Laparoscopy Distal Common Bile Duct Stenting in Case of Malignant Obstruction: A Minimally Invasive Technique
by Takkal A. Malik¹, Yassine Mohamed¹, Takkal Adam2, El Aziz Mériem3, Delgadillo Xavier3,4*
1Department of General and Digestive Surgery, Assalam Hospital, 90001-Tangier, Morocco
2Faculté de Médecine de l’Université Libre de Bruxelles-ULB, 1070-Brussels, Belgium
3Saratov State Medical University, 410012-Saratov, Russia
4Unité Spécialisée de Chirurgie, CMC-Volta, 2300-La Chaux-de-Fonds, Switzerland
*Corresponding author: Delgadillo Xavier, Unité Spécialisée de Chirurgie, CMC-Volta, 2300-La Chaux-de-Fonds, Switzerland
Received Date: 22 January 2026
Accepted Date: 28 January 2026
Published Date: 30 January 2026
Citation: Citation: TAKKAL MA, MOHAMED Y, TAKKAL A. EL AZIZ M, DELGADILLO X. (2026) Laparoscopy Distal Common Bile Duct Stenting in case of Malignant Obstruction: A Minimally Invasive Technique. J Surg 11: 11550 https://doi.org/10.29011/2575-9760.011550
Abstract
Background: Malignant distal Common Bile Duct (CBD) obstruction, most frequently related to pancreatic head carcinoma, often requires biliary decompression before surgery or as palliative treatment.
Technique: We describe a laparoscopic transcystic approach that combines diagnostic staging laparoscopy with direct access to the biliary tree through the cystic duct, allowing guide wire passage across the obstruction and deployment of an endoluminal biliary stent without papillary manipulation.
Results: In our early experience, this procedure provided reliable biliary drainage while also allowing peritoneal lavage and, when needed, targeted biopsies for staging. Because it avoids both endoscopic sphincterotomy and pancreatic duct instrumentation, it may lower the risk of post-procedure pancreatitis and help preserve normal sphincter function.
Conclusion: Laparoscopic transcystic stenting is a feasible minimally invasive option for selected patients with malignant distal CBD obstruction, particularly when endoscopic drainage is unavailable, or has failed. It also offers a laparoscopy staging.
Keywords: Biliary Stenting; Laparoscopic Transcystic Access; Malignant Biliary Obstruction
Introduction
Pancreatic cancer continues to be a primary contributor to global cancer-related mortality and is frequently diagnosed at advanced stages. Actually, there are an estimated 510,922 new cases and 467,409 deaths worldwide, affirming its status as a leading cause of oncological death [1]. A frequent clinical manifestation of tumors involving the pancreatic head, the periampullary region, or the distal biliary tree (such as cholangiocarcinoma) is obstructive jaundice resulting from malignant distal Common Bile Duct (CBD) occlusion. If left untreated, this important biliary stasis can precipitate acute cholangitis, progressive hepatic dysfunction, debilitating pruritus, and malnutrition, ultimately delaying essential therapeutic interventions such as surgical resection, neoadjuvant or palliative chemotherapy, or other supportive care measures [2]. Endoscopic Retrograde Cholangiopancreatography (ERCP) with biliary stenting remains the gold-standard drainage strategy; however, its efficacy is often hindered by technical challenges, including difficult biliary cannulation, tumor-induced anatomical distortion, or gastric outlet obstruction [3,4]. While Percutaneous Transhepatic Biliary Drainage (PTBD) serves as a viable alternative, it is frequently associated with specific morbidities, such as catheter-related infections, bile leakage, and hemorrhage [5]. To address these limitations, we developed a minimally invasive laparoscopic technique designed to provide (a) Effective biliary decompression via direct transcystic access and subsequent stent placement ; and (b) Synchronous staging laparoscopy, incorporating peritoneal lavage for cytology and targeted biopsy where indicated, to ensure comprehensive oncological assessment.
