguinchor Regional Hospital. Data were collected after obtaining the patients’ free and informed consent. The parameters studied were : epidemiological (age and sex); risk factors (chronic alcohol consumption, tobacco use, hepatitis B, HIV, diabetes, gallstones); clinical (abdominal pain, fever, hepatomegaly, WHO activity index); paraclinical (Complete Blood Count, CRP, AST/ALT, abdominal ultrasound and CT scan); therapeutic approaches (antibiotic therapy, drainage, and surgery); and outcome (favorable, recurrence, death). Data were collected from medical records. Descriptive analyses were performed, including calculations of frequencies, means and standard deviations, and the median (Q1-Q3).
Results
We recorded 36 cases of liver abscess; the 25-45 age group was the most represented 55.6% (n:20), with aaverage of 44.7years [2575 years] and a male predominance of 69.4% (n:25), ora ratio of 2.3. Chronic alcohol consumption was noted in 30.6% (n:11) of patients, two cases of HIV infection were observed (Figure 1).
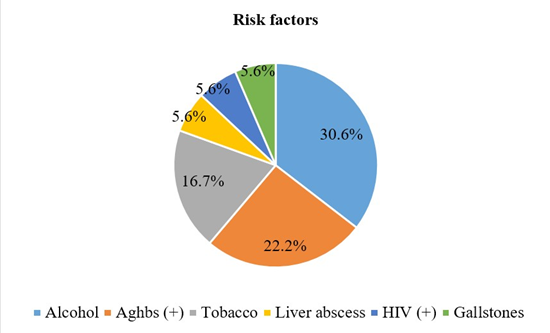
Figure 1: Distribution of Patients According to Risk Factors
The most frequent clinical signs in patients were : abdominal pain or 47.2% (n:17), fever in 38.9% (n:14) and hepatomegaly in 61.1% (n:22). In biology, the average kinetics of white blood cells (elements/mm3) was 33431.6 [1200-91000] on admission versus 9179.7 [4000-21000] after 3 days and for CRP (mg/l) measured under the same conditions, it went from 97.73 versus 79.11 (Table 1).
|
Biological
data |
Effective |
Proportion
(%) |
|
Gwhite
lobules upon admission |
Maverage:
33431.6±151732.9 [1200-91000] |
|
|
Hyperleucytosis |
21 |
58.3 |
|
Leucopenia |
12 |
33.3 |
|
normal |
3 |
8.3 |
|
Gwhite
lobules at 72H |
Average:
9179.7±3786.5 [4000-21000] |
|
|
Hyperleucytosis |
18 |
50 |
|
Leucopenia |
15 |
41.7 |
|
normal |
3 |
8.3 |
|
CRPupon
admission |
Average:
97.73±82.4 |
|
|
Raised |
19 |
52.8 |
|
Normal |
3 |
8.3 |
|
CRP at
72H |
Average:
79.11±75 |
|
|
Raised |
16 |
44.4 |
|
Normal |
2 |
5.6 |
|
Hemoglobin
levels |
||
|
Normal |
35 |
97.2 |
|
Anemia |
1 |
2.8 |
|
ASAT |
||
|
Raised |
15 |
41.7 |
|
Normal |
10 |
27.8 |
|
ALAT |
||
|
Normal |
12 |
33.3 |
|
Raised |
11 |
30.6 |
Table 1: Distribution of Patients According to Biological Data
The abdominal ultrasound was performed at 61.1% (n: 22) of patients, showing unisegmental involvement in 33.3% (n: 12) cases and an average volume of 268.5 ml. The abdominal CT scan was performed in 58.3% (n:21), showing unisegmental or bisegmental involvement inequal proportions of 22.2% (n:8) and an average size of 10 cm (Table 2). Individually considered, segment VII was the most affected that is 19.4%, at CT scan (Figure 2). The abscess was located solely in the right lobe of the liver 44.4% (n:16) (Table 3). Amoebic serology was positive in one patient, while routine cytobacteriological examination isolated pathogens in only three patients (E. coli, S. epidermidis, K. pneumoniae). Antibiotic therapy was administered to all patients, combining metronidazole to ceftriaxone in 63.9% (n:32) or to amoxicillin clavulanic acid in 36.1% (n: 13). The antibiogram showed sensitivity to these molecules in all three cases. Drainage was ultrasound-guided in 69.4% (25) and surgery was performed in a total of 30.5% (n :11) cases (Table 4). The mean volume of pus drained was 704.4 ml [60-3200 ml], and the mean drainage duration was 4.8 days [2-14 days]. A follow-up ultrasound was routinely performed before drain removal. The mean length of hospital stay was 7.8 days [3-17 days]. After one-month and three-month follow-up, the clinical, biological, and ultrasound outcomes were favorable in 80.6% of patients (n = 29), and abscess persistence was observed in the two HIV-positive patients (Table 5).
