Intimate Brightening With a Soothing and Regenerative Action Serum: Clinical Results with ProGene® Advanced Intimate
by Jocimara Gonçalves
Clínica de Estética e Saúde: Método Célula, Vitória – ES, Brazil.
*Corresponding Author: Jocimara Gonçalves, Clínica de Estética e Saúde: Método Célula, Vitória – ES, Brazil.
Received Date: 08 July, 2025
Accepted Date: 22 July, 2025
Published Date: 25 July, 2025
Citation: Gonçalves J (2025) Intimate Brightening with a Soothing and Regenerative Action Serum: Clinical Results with ProGene® Advanced Intimate. Clin Exp Dermatol Ther 10: 238. https://doi.org/10.29011/2575-8268.100238
Abstract
Background: Hyperpigmentation of intimate areas is a prevalent aesthetic concern, particularly among women, often associated with significant psychological distress. Common contributing factors include chronic friction, inflammation, depilation, hormonal fluctuations, and higher phototypes. Aim: To evaluate the clinical effects of the ProGene® Advanced Intimate Protocol, a topical formulation with depigmenting, soothing, and regenerative action, on intimate hyperpigmentation in five patients. Methods: Five adult patients with inguinal, axillary, and perianal hyperpigmentation underwent a combination of in-office treatment sessions and at-home application of a dermocosmetic serum over 30 to 60 days. Improvement was assessed subjectively and photographically. Results: All patients experienced visible improvement in pigmentation, ranging from 25% to over 75%, along with enhanced skin texture and hydration. No adverse reactions were reported. Patient satisfaction was high, with reported improvement in self-esteem and confidence in intimate settings. Conclusion: The ProGene® Advanced Intimate Protocol appears to be a safe, well-tolerated, and effective approach to managing hyperpigmentation in sensitive areas. However, larger controlled studies with objective measures are needed to confirm these preliminary findings.
Keywords: Intimate hyperpigmentation; Skin lightening; Depigmentation; Sensitive areas; Niacinamide; Arbutin; ProGene®
Introduction
Hyperpigmentation of intimate areas, such as the groin, armpits, and perianal region, is a highly prevalent aesthetic dermatological condition, primarily affecting women, though incidence among men is increasing. This pigmentation results from multifactorial causes including chronic friction, recurrent inflammation, aggressive depilation, hormonal changes, obesity, insulin resistance, and genetic predisposition [1,2]. Though generally benign, it has significant psychosocial impacts, affecting self-esteem and well-being [3].
Despite growing demand for effective solutions, standardized aesthetic protocols ensuring both clinical efficacy and safety for these sensitive areas remain scarce. These regions are anatomically distinct, with thinner epidermis, increased vascularization, higher susceptibility to irritation, and a specific physiological pH [4]. Additionally, male patients often face social stigma, contributing to underreporting and undertreatment [5,6].
Aesthetic dermatology has increasingly focused on less aggressive formulations that combine depigmenting effects with soothing and regenerative properties. These aim to modulate melanocyte activity and inflammatory microenvironments. Actives such as kojic acid, niacinamide, panthenol, and botanical extracts are being studied for their safe and well-tolerated brightening action [7-9].
Gonçalves [10], in a case study on facial melasma, showed that actives with anti-inflammatory and soothing action can produce significant results without major adverse effects, even on sensitive skin. The therapeutic approach is based on “calming” the melanocyte and restoring skin homeostasis, avoiding rebound hyperpigmentation commonly caused by aggressive treatments [10].
In this context, the development of depigmenting solutions compatible with intimate physiology becomes essential. The ProGene® Advanced Intimate Protocol emerges as a promising alternative, combining synergistic actives with depigmenting, soothing, and regenerative action, in a formula ensuring proper pH, good skin penetration, and high stability. The serum contains Aqua (q.s.p.), Glycerin (5%), Propylene Glycol (5%), EDTA (0.2%), Nano Retinol (0.3%), Cetearyl Alcohol (1-5%), Arbutin (3%), Protag CalmDerma Complex® (3%), Hyaluronic Acid (2%), Niacinamide (6%), Squalane (5%), Isopropyl Myristate (5%).
