Leptomeningeal Metastasis as an Initial Presentation of Breast Cancer Recurrence After 6 Years of Remission: A Case Report
by Firas Al Rashdi1, Humaid Al Farii2*
1Oman Medical Specialty Board, Muscat, Seeb, Oman
2Consultant Spine and Oncology, Musacat, Seeb, Oman
*Corresponding Author: Humaid Al Farri, Consultant Spine and MSK Oncology, Department of Surgery, Orthopedics Division, Musacat, Seeb, Oman
Received Date: 10 July 2025
Accepted Date: 16 July 2025
Published Date: 18 July 2025
Citation: Rashdi FA, Farii HA (2025) Leptomeningeal Metastasis as an Initial Presentation of Breast Cancer Recurrence After 6 Years of Remission: A Case Report. J Surg 10: 11386 https://doi.org/10.29011/2575-9760.011386
Abstract
Leptomeningeal Metastasis (LM) is a rare but increasingly recognized complication of solid tumors, particularly breast, lung, and melanoma, affecting up to 15% of patients. The rise in incidence is linked to improved cancer survival and advanced imaging, though prognosis remains poor, with median survival around 6.9 months. We report a case of a 54-year-old female with a history of breast cancer presenting with paraplegia due to LM. MRI revealed dural thickening compressing the spinal cord, the patient was taken for decompression, though her neurological deficits persisted. Current treatment options are limited, and recent studies highlight the potential of Proton Craniospinal Irradiation (pCSI) for improved outcomes. Further research is essential to enhance treatment and survival for patients with LM.
Keywords: Breast Cancer; HER2 Negative Breast Cancer; Leptomeningeal Metastasis; Radiotherapy
Introduction
Leptomeningeal Metastasis (LM) is quite a rare entity that has become more common over the years. LM is diagnosed in roughly 4-15% of patients with solid tumors [1]. Breast cancer, lung cancer, and melanoma are the most common solid tumors that were associated with LM [2]. Its increasing incidence is mostly due to the advancement in cancer care therefore improving survival rates and the widespread availability of Magnetic Resonance Imaging (MRI). Moreover, another explanation for the increasing incidence of CNS involvement is probably because most targeted therapies used in breast cancer have poor blood brain barrier penetration [3]. Overall prognosis is poor in such situations, A retrospective cohort study of 423 patients showed the overall median survival is around 6.9 months [4]. Due to the scarcity of cases, there has not been a well-established guideline in dealing with such situations.
Case Report
We report a case of a 54-year-old female with a history of right sided breast cancer cT4b with skin and node involvement diagnosed in 2015, Estrogen and progesterone positive, HER2 negative Ki67 25%, underwent 4 cycles of chemotherapy with Adriamycin, cyclophosphamide and Docetaxel, followed by modified radicle mastectomy with right axillary clearance, was commenced on letrozole and completed radiotherapy by 2017. she achieved full remission. She presented 6 years later with sudden paraplegia which was proceeded with a 1-week history of persistent headache, increased fatiguability associated with paresthesia mainly in her abdomen and bladder incontinence. Her examination showed hypotonic areflexia of Bilateral lower limbs with power of 0/5 on the right side and 1/5 with toe flexion only. Her upper limb examination was 4/5 on the left and 3/5 on the right side due to residual weakness on the right as a result of radiotherapy. She had impaired sensation up to T4, she had a normal cranial nerve examination
Neuroimaging
MRI showed a long segment of enhancing Dural thickening measuring up to 6.1cm in lower cervical and upper dorsal level circumferentially compressing the spinal cord, Few metastatic deposits were identified along the spinal cord as well (Figure 1).
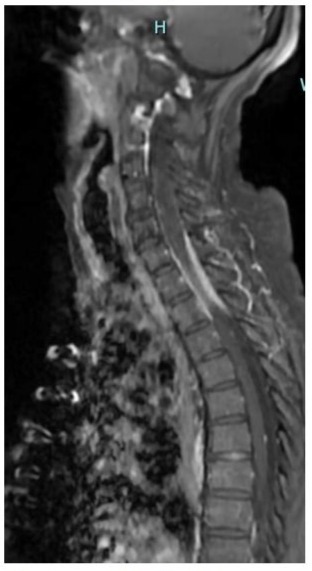
Figure 1: This is a sagittal T2 Weighted image showing high signal intensity of the cervical spinal cord
Surgical Procedure
Based on the above MRI findings and the presumption that the compression was most likely extradural, she was taken for an emergent decompression of C6-T1 under imaging, intra operatively, no obvious mass could be seen, ultrasound intra op was done which showed bulky thickening of the Dura matter. Henceforth a durotomy was done and debulking of the thick dura matter was commenced, biopsies were taken which showed intraductal adenocarcinoma. Dura was then closed, area was closed and a drain placed (Figures 2-5).