|
Morphological data |
Effective |
Proportion (%) |
|
|
Abdominal ultrasound |
22 |
61.1 |
|
|
Number of segments
reached |
1 |
12 |
33.3 |
|
2 |
7 |
19.4 |
|
|
3 |
3 |
8.3 |
|
|
Volume (ml) |
> 50 |
18 |
50 |
|
< 50 |
3 |
8.3 |
|
|
Average: 268.5± 220.9
[29-1011] |
|||
|
Abdominal CT scan |
21 |
58.3 |
|
|
Number of segments
reached |
1 |
8 |
22.2 |
|
2 |
8 |
22.2 |
|
|
3 |
4 |
11.1 |
|
|
Size (cm)
|
> 10 |
3 |
8.3 |
|
05-Oct |
2 |
5.6 |
|
|
< 5 |
1 |
2.8 |
|
|
Average 10± 5[4-19] |
|||
Table 2: Distribution of Patients According to Morphological Data

Figure 2: Distribution of Patients According to Segmental Involvement on Abdominal CT Scan
|
Diagnostic/Topographic |
Effective |
Proportion (%) |
|
Right liver |
16 |
44.4 |
|
Left liver |
7 |
19.4 |
|
Right liver + Left liver |
6 |
16.7 |
|
PAG/rupture |
4 |
11.1 |
|
Pre-suppurative |
2 |
5.6 |
|
No |
1 |
2.8 |
|
Total |
36 |
100 |
Table 3: Distribution of Patients According to Thetopographic Diagnosis
|
Indication |
Effective |
Proportion (%) |
|
|
Ultrasound-guided dr |
ainage |
25 |
69.4 |
|
Surgery/drainage f |
ailure |
7 |
19.4 |
|
Ultrasound-guided p |
uncture |
4 |
11.1 |
|
primary surgery |
4 |
11.1 |
|
|
Scan-guided drain |
age |
1 |
2.8 |
|
Associated gestures |
Toilet + drainage |
3 |
8.3 |
|
Ileostomy |
1 |
2.8 |
|
Table 4: Distribution of Patients According to the indications
|
Post-operative care |
Effective |
Proportion (%) |
|
Immediate |
||
|
Favorable |
29 |
80.6 |
|
Lost sight of |
7 |
19.4 |
|
1 month |
||
|
Favorable |
31 |
86.1 |
|
Persistent abscess |
2 |
5.6 |
|
Lost sight of |
2 |
5.6 |
|
Restoring continuity |
1 |
2.8 |
|
3 months |
||
|
Favorable |
29 |
80.6 |
|
Lost sight of |
7 |
19.4 |
Table 5: Distribution of Patients According to their Progress
Discussion
The limited identification of the underlying cause, due to the sterility of the samplesand the retrospective nature of a good phase of our study were our main limitations. Liver abscess is a wellknown tropical disease. In our study, we collected 36 cases over 18 months. The study by Diarra A et al. [5], reported 9 cases per year. This demonstrates a high frequency in our study, given the tropical geographical location of our region. Young adults were the most affected in our study. An average age of 39 to 47 years has been reported in African series.[3,5]; while Lafont, in his study in France, reported an average of 60 years [4]. This difference lies in the youthfulness of the African population. The male predominance was evident in our series. This result is consistent with the findings of many authors [4-6]. According to other authors, women are less affected due to the protective action of female sex hormones and the immune response [7]. Chronic alcohol consumption was reported by some of our patients. In the series by Bignoumba I et al.[3], the finding was 62.5%. Alcohol inhibits Kupffer cells, which are essential for eliminating infectious agents in the liver [8]. Fontan’s triad was dominant in our patients. In the series by Diarra A et al.[5], 95.1% of patients presented with fever and 93.2% with abdominal pain. This classic clinical presentation is the typical form of liver abscess reported in the literature [2,3]. The average size of the abscess was 10 cm in our patients. Bignoumba I et al.[3], they reported a size between 5 cm and 10 cm in 68.8% of cases. This result could be linked to the late consultation of our patients, due to their precarious social status in rural areas on the one hand, and their initial recourse to traditional treatment on the other. In our study, the right lobe was preferentially affected. This result does not differ from those reported in the literature [3,5,6]. This location could be explained by anatomy; the right lobe represents a larger tissue mass, and portal venous flow is greater on the right than on the left. Involvement of a single segment was more frequent in our study. In the work of Bignoumba in Gabon and Diarra in Mali, the abscess was solitary in 87.5% and 70.9% of cases, respectively [3,5].