This article aims to present five clinical case reports demonstrating the efficacy and safety of the ProGene® Protocol in patients with intimate hyperpigmentation. The intention is to contribute to the scientific understanding of brightening delicate areas, emphasizing individualized and skin-compatible approaches. The active ingredient applied in the clinic, in association with the dermo-cosmetic serum of the skincare protocol, was initially developed in a manipulated formulation, based on strict safety criteria for sensitive areas. It is now available in an industrialized version, with standardized production and improved quality control. The formula has excellent clinical performance, with visible results in lightening intimate hyperchromia and high dermocompatibility. Its application is carried out exclusively by trained professionals, with the patient's informed consent and for aesthetic purposes.
Case Report
All participants signed a Free and Informed Consent Form, authorizing the proposed aesthetic treatment, the use of clinical data and the publication of images before and after the procedure, exclusively for scientific and educational purposes, in accordance with the ethical guidelines of CNS Resolution 466/12 and the principles of the Declaration of Helsinki.
Case Report 1 - Whitening of the Perianal Region in a Male Patient
A 42-year-old male patient, phototype III, presented with an aesthetic complaint of hyperchromia in the perianal region, with a history of progressive darkening related to local friction and hair removal (Figure 1A). She reported a negative impact on her self-esteem, discomfort in intimate situations and wearing swimwear. The patient had previously undergone laser treatment for the same concern, with unsatisfactory results. He had been experiencing the darkening for over one year. During the protocol, he followed a structured homecare routine: In the morning, cleansing with soap, micellar water, and application of zinc-based water paste; at night, repeating the cleansing steps and applying the ProGene® brightening serum. He received instructions on proper intimate hygiene, daily sun protection, and avoiding friction and tight clothing. The therapeutic protocol consisted of two clinical sessions carried out in a controlled environment, with application of the ProGene® Advanced Intimate Protocol, followed by daily use of a homecare formulation containing the same whitening and regenerating active ingredients. The patient was instructed on photoprotection, intimate hygiene and continuity of homecare during the interval between sessions. After 40 days of using the protocol, there was a significant improvement in skin tone uniformity, with an estimated 75% lightening of the treated area (Figure 1B). The patient also showed improved skin texture, increased hydration and no adverse events such as erythema, burning or flaking. In subjective terms, he reported increased self-esteem, greater personal security and a return to well-being in intimate situations.
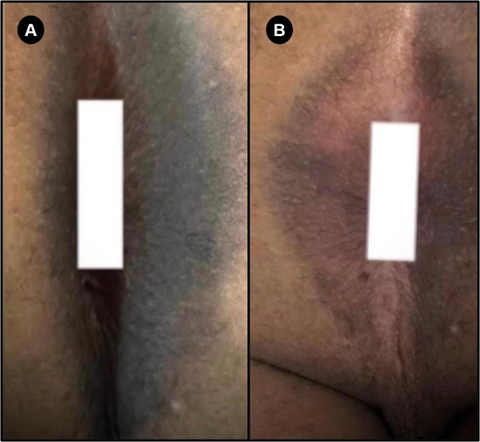
Figure 1: Perianal region whitening area; A) Perianal region before using the ProGene® protocol; B) Perianal region after using the ProGene® protocol.
Source: author (2025).
Case Report 2 - Whitening of the Axillary and Perianal Region in a Female Patient
A 42-year-old female patient, phototype VI (black skin), presented with an aesthetic complaint of hyperchromia in the armpits (Figure 2A) and perianal region (Figure 2C), with a history of darkening related to friction and depilation. She reported low self-esteem and discomfort during intimate moments, affecting her social and emotional life. The protocol consisted of two clinical sessions, with application of the ProGene® Advanced Intimate Protocol, followed by daily use of a homecare product. The patient was instructed to avoid friction and to use sunscreen daily. After 45 days, an estimated 75% lightening was observed, with improvement in skin firmness and texture (Figure 2B and D). In addition to the axillary and perianal areas, the patient presented hyperpigmentation in the inner thigh region. During the protocol, she reported a mild stinging sensation in that area, attributed to friction between the thighs, this resolved spontaneously without intervention. Her homecare routine included morning and evening application of soap, micellar water, zinc-based water paste, and the ProGene® serum. She adhered well to all recommendations. No significant adverse reactions were noticed. The patient reported increased self-confidence and satisfaction with the results, feeling safer in intimate situations.
