Integration of Skin Boosters into Rejuvenation Surgery: Preconditioning
by Ji Yeoun Shin1, Taek-Kyun Kim2*
1HEV Dermatology Clinic, 6F, 384, Ieum-daero, Seo-gu, Incheon, Republic of Korea
2THE PLUS Plastic Surgery, 9 Garosu-gil, Gangnam-gu, Seoul, Republic of Korea
*Corresponding author: Taek-Kyun Kim, THE PLUS Plastic Surgery, 9 Garosu-gil, Gangnam-gu, Seoul, 06035, Republic of Korea
Received Date: 12 May 2025
Accepted Date: 19 May 2025
Published Date: 21 May 2025
Citation: Shin JY, Kim TK (2025) Integration of Skin Boosters into Rejuvenation Surgery: Preconditioning. J Surg 10: 11326 https://doi.org/10.29011/2575-9760.011326
Abstract
Background: As aesthetic medicine evolves, the integration of minimally invasive therapies into traditional surgical workflows is gaining prominence. Rejuvenation surgery effectively addresses structural signs of aging, such as skin laxity and volume loss, but often neglects intrinsic skin quality factors like hydration, elasticity, and dermal architecture.
Methods: Skin boosters, either topical or injectable agents including hyaluronic acid, polynucleotides, and polylactic acid, can be injected prior to rejuvenation surgery such as facelifts and blepharoplasties to optimize the skin’s microenvironment before surgical trauma.
Results: Skin boosters may enhance healing, reduce postoperative complications, and improve overall aesthetic outcomes by offering bioactive stimulation that improves extracellular matrix integrity, promotes collagen synthesis, enhances hydration, and supports tissue regeneration.
Conclusions: This article suggests the concept and protocol of skin preconditioning with skin boosters prior to rejuvenation procedures.
Key words: Skin boosters, Rejuvenation Surgery, Preconditioning
Introduction
Rejuvenation surgery has long been the gold standard in addressing visible signs of aging, including sagging skin, wrinkles, and volume loss. However, with the growing preference for minimally invasive procedures, the demand for non-surgical adjuncts to enhance surgical outcomes has increased [1]. Skin boosters, a subset of topical and injectable treatments, have gained traction to improve skin hydration and elasticity through the direct action on skin itself. While rejuvenation surgeries target structural issues such as skin laxity and wrinkle, they do not address underlying skin quality issues including dehydration and texture. Skin boosters, encompassing hyaluronic acid, polynucleotide, poly lactic acid, etc. by improving the intrinsic properties of the skin, have the potential to complement these surgical interventions and enhance both their immediate and long-term aesthetic results [2]. This article aims to investigate the feasibility of integrating skin boosters into rejuvenation surgery, with a specific focus on the underlying mechanisms and clinical outcomes.
Aging of Skin (Figure 1)
The skin, with an approximate surface area of 2 m² and accounting for one-sixth of an adult’s body weight, is the largest organ in the human body [3]. It comprises a highly organized microanatomical structure composed of various cell types, including keratinocytes, fibroblasts, melanocytes, Merkel cells, and immune cells such as mast cells, mononuclear cells, and Langerhans cells. In addition to these cellular components, it contains appendages like sweat glands and hair follicles, along with intricate vascular and neural networks. The skin’s resilience and elasticity are largely dependent on connective tissues rich in Extracellular Matrix (ECM).
A critical anatomical interface within the skin is the Dermal Epidermal Junction (DEJ), which not only anchors the epidermis to the dermis but also facilitates biochemical exchange and provides a barrier against external insults. With aging, the epidermis becomes thinner, and the DEJ flattens significantly, resulting in a diminished surface area. This structural alteration compromises the mechanical integrity of the skin and reduces nutrient transfer between layers, contributing to increased fragility and susceptibility to injury. Agerelated epidermal atrophy is accompanied by a marked decline in the proliferative capacity of basal keratinocytes, leading to delayed wound healing and impaired desquamation. Studies have shown that the epidermal turnover rate in individuals in their 80s is reduced by at least 30% compared to those in their 30s [4]. Moreover, aged individuals require substantially more time to reepithelialize after resurfacing procedures, highlighting the clinical relevance of epidermal regeneration.