Figure 2: Intraoperative photo showing the dura at the level of the cervical spine, there is no external mass identified.
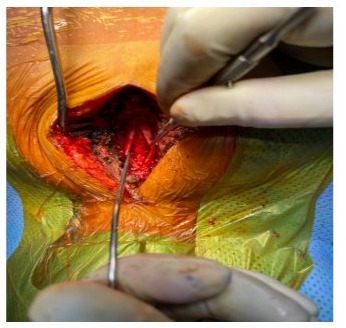
Figure 3: In the above photo, durotomy was done and the spinal cord was exposed, no obvious lesion was identified, here we appreciated increased thickness of the dura matter.

Figure 4: Intraoperative ultrasound imaging showing the spinal cord prior to durotomy, no obvious external compression seen.
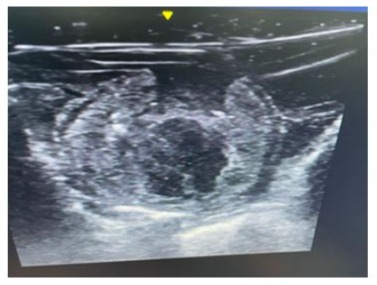
Figure 5: The above photo is an intraoperative ultrasound which shows evidence of increased thickness of the dura matter.
Post Operative Course
Unfortunately, Her neurological deficit did not improve postoperatively. She was transferred to another center to receive palliative care
Discussion
The molecular pathway of leptomeningeal metastasis is still poorly understood, therefore limiting therapy options
One study that investigated breast cancer in mice showed that breast cancer cells invade the leptomeninges through albumin migration along blood vessels that connect vertebral or calvaria bone marrow and meninges effectively bypassing the blood brain barrier [5]. Photon involved-field radiotherapy is thought to be the standard of care for such patients with LM from solid tumors. Another retrospective Japanese paper looked into ER positive HER2 negative breast cancer, patients were divided into 3 groups: patients with brain metastasis only, patients with both brain and leptomeningeal metastasis, and patients with leptomeningeal metastasis alone The study included around 369 patients, it concluded that patients with leptomeningeal metastasis alone had later onset, poorer performance status, more symptoms, and more skull metastasis than the other groups. Moreover, they had the lowest overall survival rate [6]. Furthermore, one phase 2 randomized control trial investigated the use of Proton Craniospinal Irradiation (pCSI) encompassing the entire central nervous system and compared it with the standard Photon involved-field radiotherapy. This study showed superior outcomes in terms of Overall survival and CNS progression free survival with no increase in treatment related adverse events [6].
Conclusion
Leptomeningeal metastasis from solid tumors is at an increased incidence due to the advances of cancer treatment and imaging modalities, there is still much to know with regards to the pathophysiology and optimal treatment modalities, there is special attention in recent publications given to this issue as it poses a great challenge in treatment. Pursuit of further treatment is necessary for better overall survival for such patients.
References
- Taillibert S, Laigle-Donadey F, Chodkiewicz C, Sanson M, Hoang-Xuan K, et al. (2005) Leptomeningeal metastases from solid malignancy: a review, J Neurooncol 75: 85-99.
- Cheng H, Perez-Soler R (2018) Leptomeningeal metastases in nonsmall-cell lung cancer, Lancet Oncol, p. 19: 43-e55.
- Mills MN, Figura NB, Arrington JA, Michael Yu H, Etame AB, et al. (2020) Management of brain metastases in breast cancer: A review of current practices and emerging treatments, Breast Cancer Res. Treat 2020: 279-300.
- Znidaric T, Gugic J, Marinko T, Horvat AG, Kosir MSP, et al. (2019) Breast cancer patients with brain metastases or leptomeningeal disease: 10-year results of a national cohort with validation of prognostic indexes, Breast J 2019: 1117-1125.
- Whiteley AE, Ma D, Wang L, Yu SY, Yin C, et al. (2024) Breast cancer exploits neural signaling pathways for bone-to-meninges metastasis, Science 21: 384.
- Yang JT, Wijetunga NA, Pentsova E, Wolden S, Young RJ, et al. (2022) Randomized Phase II Trial of Proton Craniospinal Irradiation Versus Photon Involved-Field Radiotherapy for Patients With Solid Tumor Leptomeningeal Metastasis, J Clin Oncol 40: 3858-3867.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.