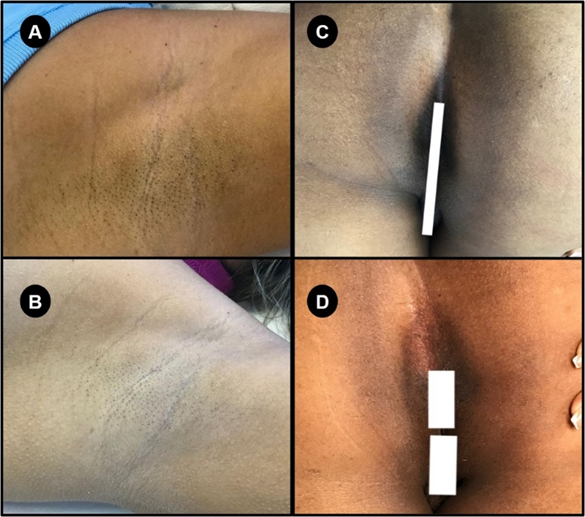
Figure 2: Axillary (A e B) and Perianal (C e D) Bleaching Axillary region, before; A) and after B) use of the ProGene® protocol; Perianal region before C) and after D) use of the ProGene® protocol.
Source: author (2025).
Case Report 3-Whitening of the Inguinal Region in a Female Patient
A 40-year-old female patient, phototype II, complained of hyperchromia in her groin (Figure 3A), with a history of darkening due to friction and hair removal. She reported an impact on her self-esteem and discomfort during intimate moments, avoiding swimwear and social situations. The treatment included four clinical sessions with the ProGene® Advanced Intimate Protocol and the use of a homecare product. The patient followed guidelines for correct hygiene and sun protection, avoiding friction. After 60 days of treatment, an estimated 50% lightening was observed, as well as improvements in skin texture and hydration (Figure 3B).
The pigmentation had been present for over a year and was associated with friction and depilation. The patient had not undergone any previous treatment. The protocol consisted of four clinical sessions with 15-day intervals. She strictly followed homecare twice a day, using soap, micellar water, water paste, and serum, which contributed to improved hydration and firmness. She reported that the hyperpigmentation negatively impacted her confidence, especially in social settings, and avoided swimwear. No adverse effects were noted. No adverse reactions were reported. The patient noticed a significant increase in self-esteem and confidence in intimate situations.
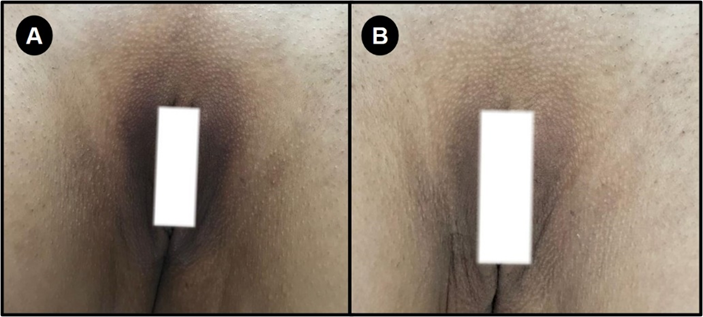
Figure 3: Whitening of the inguinal region; Inguinal region, before A) and after B) use of the ProGene® protocol; Source: author (2025).
Case Report 4 - Whitening of the Axillary Region in a Female Patient
A 33-year-old female patient, phototype I according to the Fitzpatrick classification, reported hyperpigmentation in her armpits for over a year (Figure 4A). She reported that factors such as friction, hair removal and the use of aerosol products had contributed to the appearance and worsening of the stain. She has no history of comorbidities such as obesity, diabetes or dermatitis, and has had no previous medical or aesthetic treatments in the area. The patient reported that the spot had a negative impact on her self-esteem, causing discomfort in intimate moments and social withdrawal. Three clinical sessions were carried out with an interval of seven days between them. The protocol was adapted to her case, using products at home twice a day, including soap, micellar water, serum and water paste. Initially, the products were only applied in the evening, but were later included in the morning. Guidance was given on proper hygiene of the area, the use of sunscreen and avoiding friction and tight clothing. The patient reported lightening of between 50% and 75% of the spot after treatment, as well as improved hydration and skin texture (Figure 4B). No adverse effects were experienced. No adverse reactions were reported during or after the sessions.
