Lessons Learned: Barriers to Mammogram Screening Among Women During the COVID-19 Pandemic in a Malaysian Teaching Hospital
by Li Ping Wong1*, Kah Chun Yip2, Haridah Alias1, Lee Lee Lai3, Kartini Rahmat4, Vijayanathan Anushya4, Mee Hoong See5*
1Department of Social and Preventive Medicine, Centre for Epidemiology and Evidence-Based Practice, Faculty of Medicine, Universiti of Malaya, 50603 Kuala Lumpur, Malaysia
2Faculty of Medicine, Universiti of Malaya 50603, Kuala Lumpur, Malaysia
3Department of Nursing Science, Faculty of Medicine, Universiti Malaya, 50603, Kuala Lumpur, Malaysia
4Department of Biomedical Imaging, Faculty of Medicine, Universiti Malaya, 50603 Kuala Lumpur, Malaysia
5Department of Surgery, Breast Surgery Unit, Faculty of Medicine, Universiti of Malaya, 50603 Kuala Lumpur, Malaysia
*Corresponding author: Li Ping Wong, Department of Social and Preventive Medicine, Centre for Epidemiology and Evidence-Based Practice, Faculty of Medicine, Universiti of Malaya, 50603 Kuala Lumpur, Malaysia; Mee Hoong See, Department of Surgery, Breast Surgery Unit, Faculty of Medicine, Universiti of Malaya, 50603 Kuala Lumpur, Malaysia
Received Date: 29 July 2025
Accepted Date: 04 August 2025
Published Date: 06 August 2025
Citation: Wong LP, Yip KC, Alias H, Lai LL, Rahmat K, et al. (2025) Lessons Learned: Barriers to Mammogram Screening Among Women During the COVID-19 Pandemic in a Malaysian Teaching Hospital. J Surg 10: 11403 https://doi.org/10.29011/2575-9760.011403
Abstract
Background: The COVID-19 pandemic could affect the attendance of individuals for mammogram screening for breast cancer. This study examines the prevalence of non-attendance for follow-up breast cancer screening and explores the reasons behind it during the COVID-19 pandemic at a teaching hospital in Kuala Lumpur, Malaysia.
Methods: A retrospective review of hospital records was conducted for women who were scheduled for screening mammograms from February 2019 to March 2021. Non-attendees were contacted and questioned about both the reasons for not attending and their emotional reactions to the missed opportunity.
Results: Of a total of 1004 patients scheduled for breast screening during the study period, a total of 145 (14.2%) missed breast cancer screening. Of these, a total of 82 consented to take part in the survey. When questioned about the reasons for not attending their scheduled mammogram screening, the majority (79.3%) reported that they sought screening elsewhere. A considerable proportion (31.7%) noted that they were afraid of acquiring COVID-19 in the hospital. Other reasons included financial constraints (17.1%), forgetting the appointment (17.1%), and lack of interest in carrying out the screening (12.2%). In terms of emotional responses to abstaining from mammogram screenings, 92.7% believe that the risk of contracting COVID-19 is more significant than the risk of developing cancer.
Conclusion: Findings guide strategies and interventions to ensure that breast cancer preventive measures remain accessible and effective even in the face of a global health crisis.
Introduction
The COVID-19 pandemic has introduced unprecedented challenges to patients and healthcare systems globally, impacting routine medical procedures and preventive screenings. One crucial area affected is mammogram screening participation among women [1]. Substantial decreases in breast screening volume and the number of diagnosed breast cancers were globally reported during the COVID-19 pandemic [2]. Investigating the decline in mammogram screening rates during the COVID-19 pandemic is of paramount importance as the disruption caused by the pandemic may led to substantial challenges in maintaining routine medical procedures and preventive screenings globally. Understanding the reasons behind the observed decrease in screening rates is essential for timely and regular mammogram screenings for the early detection of breast cancer, which significantly improves treatment outcomes and overall survival rates. In Malaysia, many hospitals nationwide have observed a reduction in screening rates, but there is a lack of empirical evidence formally documenting this decline in screening rates. However, there is a lack of empirical evidence formally documenting this decrease in screening rates. Reasons women refraining from mammogram screenings during the COVID-19 pandemic could include fear of exposure to the virus in healthcare settings, logistical challenges, or other pandemic-related concerns [3-5] Identifying the reasons contributing to abstaining from attending mammogram screening can help implement strategies to encourage and facilitate women to resume regular screening, mitigating potential long-term health consequences. Hence, this study aimed to investigate the prevalence and reasons behind women refraining from mammogram screenings during the COVID-19 pandemic.
