IPL Treatment of Vascular and Pigmented Lesions in Clinical Practice: A Retrospective Case Series.
by Cristina Cabac*
Dermatologist, Alma Clinic, Clinical Moldova Alma Lasers, Moldova
*Corresponding author: Cristina Cabac, Dermatologist, Alma Clinic, Clinical Moldova Alma Lasers, Moldova
Received Date: 14 July 2025
Accepted Date: 19 July 2025
Published Date: 21 July 2025
Citation: Cabac C. (2025). IPL Treatment of Vascular and Pigmented Lesions in Clinical Practice: A Retrospective Case Series. Ann Case Report. 10: 2347. https://doi.org/10.29011/2574-7754.102347
Introduction
Intense Pulsed Light (IPL) technology has emerged over the past two decades as a versatile and non-ablative modality for the treatment of various dermatologic conditions, particularly benign vascular and pigmented lesions. Unlike laser systems, IPL emits a no coherent, polychromatic light spectrum, typically ranging from 400 to 1,200 nm, which can be tailored to specific chromophores such as melanin and hemoglobin through the application of cutoff filters and pulse configuration strategies. [1] This versatility allows IPL systems to target multiple skin components, facilitating the simultaneous treatment of multiple lesion types with minimal downtime and high patient acceptance [2,3].
The mechanism of action of IPL is grounded in the principle of selective photothermolysis, whereby specific wavelengths are absorbed by target chromophores-oxyhemoglobin, deoxyhemoglobin, or melanin-resulting in localized thermal injury while sparing adjacent tissues. [4] For vascular lesions, the primary targets are oxyhemoglobin and deoxyhemoglobin, with absorption peaks in the green-yellow and near-infrared ranges. Pulse duration, fluence, and filter selection are optimized to match the thermal relaxation times and absorption profiles of vessels of varying sizes and depths [5,6].
Clinically, IPL has demonstrated comparable efficacy to pulsed dye lasers (PDL) and other single-wavelength lasers in reducing facial telangiectasias, poikiloderma of Civatte, and erythema associated with rosacea, but with the added advantage of minimal purpura and broader treatment coverage. [1,4] For pigmented lesions such as lentigines, ephelides, melasma, and café-au-lait macules, IPL can selectively photocoagulate melanin-rich structures, particularly those located in the epidermis. Studies have shown that shorter cutoff filters (e.g., 515-560 nm) are most effective for superficial pigmentation, while longer wavelengths can be used to target deeper or dermal melanin deposits [2,4,7].
Histological analyses support the remodeling effects of IPL beyond pigment and vessel clearance, indicating neocollagenesis and dermal matrix reorganization in the context of photorejuvenation. [1,2] Such effects are mediated through mild thermal stimulation of fibroblasts and modulation of cytokine expression, including TGF-β1 and inhibition of matrix metalloproteinases [2].
The growing body of literature demonstrates that IPL is not only effective but also safe when appropriate patient selection, skin typing, and parameter adjustment are observed. Advances in IPL technology, such as optimized pulse shaping and real-time cooling systems, have further enhanced treatment tolerability and outcomes. [2,6] Moreover, comparative evaluations have concluded that IPL, when configured correctly, performs on par with established laser modalities in the management of both pigmentary and vascular dyschromias. This further supports the role of IPL as a first-line or complementary modality for patients with facial telangiectasia and pigmentation disorders, particularly those seeking minimal downtime and broad facial treatment coverage. However, there is little published data from routine clinical practice, where patients and methods may differ from those used in clinical trials. This case series report aims to describe our experience in treating vascular and pigmented lesions, with a particular focus on analyzing the methods used and the consecutive clinical outcomes. Such clinical data can enable doctors and patients to make more informed decisions about the available treatment options and their likely outcomes.
Materials and Methods
Study Design
This retrospective case series evaluated the clinical efficacy and safety of the Intense-Pulsed-Light Dye-VL applicator, used alone or in combination with other modalities, for the treatment of facial vascular lesions, pigmented lesions, and melasma.