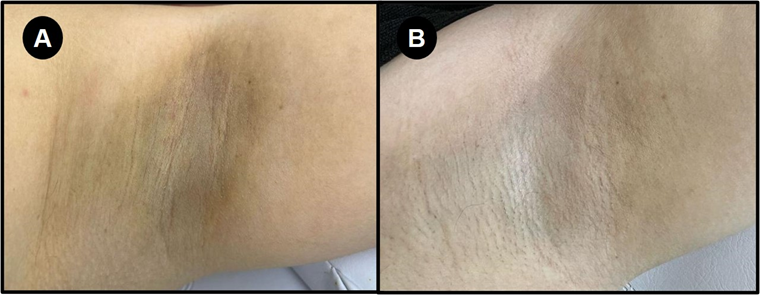
Figure 4: Whitening of the Axillary Region; Legend: Axillary region, before A) and after B) use of the ProGene® protocol; Source: author (2025).
Case Report 5 - Whitening of the Inguinal Region in a Female Patient
A 47-year-old female patient, phototype IV according to the Fitzpatrick classification, had hyperpigmentation in the groin area for over a year (Figure 5A). She reports that wearing jeans every day, combined with friction and hair removal, contributed to the appearance of the spot. She has no comorbidities and has never had previous aesthetic or medical treatment on the affected area. The patient says that the stain negatively affects her self-esteem and causes discomfort during intimate moments. Two clinical sessions were carried out with an interval of 30 days between them. The protocol had no specific adaptations for the case. In addition, the patient was prescribed to use products at home on a daily basis, with a routine that included liquid soap for hygiene, application of mineral water to the area, followed by whitening cream combined with water paste and finishing with the Scan Care product. The guidelines provided for care at home included proper hygiene of the area, use of sunscreen and avoidance of friction and tight clothing. The patient reported lightening of between 25% and 50% of the spot after starting treatment, as well as an improvement in skin firmness and texture (Figure 5B).
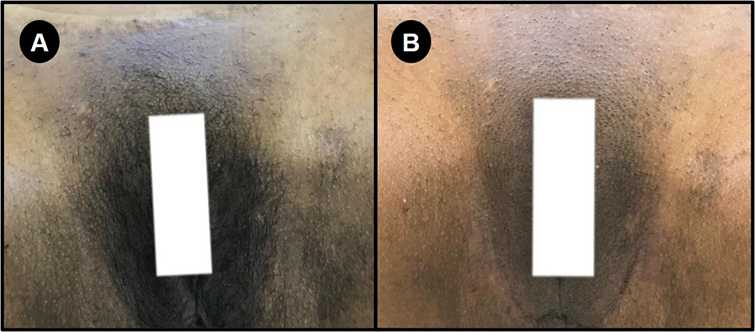
Figure 5: Whitening of the inguinal region Legend: Inguinal region, before; A) and after; B) use of the ProGene® protocol. Source: author (2025).
The following table 1 summarizes the key clinical data from the five patients treated with the ProGene® Advanced Intimate Protocol, including age, phototype, treated area, number of sessions, treatment duration, estimated improvement, adverse effects, and reported subjective outcomes. This overview facilitates the visualization of response patterns and highlights the consistency of the observed results across different clinical profiles.
|
Case |
Age / Sex |
Phototype |
Treated Area |
No. of Sessions |
Treatment Duration |
Estimated Improvement |
Adverse Effects |
|
1 |
42 / Male |
III |
Perianal |
2 |
40 days |
>75% |
None |
|
2 |
42 / Female |
VI |
Axillary and Perianal |
2 |
45 days |
>75% |
None |
|
3 |
40 / Female |
II |
Inguinal |
4 |
60 days |
~50% |
None |
|
4 |
33 / Female |
I |
Axillary |
3 |
~21 days |
50-75% |
None |
|
5 |
47 / Female |
IV |
Inguinal |
2 |
60 days |
25-50% |
None |
Table 1: Summary of Clinical Cases Treated with the ProGene® Advanced Intimate Protocol Source: author (2025).
Discussion
Hyperchromia of intimate areas, although not a physical health risk, has a significant impact on patients' self-esteem, psychological well-being and quality of life. Areas such as the groin, perineum and armpits are particularly susceptible to post-inflammatory hyperpigmentation due to constant exposure to friction, hair removal, humidity and hormonal changes, especially in individuals with higher phototypes [1,3].