Minimally Invasive Technique
The procedure is performed under laparoscopy approach, under general anesthesia, setting the patient in French position (surgeon between the legs), with the monitor at the patient’s head. A nasogastric tube may be placed to decompress the stomach if nesesary. Malignant distal Common Bile Duct (CBD) obstruction presents a significant clinical challenge, often necessitating effective biliary decompression prior to definitive oncological treatment. Traditional Endoscopic Retrograde Cholangiopancreatography (ERCP) is the established first-line intervention; however, its application can be limited by failed cannulation, complex tumor anatomy, or duodenal invasion.To circumvent these limitations, we employ a novel, entirely laparoscopic approach, describing the core objective of this technique, how to facilitate by a transcystic access to the biliary system under minimal invasive approach. The procedure starts with the establishment of standard laparoscopy desinfection and ports placement, with the aim to perform a meticulous dissection of the hepatoduodenal ligament that will expose the cystic duct, as it is described step by step as follows :
Phase I°. Staging laparoscopy for establishing an insufflation of CO2 controlled at 12 mmHg of pneumoperitoneum pressure, and perform a systematic exploration of the peritoneal cavity and liver surface. Collect peritoneal fluid for cytology and biopsy for any suspicious peritoneal or hepatic metastatic lesions Figure 1.
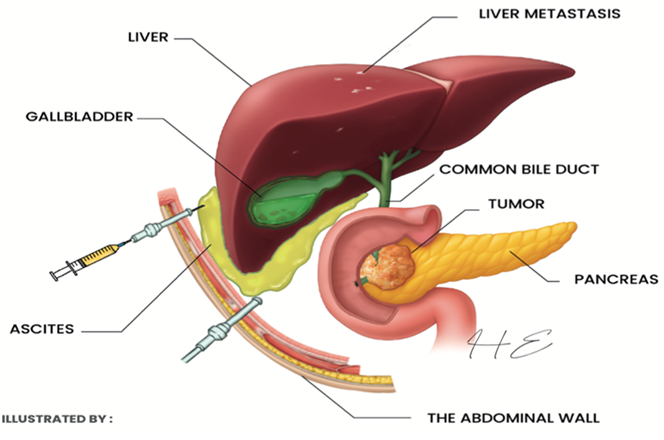
Figure 1: Laparoscopy for staging.
Phase II°. Gallbladder decompression to facilitate its safe grasping and cephalad retraction, the maneuver will decompress the gallbladder suffering generally of hydro-cholecystitis by needle aspiration under direct vision.
Phase III°. Exposure of the cystic duct and trans-cystic access obtained by a complete dissection of Calot’s triangle to identify the cystic duct and cystic artery. We always clip the cystic duct proximally (toward the gallbladder) to prevent bile spillage, followed by the creation of a small transversal section of the cystic duct followed by the introduction of a 0.035" x 150 cm hydrophilic-coated guidewire through the epigastric port.
Phase IV°. Guidewire passage across the stricture in order to advance it through the cystic duct and reach the CBD under gentle fluoroscopic control. The malignant stricture was successfully traversed, and the guidewire was advanced through the sphincter of Oddi into the duodenum, as described in Figure 2.
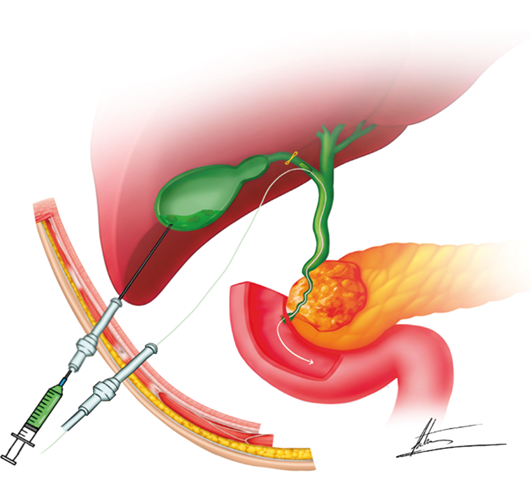
Figure 2: Laparoscopic guide-wiring across the stricture.
Phase V°. Sequential ductal dilation in order to achieve incremental diametric expansion, the cystic duct insertion site and distal Common Bile Duct (CBD) stricture were serially dilated with 6 French and 8 French catheters in a wire-guided fashion as shown in Figure 3.
