Isolated Adrenocorticotropic Hormone Deficiency Associated with Prolonged QT Interval in a Pediatric Patient: A Case Report and Review of Literature
by Alharbi R4, Bin Shaman A4, Alsubhi A1, Aldubayee M2,4,5, SA. Alghamdi3, Eyaid W*1,4,5
1Department of Genetics and precision medicine, King Abdulaziz Medical City, Riyadh, Saudi Arabia
2Department of Pediatrics, King Abdulaziz Medical City, Riyadh, Saudi Arabia
3Cardiac Sciences Department, Section of Pediatric Cardiology, King Abdulaziz Cardiac Center, Ministry of National Guard Health Affairs, Riyadh Arrhythmia division, Prince Sultan Cardiac Center, Riyadh, Saudi Arabia
4King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
5King Abdullah International Medical Research Center (KAIMRC), Riyadh, Saudi Arabia
*Corresponding author: Wafaa Eyaid, Department of Genetics and precision medicine, King Abdulaziz Medical City, Riyadh, Saudi Arabia.
Received Date: 26 December 2024
Accepted Date: 31 December 2024
Published Date: 06 January 2025.
Citation: Alharbi R, Shaman BA, Alsubhi A, Aldubayee M, Alghamdi SA, et al. (2024) Infectious Causes of Hypopituitarism in Children: A Systematic Review. Arch Pediatr 8: 320. https://doi.org/10.29011/2575-825X.100320
Abstract
A 5-day-old baby girl was admitted to the pediatric intensive care unit (PICU) with non-ketotic hypoglycemia, abnormal movement, bradycardia, and a prolonged QT interval. Initial investigations, including whole exome sequencing, revealed a likely pathogenic variant in the TBX19 gene, which was associated with congenital isolated adrenocorticotropic hormone deficiency (ACTH). Upon initiating hydrocortisone treatment, there was significant improvement in the QT interval, indicating a potential link between cortisol deficiency and cardiac arrhythmias. Despite the initial success, the patient lost follow-up after discharge and was later readmitted at 16 months with recurrence of similar symptoms. Restarting hydrocortisone therapy resulted in improvements in electrocardiogram findings and her associated bradycardia. This case highlights the critical relationship between cortisol deficiency and prolonged QT interval and emphasizes the importance of early diagnosis and management of adrenal insufficiency in pediatric patients. The precise mechanisms underlying the association remain poorly understood, warranting further investigation into the role of glucocorticoids in cardiac function and the potential for life-threatening arrhythmias. This study aims to present this unique case and conduct a comprehensive literature review on the subject.
Keywords: Prolonged QTc interval; Hypoglycemia; TBX19; Hydrocortisone.
Introduction
A prolonged QTc interval, which can be inherited or acquired, poses a significant risk to the life of pediatric patients. Secondary causes are often linked to imbalances in electrolytes, medication usage or exposure to toxins. These causes may also be related to abnormal myocardial disease. In our case report, we discuss the connection between adrenocorticotropic hormone deficiency and a prolonged QTc interval. We observed that the QTc interval improved following treatment with hydrocortisone.
Case report
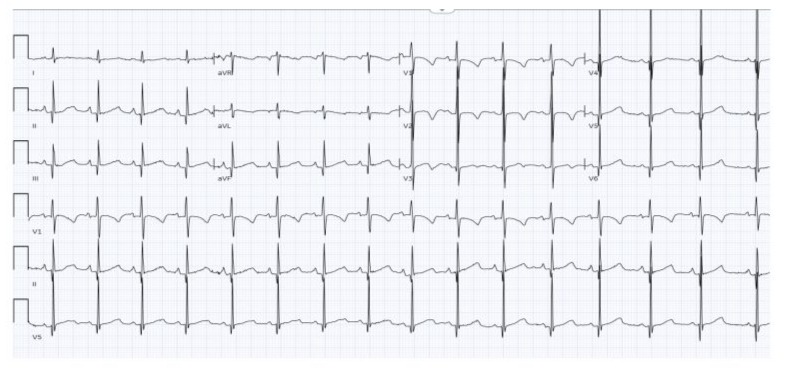
A 5-day old infant girl was admitted to the Pediatric Intensive Care Unit (PICU) due to non-ketotic hypoglycemia. She exhibited abnormal movements, bradycardia, and a progressive prolongation of the QT interval. Whole exome sequencing revealed a likely pathogenic variant in the TBX19 gene, which is associated with congenital isolated central adrenocorticotropic hormone (ACTH) deficiency. The patient was commenced on hydrocortisone treatment, resulting in an improvement of her QT interval length. However, after being discharged, the patient discontinued her medications without medical advice.