Patients
A total of twenty-five patients (24 female, 1 male), mean age of 47.9 (range 29-73 years), Fitzpatrick skin types II-III, with 16 facial pigmented lesions, 7 vascular lesions, and 2 with melasma (Table 1) undergone treatment using Harmony XL Pro/Dye-VL (Alma Lasers, Israel) alone or in combination with other modalities. All patients were in good general health, with no significant pre-existing medical conditions or dermatologic disorders, and none were taking medications that could influence their skin condition.
|
Characteristic |
Value |
|
|
Age (years) Avg±SD |
47.9±16.3 |
|
|
Gender |
F |
24 |
|
M |
1 |
|
|
Skin Type |
II |
20 |
|
III |
5 |
|
|
Indication (n) |
Pigmented Lesions |
16 |
|
Vascular Lesions |
7 |
|
|
Melasma |
2 |
|
Table 1: Patient Demographic and Clinical Characteristics.
Treatment Procedures
Treatment employed Dye-VL alone or in combination with another modality according to the specific skin condition. Combinations included either Harmony XL Pro 1064 nm Nd:YAG laser or Alma Hybrid/Softlift 1570nm laser (Alma lasers, Israel) as detailed in Table 2.
Table 2: Treatment Parameters Used.
Treatment outcomes were evaluated using standardized pre- and post-treatment digital photographs taken at baseline and at three months following the last treatment session. Three independent, blinded physicians assessed the results using a 4-point clearance scale (1 = 0-25% clearance, 2 = 26-50%, 3 = 51-75%, 4 = 76-100%). The mean percentage clearance score was calculated for each case. Side effects were documented at each visit.
To explore possible associations between treatment response and patient or procedural variables, statistical analyses were performed. Pearson correlation coefficients were calculated to assess the relationships between lesion clearance and patient age, skin type, and the number of treatment sessions. Additionally, a one-way ANOVA was conducted to assess differences in clearance outcomes between the three treatment indications (pigmented lesions, vascular lesions, and melasma). A p-value < 0.05 was considered statistically significant.
Results
Patients received one to five treatments, those who underwent more than one treatment session, consecutive treatments were conducted at intervals of 2-5 weeks. Blinded comparison of photographs taken before the treatment vs. 3 months following the last treatment session by three independent assessors revealed that the mean lesion clearance score across all 25 patients was 3.2 ± 0.58, indicating more than 75% clearance of the lesions. Vascular lesions showed the highest individual clearance scores, with some patients achieving 76-100% clearance (score = 4) after a single session. Representative before-and-after pictures are shown in (Figures 1-3). Statistical analysis revealed no significant correlations between lesion clearance and age (r = 0.31, p = 0.13), skin type (r = 0.30, p = 0.15), or number of treatment sessions (r = –0.21, p = 0.31). Likewise, no significant differences in clearance scores were found between the three indications (p = 0.80, one-way ANOVA), suggesting consistent efficacy across conditions. Edema was reported in four patients (16%), all of whom recovered without any intervention. No other adverse effects, such as post-inflammatory hyperpigmentation or scarring, were observed.


Figure 1: Pigmented lesions (A) before and (B) 3 months following a single Dye-VL treatment.

Figure 2: Vascular lesions (A) before and (B) 3 months following a single Dye-VL treatment.
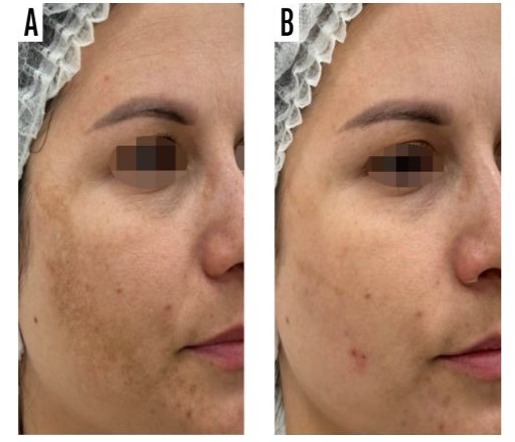
Figure 3: Melasma (A) before and (B) 3 months following 3 Dye-VL treatment sessions.