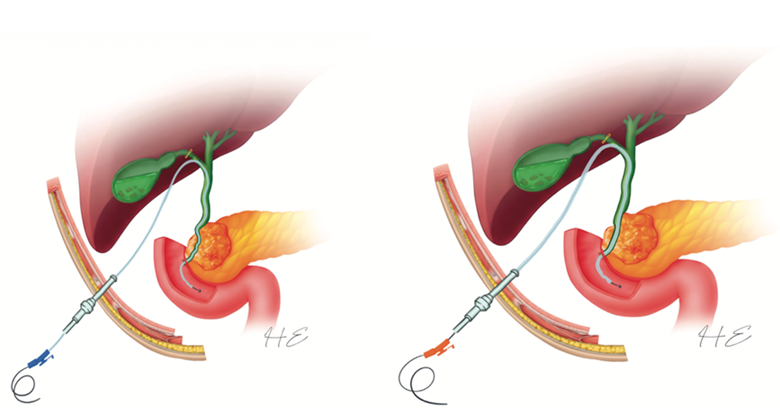
Figure 3: Laparoscopic Common Bile Duct (CBD) dilation.
Phase VI°. Stent deployment by the endoprosthesis advancement in an over-the-guide wire fashion, ensuring the distal portion traversed the sphincter of Oddi into the duodenum and the proximal margin was situated superior to the site of malignant obstruction, as described in Figure 4.
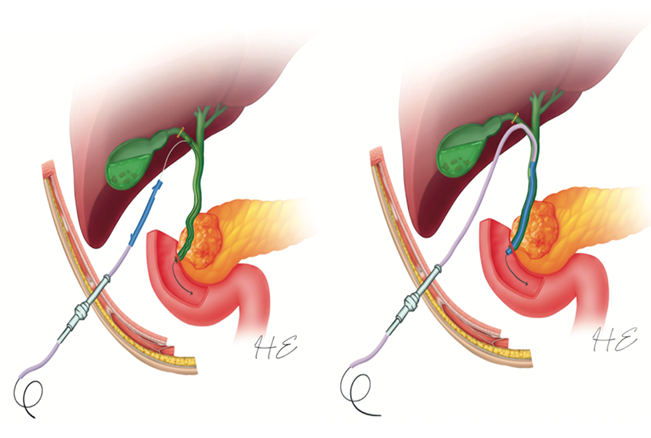
Figure 4: Deployment of the stenting device.
Phase VII°. Confirmation of the stent position and drainage to verify the correct stent positioning and the correct free hepatic flow into the duodenum, we performed an intraoperative cholangiography through the transcystic catheter to verify and to record stent location as shown in Figure 5.
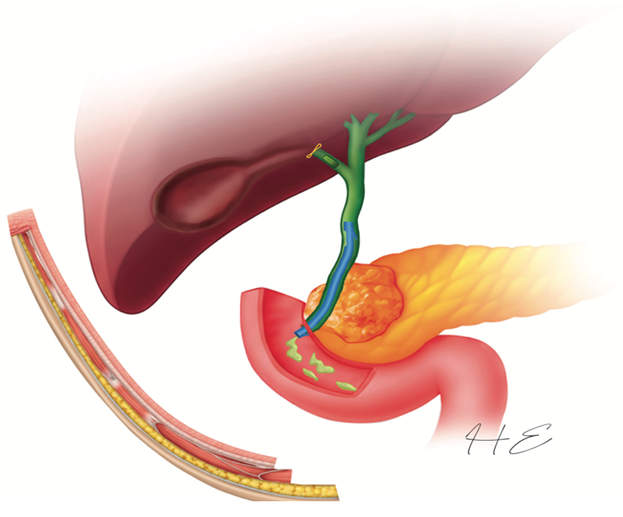
Figure 5: Drainage and stent positioning control.
Phase VIII°. Completion cholecystectomy performed by a standard laparoscopic procedure in order to prevent secondary cholecystitis and other gallbladder‑related complications. Sometimes we have to consider to leave a subhepatic drainage in prevention of biliary ascites.