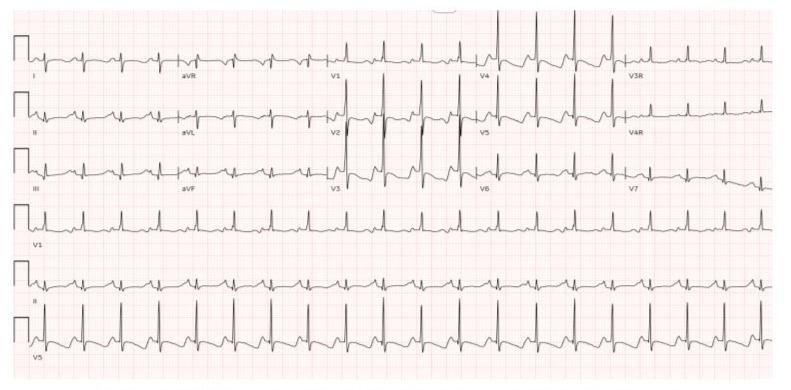
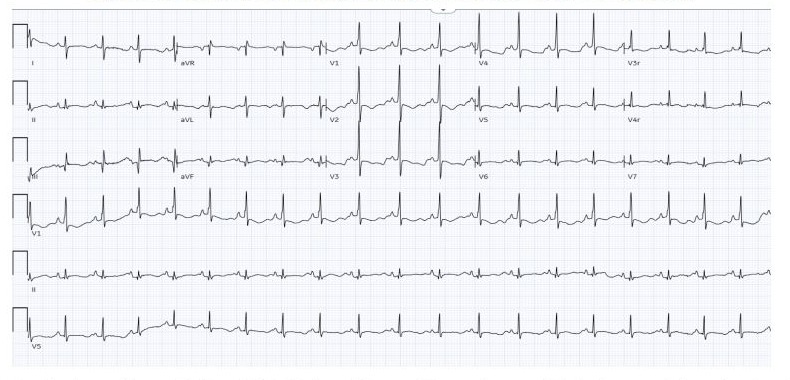
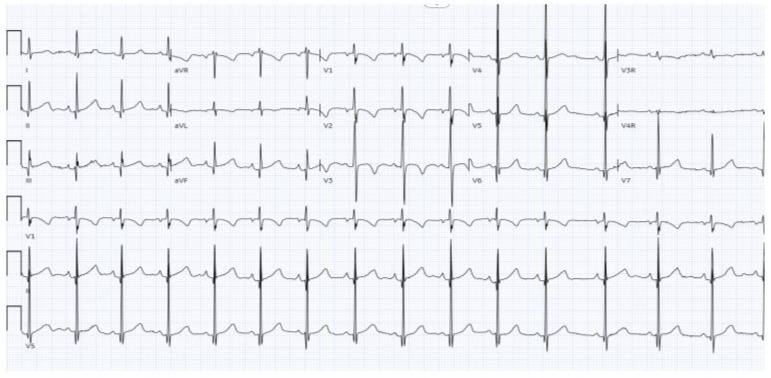
At the age of 16 months, she presented to the Emergency Room (ER) with seizures, fever, tachycardia, decreased level of consciousness and non-ketotic hypoglycemia. Her electrocardiogram (EKG) at that time showed sinus bradycardia, with a heart rate that could not be determined, and a QTc interval of 550 milliseconds (Figure 1A, 1B). She was readmitted to the PICU and hydrocortisone treatment was resumed. Biochemically, she exhibited adrenal insufficiency that did not meet the criteria for neither central or peripheral etiology. The patient's ACTH level was measured to be less than 1 pg/mol, and an ACTH stimulation test revealed a blunted response. Cortisol levels measured 30 and 60 minutes after the administration of ACTH consistently remained low. Thyroid-stimulating hormone (TSH) level was measured at 1.2 mlU/L, while the free thyroxine (T4) level was 12.6 pmol/L, and the free triiodothyronine (T3) level was 4.64 pmol/L.
Apart from the aforementioned EKG findings, an echocardiography showed a structurally normal heart with a small patent foramen ovale (PFO). Abdominal ultrasonography revealed a persistently thrombosed left portal vein, which did not require anticoagulant therapy. Following the reintroduction of hydrocortisone and levothyroxine, the QTc interval normalized once again.
Figure 1A: Brain MRI.
Figure 1B: Brain MRI.