Methods
A retrospective review of hospital records was conducted for women who were scheduled for screening mammograms from February 2019 to March 2021. Figure 1 shows the participant recruitment process. Non-attendees were contacted and questioned about both the reasons for not attending and their emotional reactions to the missed opportunity. Verbal consent was obtained as the study involved telephone interviews. Ethical approval was granted by the Medical Research Ethics Committee (MREC), University of Malaya Medical Centre (MREC ID No:2022112-10919)
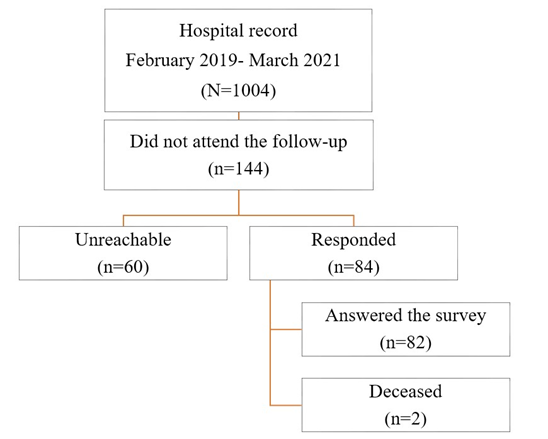
Figure 1: Flowchart illustrating the process of recruiting participants.
Results
The mean age of the 83 respondents was 58.7 years (SD ± 11.3). Out of 82 women who abstained from attending mammogram screening, 90.2% completely missed their scheduled screening, while 9.8% opted to delay or postpone their screening session. When questioned about the reasons for not attending their scheduled mammogram screening, the majority (79.3%) reported that they sought screening elsewhere (Table 1). A considerable proportion (31.7%) noted that they were afraid of acquiring COVID-19 in the hospital. Other reasons included financial constraints (17.1%) and forgetting the appointment (17.1%). A total of 12.2% reported a lack of interest in carrying out the screening.
|
Reasons |
N (%)† |
|
Afraid of hospital acquired COVID-19 infection |
26 (31.7) |
|
Afraid of acquiring COVID-19 infection through public transportation |
1 (1.2) |
|
Forgotten the appointment |
14 (17.1) |
|
Infection with COVID-19 (isolated) |
2 (2.4) |
|
Close contact with positive COVID-18 patients (Quarantine) |
1 (1.2) |
|
Interstate travel restriction |
6 (7.3) |
|
Financial reasons |
14 (17.1) |
|
Sought screening elsewhere |
65 (79.3) |
|
Postponed by the hospital |
4 (4.9) |
|
Not interested to do screening |
10 (12.2) |
†The percentages do not sum to 100% because respondents were allowed to provide more than one reason for their non-attendance.
Table 1: Reason for refraining from mammogram screening participation (N=82)
Concerning the emotional responses to refraining from engaging in mammogram screenings, a significant majority (92.7%) agreed or strongly agreed that their risk of contracting COVID-19 outweighs the risk of developing cancer. While the majority disagreed with the notion that missing mammogram screenings may not lead to serious health consequences compared to the risk of severe illness from COVID-19 (59.8%), a substantial proportion expressed strong agreement or disagreement (35.4%). There was a substantial proportion who felt mildly concerned (42.7%) or not at all worried (29.3%) about difficulties in rescheduling their next appointment. Similarly, a substantial proportion felt mildly concerned (47.0%) or not at all worried (38.6%) about missing a cancer diagnosis. Additionally, a considerable proportion felt mildly concerned (46.3%) or not at all worried (42.7%) about the potential delay in treatment associated with a delayed diagnosis (Table 2).