Amoebic abscess is the most frequently reported etiology in African literature [3,6,9]. In our series, bacteriology failed to isolate any germs in almost all patients, and amoebic serology was positive in one patient. This sterility of the sample could be linked to the overuse of antibiotics for fever and to the adhesion of the amoeba to liver tissue, potentially causing false negatives. Systematic dual antibiotic therapy, including metronidazole, was the cornerstone of treatment for our patients. This therapeutic approach likely reflects the microbiological context in our country and is supported by numerous case series [3,5]. In our study, ultrasound-guided drainage was performed in more than half of the patients. In the series by Dieng M et al. [6], drainage was carried out in 82.5% of cases and in 66% of cases in Diarra’s series [5]. Surgery, in the presence of peritonitis or after drainage failure, was the second indication in our study. Bignoumba et al. [3], they reported two cases requiring additional surgical drainage. Peritonitis and deep abscesses are contraindications to, or factors that can lead to drainage failure [1,6].
In liver abscesses, clinical healing is early, while anatomical lesions may persist for several months [10]. The evolution of the patients in our study was almost entirely favorable, but we noted the persistence of the abscess in the two HIV+ patients after one month of follow-up, and we had recorded no [other cases]. In the African literature, Diarra et al. [5], reported 2 cases of death and Bignoumba et al.[3]. They recorded one death, highlighting the sometimes fatal nature of this disease [2].
Conclusion
Liver abscess remains a common condition in our practice. It generally affected adults. Fontan’s triad was frequently observed. Dual antibiotic therapy, including metronidazole, combined with instrumental intervention, was the cornerstone of treatment.
Conflicts of interest: No conflict of interest for this work
References
- Lardière-Deguelte S, Ragot E, Amroun K, Piardi T, Dokmak S, et al. (2015) Liver abscesses: diagnosis and management.J Chir Viscérale 152: 233-246.
- Singh S, Chaudhary P, Saxena N, Khandelwal S, Poddar DD, et al. (2013) Treatment of liver abscess: prospective randomized comparison of catheter drainage and needle aspiration. Ann Gastroenterol 26: 332-339.
- Bignoumba PEI, Moussavou IFM, Alilangori T, Apendi A, Nguema AGE, et al. (2020) Hepatic Abscesses in the Hepatogastroenterology Department of the CHU of Libreville: Epidemiological, Therapeutic and Evolutionary Aspects 21: 74-76.
- Lafont E, Rossi G, Rossi B, Roux O, De Lastours V, et al. (2017) Liver abscess. Journal of Anti-infectives 19: 89-99.
- Diarra A, Keita K, Traoré A, Koné A, Guindo I, et al. (2025) Liver abscesses: epidemiological, clinical and therapeutic aspects at the University Hospital Center Pr Bocar Sidy Sall of Kati (Mali). Journal of Surgery and Specialties of Mali 5: 52-62.
- Dieng M, DIOP B, KONATE I, KA O, DIA A, et al. (2007) Treatment of liver abscesses: experience of a general surgery department. Médecine d’Afrique Noire 54: 514-519.
- Weinke T, Grobusch MP, Güthoff W (2002) Amebic liver abscess--rare need for percutaneous treatment modalities. Eur J Med Res 7: 25-29.
- Khim G, Em S, Mo S, Townell N (2019) Liver abscess: diagnosis and management issues found in the low resource setting. Br Med Bull 132: 45-52.
- Thioub D, Lawson ATD, Sarr NA, Mbengue N, Ba P, et al. (2024) Profile and management of amebic liver abscess in rural Senegal. Revue Malienne d’Infectiologie et de Microbiologie 19: 56-62.
- Badaoui L, Dabo G, Sodqi M, Marih L, Lahsen AO, et al. (2014) Liver abscess due to pyogenic bacteria: clinical, morphological and therapeutic aspects - A report of 19 cases. Revue Malienne d’Infectiologie et de Microbiologie 4: 8-11.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.