The results obtained in the five clinical cases presented demonstrate a significant improvement in skin color, texture and hydration after the application of the ProGene® Advanced Intimate Protocol. The efficacy observed is in line with scientific evidence pointing to the superiority of combined therapies containing depigmenting, anti-inflammatory and regenerating agents for the treatment of hyperchromias in sensitive areas [2]. The strategy of combining clinical sessions with homecare reinforces the importance of therapeutic continuity, promoting sustainable results and reducing the risk of rebound hyperpigmentation - especially common when using more aggressive acids or invasive methods in delicate areas [4]. In this sense, niacinamide, kojic acid, panthenol and botanical extracts such as chamomile and calendula have a favorable safety profile and mechanisms of action that involve inhibiting tyrosinase, controlling inflammation and modulating skin barrier function [7] Rodrigues et al., 2021). Another fundamental aspect concerns the tolerability of the protocol. None of the patients reported adverse effects such as burning, flaking or erythema, which indicates adequate compatibility of the formulation with the pH and anatomical characteristics of the treated regions. This is essential, considering that the skin of intimate areas is more permeable, has a higher density of nerve endings and is subject to microbiological imbalances when exposed to unsuitable products [4].
In addition to the objective clinical improvement, both patients reported a positive impact on their self-perception and intimate life, reinforcing the importance of therapeutic approaches that consider not only the physical aspects, but also the emotional ones. The literature already recognizes the association between visible pigmentary disorders and anxiety, depression and social withdrawal, especially in populations with greater aesthetic concern or body exposure [11]. The study by Gonçalves [9], which proposes a treatment for melasma based on soothing and regenerating active ingredients, provides an important conceptual reference for this study. As with melasma, intimate hyperchromia requires approaches that promote melanocyte rebalancing, restoration of the skin barrier and sustained reduction of inflammation, preferably without causing additional aggression to the skin.
Although the results presented are promising, there is a need for more extensive and controlled clinical studies, with histological evaluation and long-term follow-up, to validate the efficacy of the ProGene® Protocol in different population profiles. Even so, the cases described reinforce the relevance of innovative, personalized and dermocompatible therapeutic strategies in the management of intimate hyperpigmentation.
Conclusion
The case reports presented demonstrate that the ProGene® Advanced Intimate Protocol is an effective, safe and well-tolerated approach to managing hyperpigmentation in intimate regions, promoting significant skin lightening, improved texture and hydration, as well as a positive impact on patients' self-esteem and quality of life. The absence of adverse effects and good adherence to treatment reinforce the formulation's dermocompatibility, especially in higher phototypes. Although the results are promising, controlled clinical studies with a larger sample size and long-term follow-up are needed to validate and expand the evidence on its therapeutic efficacy.
Conflict of Interest
The author declares a potential conflict of interest regarding the formulation and application of the ProGene® Advanced Intimate Protocol, as the product was developed and is currently used within her clinical practice. There is no financial sponsorship from third parties for this study. All clinical cases were conducted independently and without funding from commercial entities.
References
- Taylor SC, Cook-Bolden F, Rahman Z, Strachan D (2002) Acne vulgaris in skin of color. J Am Acad Dermatol 46: S98-106.
- Sarkar R, Arora P, Garg KV (2013) Cosmeceuticals for hyperpigmentation: What is available? J Cutan Aesthet Surg 6: 4-11.
- Handel AC, Miot LDB, Miot HA (2014) Melasma: a clinical and epidemiological review. An Bras Dermatol 89: 771-782.
- Draelos ZD (1997) Sensitive skin: perceptions, evaluation, and treatment. Am J Contact Dermat 8: 67-78.
- Ginsberg BA (2017) Dermatologic care of the transgender patient. International journal of women's dermatology Int J Womens Dermatol 3: 65-67.
- Butler W, Cai CR, Carswell JM, Huang JT (2024) Dermatologic needs of transgender and gender diverse youth: A retrospective cohort study. Pediatr Dermatol 41: 677-679.
- Grimes PE (2009) Management of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg 28: 77-85.
- Vashi NA, Wirya SA, Inyang M, Kundu RV (2017) Facial hyperpigmentation in skin of color: special considerations and treatment. Am J Clin Dermatol 18: 215-230.
- Chatrath S, Bradley L, Kentosh J (2023) Dermatologic conditions in skin of color compared to white patients: similarities, differences, and special considerations. Arch Dermatol Res 315: 1089-1097.
- Gonçalves JC (2020) Discovery under Calming Assets in Melasma: A Case Report. Clin Exp Dermatol Ther 5: 168.
- Misery L, Seneschal J, Reguiai Z, Brenaut E, Le Garrec R, et al. (2018) Sensitive skin in the genital area. J Eur Acad Dermatol Venereol 32: 791-796.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.