Discussion
This retrospective case series evaluated the safety and efficacy of intense pulsed light (IPL) using the Harmony XL Pro Dye-VL applicator, with or without combination treatment, for vascular and pigmented facial lesions. Our findings support the high effectiveness of Dye-VL IPL in improving lesion appearance, with a mean blinded clearance score of 3.2 ± 0.58 (on a 4-point scale) and no significant adverse events. The observed outcomes are consistent with the evolving clinical literature on IPL over the past two decades. Goldberg [3] provided one of the earliest comprehensive reviews of vascular and pigmented lesion management with light-based devices, highlighting the role of IPL as a versatile adjunct to laser therapy due to its polychromatic light spectrum and broader absorption targeting, though with less chromophore specificity compared to devices like KTP, PDL, or Nd:YAG. Building on this, Campolmi et al. [8] published one of the earliest large-scale retrospective evaluations of IPL efficacy in treating non-aesthetic facial and neck vascular lesions. Their study of 85 patients demonstrated an 81% rate of marked improvement in rosacea and poikiloderma lesions, and 77% for pigmented lesions, with minimal side effects. Their protocol involved the use of cutoff filters between 500-550 nm with fluences up to 25 J/cm², and treatment intervals of 3 weeks-closely aligning with the parameters used in the present study. Soon after, Rusciani et al. [9] reported a 7-year experience with IPL for poikiloderma of Civatte in 175 patients. Using similar cutoffs (515–590 nm) and fluences (32-38 J/cm²), they achieved over 75% clearance in 81% of cases. Notably, they documented the effectiveness of IPL in addressing both vascular and pigmented components of lesions, confirming the dual-targeting utility of the modality. In parallel, Hague and Lanigan [10] provided real-world data from routine dermatological practice using various laser modalities, including Q-switched and Er:YAG systems, for pigmentary lesions. Their results, while derived from different energy sources, reinforce the principle that light-based interventions are highly effective for congenital and acquired pigmented conditions. Importantly, 75% of their patients achieved favorable outcomes, aligning well with the clearance levels observed in our cohort.
González-Rodríguez and Lorente-Gual [4] contributed a detailed review of IPL technology and its clinical applications. They highlighted the mechanism of selective photothermolysis, emphasized the role of chromophore-matched cutoff filters, and discussed IPL's role in treating vascular and pigmented lesions, including rosacea and lentigines, with results comparable to those achieved by laser systems when parameters are appropriately optimized.Most recently, Avdulaj [11] presented a large retrospective study of 100 patients treated with a narrowband IPL (450-600 nm) featuring Advanced Fluorescence Technology (AFT). The study reported high GAIS scores (8.02 for vascular lesions and 8.14 for pigmented lesions) and a strong correlation with patient satisfaction, mirroring our own findings. Importantly, no pain was reported and only two mild adverse events were observed, highlighting the excellent safety profile of IPL in real-world use.
In comparison to earlier IPL studies, such as that by Maruyama, [7] that focused on hand rejuvenation, the present study shows that facial lesions may respond more rapidly and robustly, likely due to anatomical and physiological differences. Maruyama noted that heavily pigmented lentigines often required up to two treatments for visible improvement, with longer downtime and occasional PIH. In contrast, our study recorded significant improvements after just one session in several cases, with only transient edema as the primary side effect.