|
Anxiety concern |
N (%) |
|
My risk of getting COVID-19 outweighs the risk of developing cancer |
|
|
Strongly agree |
34 (41.5) |
|
Agree |
42 (51.2) |
|
Disagree |
6 (7.3) |
|
Strongly disagree |
0 (0.0) |
|
Missing mammogram screening may not lead to serious health consequences as the risk of severe illness from COVID-19 infection |
|
|
Strongly agree |
4 (4.9) |
|
Agree |
25 (30.5) |
|
Disagree |
49 (59.8) |
|
Strongly disagree |
4 (4.9) |
|
Worry about the difficulties to reschedule next appointment |
|
|
Not at all worried |
24 (29.3) |
|
Mild |
35 (42.7) |
|
Moderate |
17 (20.7) |
|
Extremely worried |
6 (7.3) |
|
Worry about missing your cancer diagnosis |
|
|
Not at all worried |
32 (38.6) |
|
Mild |
39 (47.0) |
|
Moderate |
11 (13.3) |
|
Extremely worried |
1 (1.2) |
|
Worry about delay treatment associated with delayed diagnosis |
|
|
Not at all worried |
35 (42.7) |
|
Mild |
38 (46.3) |
|
Moderate |
9 (11.0) |
|
Extremely worried |
0 (0.0) |
Table 2: Emotional responses to refraining from engaging in mammogram screenings (N=82).
Discussion
Investigating the reasons contributing to non-participation found a significant number revealed opting for screening elsewhere and concerns about presenting themselves at the hospital during the pandemic due to fears of acquiring infections within the hospital setting. Many participants reported seeking screening elsewhere and fear of acquiring COVID-19 in the hospital emerged as a prevalent concern, likewise similarly reported in many studies [6], highlighting the profound impact of the ongoing pandemic on healthcare decisions. Financial constraints also played a role, acting as a barrier for a proportion of participants, underscoring the economic factors influencing their decision-making process. Additionally, a notable percentage mentioned forgetting the appointment, indicating a potential need for improved appointment reminders or scheduling systems. This finding is consistent with earlier research, suggesting that busyness and forgetfulness in scheduling or attending mammography appointments are factors contributing to non-participation in some women [7]. Improving appointment reminder systems could help address this issue and potentially increase participation rates. Interestingly, some individuals expressed a lack of interest in undergoing the screening, underscoring the importance of addressing motivational factors to encourage participation. The study’s findings revealed significant emotions and perceptions related to abstaining from mammography screening during the COVID-19 pandemic. A considerable majority of participants expressed overriding concerns about contracting COVID-19, which eclipsed their perceived risk of developing cancer. Notably, a sizable proportion of participants disagreed with the idea that skipping mammograms might have severe health consequences. This disparity in views suggests that while some recognize the potential gravity of missed screenings, others may minimize its importance. This contrast highlights the necessity for tailored interventions to promote recognition of the health risks associated with neglecting screenings.
The study further illuminates the participants’ attitudes toward logistical aspects, such as rescheduling appointments.
A substantial percentage expressed either mild concern or no worry at all regarding the difficulties in rearranging their next screening. It is noteworthy to consider that in teaching hospitals, rescheduling for the next screening after a missed appointment may take time, leading to additional delays in the screening and diagnostic process. On an individual patient level, it is crucial to raise awareness about the extended time it takes to reschedule appointments and its consequences. Delays in screening mammography during the pandemic of COVID-19 were reported to result in a 60% decrease in breast cancer diagnoses by a large tertiary care institution in the United States [8]. Further, rescheduling mammogram screenings may strain hospital resources, causing logistical challenges and potential delays in accommodating patients. Hence, it is crucial to adopt measures aimed at reducing patient non-attendance and tackling the difficulties linked to rearranging appointments for screening mammography at the organizational level to ensure timely and effective screening procedures. A considerable portion of participants demonstrated a noteworthy level of anxiety regarding the possibility of missing a cancer diagnosis, underscoring their awareness of the severe repercussions associated with skipping screenings. Similarly, a significant percentage expressed worry about the potential delay in treatment linked to a delayed diagnosis. On a positive note, women expressing concern about cancer diagnosis and treatment delays associated with delayed diagnosis serve as a positive indicator that encourages the pursuit of missed diagnoses. In contrast, heightened worry or anxiety related to missing mammogram screenings may contribute to mental stress, potentially disrupting overall well-being. During the pandemic, women’s perception of risk changed, prioritizing concerns about contracting COVID-19 or acquiring infections in a hospital over their willingness to attend mammogram screenings [9]. This shift, as similarly found in this study, underscores the essential need for well-designed communication and educational campaigns. Initiatives aimed at raising awareness about the tangible consequences of skipping screenings are necessary, especially emphasizing the importance of addressing changing risk perceptions during unprecedented times.