Discussion
The exact mechanism underlying the association between cortisol deficiency and prolonged QT interval is not fully understood. Adrenal insufficiency can manifest in various ways, such as hypotension, hypoglycemia, and electrolyte imbalance. One crucial observation in this case is the presentation with fever associated with significant bradycardia, prolonged QTc interval and normal plasma electrolytes. Along with hypothyroidism and blunted ACTH challenging test showed low cortisol level. The direct effect of low glucose on the human Ether-à-go-go Related Gene (hERG) ion channel and hypokalemia has been reported to prolonged QT interval in individuals with type 1 and type 2 diabetes [1-5]. Glucocorticoid has been reported to be important for the maintenance of membrane calcium transport function in the cardiac sarcoplasmic reticulum [6]. It has been also reported that glucocorticoid up-regulates expression levels of various ion channels, including IKs (mink, KvLQT1) and IKr (hERG, MiRP1) by inducing expressions of the serum- and glucocorticoid-inducible kinase (SGK1) [7]. Since these IK channels induce outward potassium currents, glucocorticoid deficiency may extend duration of action potentials by reducing expressions of SGK1 and these ion channels [5]. This prolongation improved dramatically after hydrocortisone administration. Our genetic testing revealed a pathogenic variant in the TBX19 gene that is associated with congenital isolated adrenocorticotropic hormone deficiency.
There are few reported cases of isolated adrenocorticotropic hormone deficiency that causes QT prolongation with no electrolytes disturbance. We searched the literature and no pediatric cases were reported in this regard. However, in adult patients we have found case about a 63-year-old lady with hypopituitarism and prolongated QTc interval that progressed to polymorphic VT. She had low cortisol, luteinizing hormone, follicle stimulating hormone, and prolactin with relatively low corticotropin, while having normal thyroid hormone and serum electrolytes. QTc length was normalized with hydrocortisone treatment [1].
Another case described a 44-year-old presented in cardiac arrest and EKG findings of polymorphic ventricular tachycardia and prolonged QTc interval.
Additional laboratory tests showed low baseline cortisol and ACTH levels. Corticotropin-releasing hormone, gonadotropin- releasing hormone and thyrotropin-releasing hormone stimulation tests were carried on and showed a poor response to CRH stimulation. On the other hand, ACTH stimulation was normal and she had high thyroid-stimulating hormone level. EKG findings improved after starting steroid and levothyroxine treatment [2].
One case reported about a 72-year-old man presented to the ER with altered level of consciousness and severe hypoglycemia. Earlier, he had nonvalvular chronic atrial fibrillation with preserved left ventricular ejection fraction. Then he suddenly collapsed with EKG showed that QT intervals were unexpectedly prolonged that progressed to torsade de pointes and ventricular fibrillation. His lab work was suggestive of cortisol deficiency. After starting hydrocortisone replacement therapy QTc was gradually normalized [3].
Although there are several genetic mutations causing a congenital long QTc interval but we did not find any in our patient as whole exome sequencing in 2019 and reanalysis of whole exome sequencing raw data in 2021 were both negative for variants causing such prolongation. Likely pathogenic mutation in TBX19 leading to DNA binding defects causing congenital isolated adrenocorticotropic hormone deficiency. Such patients will present with neonatal onset hypoglycemia and seizures. Biochemically; plasma cortisol and ACTH are low with diminished response to CRH. We believe that in this case the low serum cortisol caused the prolonged QTc.
References
- Komuro J, Kaneko M, Ueda K, Nitta S, Kasao M, et al. (2016) Adrenal insufficiency causes life‐threatening arrhythmia with prolongation of QT interval. Heart vessels 31: 1003-1005.
- Kanamori K, Yamashita R, Tsutsui K, Hara M, Yuji Murakawa, et al. (2014) Long QT syndrome associated with adrenal insufficiency in a patient with isolated adrenocorticotropin hormone deficiency. Intern Med 53: 2329-2331.
- Shinya Nishizawa, Takeshi Nakamura, Tetsuro Hamaoka, Akiyoshi Matsumuro, Takahisa Sawada, et al. (2009) Lethal arrhythmia and corticosteroid insufficiency. Am J Emerg Med : 1167e1-3.
- Zhang Y, Han H, Wang J, Wang H, Yang B, Wang Z (2003) Impairment of human ether-à-go-go-related gene (HERG) K+ channel function by hypoglycemia and hyperglycemia. Similar phenotypes but different mechanisms. J Biol Chem 278: 10417-10426.
- Marques JL, George E, Peacey SR, Harris ND, Macdonald IA, et al. (1997) Altered ventricular repolarization during hypoglycaemia in patients with diabetes. Diabet Med 14: 648-654.
- Lang F, Shumilina E (2013) Regulation of ion channels by the serum- and glucocorticoid-inducible kinase SGK1. FASEB J 27: 3-12.
- Lamothe SM, Zhang S (2013) The Serum- and Glucocorticoid-inducible Kinase SGK1 and SGK3 Regulate hERG Channel Expression via Ubiquitin Ligase Nedd4-2 and GTPase Rab 11. J Biol Chem 288: 15075-15084.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.