Discussion
Nowadays, ERCP remains a first‑line modality for malignant biliary drainage, but procedure‑related adverse events are well described. In a multicenter prospective series of 2,347 patients undergoing endoscopic biliary sphincterotomy, the overall 30‑day complication rate was 9.8%, including pancreatitis (5.4%) and hemorrhage (2.0%) [4]. Percutaneous transhepatic drainage offers an alternative route but can be complicated by bleeding, bile leakage, infection, and catheter dysfunction, particularly in frail patients [5]. The laparoscopic transcystic approach offers potential advantages: (a) preservation of sphincter of Oddi integrity by avoiding sphincterotomy; (b) the ability to combine drainage with staging laparoscopy, which can reveal occult metastatic disease not detected on CT scan/MRI or PET CT imaging [6,7]; and (c) systematic cholecystectomy is performed not only to reduce possible secondary hydro cholecystitis but to reduce the risk of gallbladder‑related complications due to high pressure caused by stent placing. Though the base guideline is slightly older, more recent clinical practice updates continue to define the standard of care for using Self-Expandable Metal Stents (SEMS) for palliative drainage of extrahepatic malignant biliary obstruction [8]. However, this technique demands surgical advanced laparoscopic skills, appropriate wires, catheters, and fluoroscopy. In addition, plastic stents may have limited patency in malignant obstruction; selection of stent type and plans for exchange should be individualized without forgetting the possibility of laparoscopic choledochotomy to have an access over the obstruction, as described by Yamada et al. [9] on a reviewed highlights description in recent advancements in minimally invasive techniques for distal strictures, specifically focusing on the integration of endoscopic ultrasound-guided drainage and innovative stent designs to improve patient outcomes. Overall, laparoscopic transcystic stenting may be considered as a complementary option in centers where staging laparoscopy is part of the standard pathway or an alternative option when endoscopic drainage is not feasible or contraindicated, and by the other hand evolution of laparoscopic common bile duct explorations and the use of laparoscopic techniques resolve biliary obstruction with reduced patient risk compared to open surgery [10].
Conclusion
Laparoscopic transcystic stenting is a safe and minimally invasive technique for selected patients with malignant distal CBD obstruction. It combines biliary decompression with the benefits of staging laparoscopy and avoids papillary manipulation. However, future randomized studies will be needed to confirm its role in the current therapeutic arsenal of biliary drainage. Finally, transcystic stenting of the lower CBD as a safe procedure, allowing relief & biliary decompression and avoids any hazardous papillary manipulation.
References
- International Agency for Research on Cancer (IARC) (2026) GLOBOCAN 2022: Pancreas cancer fact sheet.
- Kruse EJ (2010) Palliation in pancreatic cancer. Surg Clin North Am 90: 355-364.
- Dumonceau JM, Andriulli A, Elmunzer BJ (2020) ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 52: 127-149.
- Freeman ML, Nelson DB, Sherman S (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335: 909-918.
- Molina H (2021) Complications of percutaneous biliary procedures. Semin Intervent Radiol 38(3): 266-281.
- O'Halloran EA, Board T, Lefton M, Devarajan K, Dotan E, et al. (2021) Predicting positive peritoneal cytology in pancreatic cancer. J Cancer Res Clin Oncol 147: 1825-1832.
- Peng JS, Mino J, Monteiro R (2017) Diagnostic laparoscopy prior to neoadjuvant therapy in pancreatic cancer is high yield: an analysis of outcomes and costs. J Gastrointest Surg 21: 1420-1427.
- Dumonceau JM, Tringali A, Papanikolaou IS (2018) Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline – Updated 2021.Endoscopy 50: 910-930.
- Yamada R, Miwata T, Nakamura Y, Nose K, Tanaka T, et al. (2025) Advances in Endoscopic Management of Distal Biliary Stricture: Integrating Clinical Evidence into Patient-Specific Decision-Making. Cancers (Basel) 7: 2644.
- Sotirov D (2024) Laparoscopic Approach in the Case of Biliary Obstruction: Choledocholithiasis. Current Concepts and Controversies in Laparoscopic Surgery. Intech Open.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.