Conclusion
Our findings underscore the multifaceted factors contributing to non-participation in mammogram screenings. Effective interventions and communication strategies should consider addressing fears related to COVID-19, financial constraints, and lack of motivation to enhance participation rates and ultimately improve breast cancer screening outcomes. The study also reveals the complex emotions and perceptions surrounding the decision to abstain from mammogram screenings during the COVID-19 pandemic. The results emphasize the imperative of addressing individual concerns and highlighting the tangible emotional and health consequences of missing screenings to ensure proactive healthcare decision-making. Given the potential prevalence of under-diagnoses, health authorities must develop strategies that specifically address underdiagnosed women. The findings can inform targeted interventions to address the underlying factors and contribute to the resilience of healthcare systems in the face of unprecedented challenges.
Funding: None to acknowledge.
Conflict of interest: All authors declare no conflict of interest.
Ethical approval: The study is approved by the University of Malaya Medical Centre’s Medical Ethics Committee UMMC MECID.NO: No:2022112-10919 and conforms to the Declaration of Helsinki 1975.
Author’s contribution: MHS, LPW and KCY conceptualised, conceived and designed the study and analysed the data. KCY, LLL, VA and KR collected data. LLL, WLP and HA analysed the data. All authors have reviewed the manuscript for important intellectual content and approved the final version of the manuscript.
References
- Pifarré I Arolas H, Vidal-Alaball J, Gil J, López F, et al. (2021) Missing Diagnoses during the COVID-19 Pandemic: A Year in Review. Int J Environ Res Public Health 18: 5335.
- Li T, Nickel B, Ngo P, McFadden K, Brennan M, (2023) A systematic review of the impact of the COVID-19 pandemic on breast cancer screening and diagnosis. Breast 67: 78-88.
- Lee WJ, Shah Y, Patel N, Ku A, Rodriguez A, et al. (2023) The Consequences of COVID-19 on Breast Cancer Screenings in an Underserved Urban Population and the Screening Access of Value for Essex Program’s Efforts to Control the Damage. Cureus 15: e42338.
- Richman I, Tessier-Sherman B, Galusha D, Oladele CR, Wang K (2023) Breast cancer screening during the COVID-19 pandemic: moving from disparities to health equity. J Natl Cancer Inst 115: 139145.
- Chou CP, Pan HB, Yang TL, Chiang CL, Huang JS, et al. (2021) Impact of the COVID-19 pandemic on the volume of mammography examinations in Southern Taiwan. Breast J 27: 89-91.
- Duarte MBO, Argenton JLP, Carvalheira JBC (2022) Impact of COVID-19 in Cervical and Breast Cancer Screening and Systemic Treatment in São Paulo, Brazil: An Interrupted Time Series Analysis. JCO Glob Oncol 8: e2100371.
- Gierisch JM, O’Neill SC, Rimer BK, DeFrank JT, Bowling JM, et al. (2009) Factors associated with annual-interval mammography for women in their 40s. Cancer Epidemiol 33: 72-88.
- Amornsiripanitch N, Chikarmane SA, Bay CP, Giess CS (2021) Patients characteristics related to screening mammography cancellation and rescheduling rates during the COVID-19 pandemic. Clin Imaging 80: 205-210.
- Bosch G, Posso M, Louro J, Roman M, Porta M, et al. (2022) Impact of the COVID-19 pandemic on breast cancer screening indicators in a Spanish population-based program: a cohort study. Elife 11: e77434.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.