Urdiales-Gálvez et al. [5] reported a weighted mean clearance index of 92.4% for facial vascular lesions treated with a narrowband Dye-VL handpiece, and noted excellent or very good patient satisfaction in all cases. In our series, similarly high clearance rates were achieved for vascular lesions after a single treatment, suggesting comparable efficacy with fewer sessions. Unlike traditional PDL-based treatments which often require extended regimens and carry risks of purpura, IPL demonstrated excellent tolerability, as also highlighted in Fischer et al. [12] and Goldberg, [3] with no significant adverse events reported in our cohort.
Together, these studies illustrate the trajectory of IPL research from early clinical feasibility to large-scale adoption. The present case series adds to this growing body of evidence by demonstrating that IPL using the Harmony XL Pro Dye-VL applicator, with or without combination treatment, is highly effective and well tolerated in daily clinical practice.
Limitations
This study is limited by its retrospective design, small sample size, and the absence of objective quantitative assessment tools. Moreover, the variability introduced by using combination modalities in some cases limits the ability to isolate the effect of the Dye-VL applicator alone. However, this reflects real-world clinical workflows where individualized treatment plans are common. Future prospective studies with standardized assessment tools and comparator arms are warranted.
Conclusion
In summary, IPL using the Harmony XL Pro Dye-VL applicator demonstrates high clinical efficacy and safety for the treatment of both vascular and pigmented lesions. The consistency of outcomes across indication types, patient demographics, and treatment modalities underscores the versatility of IPL in aesthetic dermatology. These findings align with the clinical evolution of IPL over the past two decades and support its continued integration into evidence-based practice.
References
- Goldman MP, Weiss RA, Weiss MA. (2025). Intense pulsed light as a nonablative approach to photoaging. Dermatologic Surg. 31: 1179-1187.
- Li D, Lin S, Bin Cheng B. (2016). Intense Pulsed Light: From the Past to the Future. Photomed. Laser Surg. 34: 435-447.
- Goldberg DJ. (2006). Laser removal of pigmented and vascular lesions. J. Cosmet. Dermatol. 5: 204-209.
- González-Rodríguez AJ, Lorente-Gual R. (2015). Indicaciones actuales y nuevas aplicaciones de los sistemas de luz pulsada intensa. Actas Dermosifiliogr. 106: 350-364.
- Urdiales-Gálvez F, Castellano-Miralla A. (2023). Effectiveness and safety of a narrow band spectrum intense pulsed-light dye with long pulse Nd:YAG laser for treating facial vascular lesions. J. Cosmet. Dermatol. 22: 8-15.
- Ross EV, Smirnov M, Pankratov M, Altshuler G. (2005). Intense pulsed light and laser treatment of facial telangiectasias and dyspigmentation: Some theoretical and practical comparisons. Dermatologic Surg. 31: 1188-1198.
- Maruyama S. (2016). Hand rejuvenation using standard Intense Pulsed Light (IPL) in Asian patients. Laser Ther. 25: 43-54.
- Campolmi P. (2011). Intense pulsed light in the treatment of non-aesthetic facial and neck vascular lesions: Report of 85 cases. J. Eur. Acad. Dermatology Venereol. 25: 68-73.
- Rusciani A, Motta A, Fino P, Menichini G. (2008). Treatment of poikiloderma of Civatte using intense pulsed light source: 7 Years of experience. Dermatologic Surg. 34: 314-319.
- Hague JS, Lanigan SW. (2008). Laser treatment of pigmented lesions in clinical practice: A retrospective case series and patient satisfaction survey. Clin. Exp. Dermatol. 33: 139-141.
- Arminda A. (2024). Intense Pulsed Light (IPL) for the treatment of vascular and pigmented lesions. J. Cosmet. Dermatol. 23: 1-6.
- Nestor MS, Fischer D, Arnold D. (2020). Randomized, Investigator-Blinded Study to Compare the Efficacy and Tolerance of a 650-microsecond, 1064-nm YAG Laser to a 308-nm Excimer Laser for the Treatment of Mild to Moderate Psoriasis Vulgaris. J. Drugs Dermatol. 19: 176-183.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.