The dermis also undergoes pronounced changes with aging. It becomes relatively acellular and avascular, with a decline in fibroblasts, mast cells, and vascular structures. The reduction in hyaluronic acid and glycosaminoglycan content contributes to a loss of dermal turgor and hydration. Simultaneously, the degradation and disorganization of collagen and elastin fibers within the ECM lead to decreased tensile strength and wrinkle formation. Cellular senescence further exacerbates tissue aging through the SenescenceAssociated Secretory Phenotype (SASP), characterized by the release of pro-inflammatory cytokines, chemokines, and proteases that promote chronic low-grade inflammation. The rationale for identification and validation of a new class of drugs termed senolytics, which selectively kill senescent cells can be described [5]. Telomeres are nucleoprotein structures at chromosome ends that play a crucial role in protecting chromosomes from degradation, fusion, and erroneous recombination [6]. Telomere shortening, driven by oxidative stress and environmental insults, is also implicated in cellular aging. While the telomerase enzyme is present in basal keratinocytes, it is largely absent in dermal fibroblasts, contributing to limited regenerative capacity in the dermis. To counteract these multifactorial aging processes, skin booster therapies have emerged as a promising modality along with rejuvenation surgery.
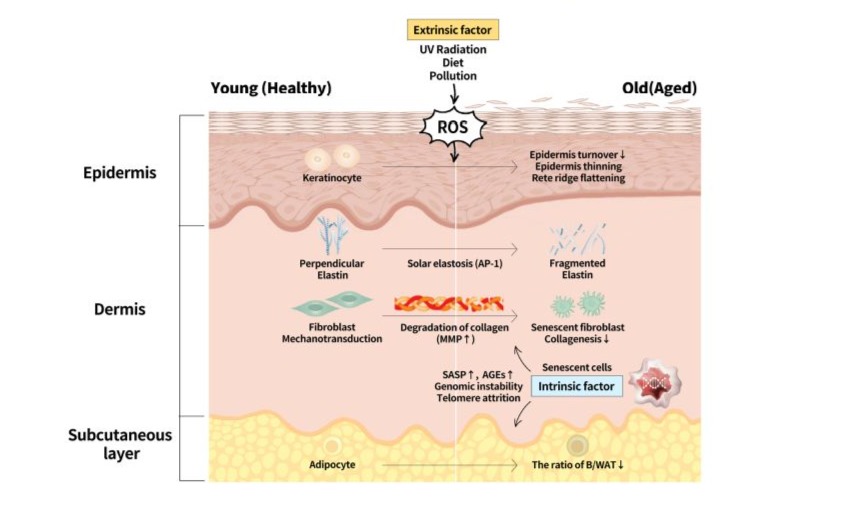
Figure 1: Aging process of skin with comparison between the young and the old. Senescence-Associated Secretory Phenotype (SASP), Advanced Glycation End-products (AGEs), B/WAT (Brown to White Adipose Tissue).
Methods
Mechanisms of Skin Boosters (Figure 2)
Skin boosters, through their ability to improve hydration, elasticity, and dermal architecture, represent a valuable intervention in aesthetic dermatology and plastic surgery for managing aged skin. Skin boosters contain a variety of active ingredients and can be categorized into two types: topical products intended for external application and injectable formulations. Topical agents such as alpha-hydroxy acids, Trichloroacetic Acid (TCA), ascorbic acids are used to accelerate keratinocyte proliferation, desquamation and activation of fibroblast via IL-1 secretion or to increase mRNA expression of the procollagen gene. Additionally, antioxidant compounds-including vitamin C, vitamin E, glutathione etc.are employed to neutralize Reactive Oxygen Species (ROS) and reduce oxidative damage. Injectable agents-including Polylactic Acid (PLA), Polynucleotide (PN), Polydioxanone (PDO), Hyaluroic acid (HA), Calcium hydroxyapatite (CaHA), Polycaprolactone (PCL), Acellular Dermal Matrix (ADM)- are used to an integrated, multilayer-targeted therapeutic approach is essential for effective skin rejuvenation. This includes restoring the epidermal barrier, attenuating inflammation, combating oxidative stress and Advanced Glycation End-products (AGEs), preserving telomere length, improving ECM integrity. Notably, hyaluronic acid-based injectables have been shown to enhance Adipose-derived Stem Cell (ASC) proliferation and support adipose tissue remodeling, offering additional benefits for dermal rejuvenation [7].
These bio-stimulating substances work through hydration, collagen stimulation, extracellular matrix remodeling, tissue regeneration and wound healing.
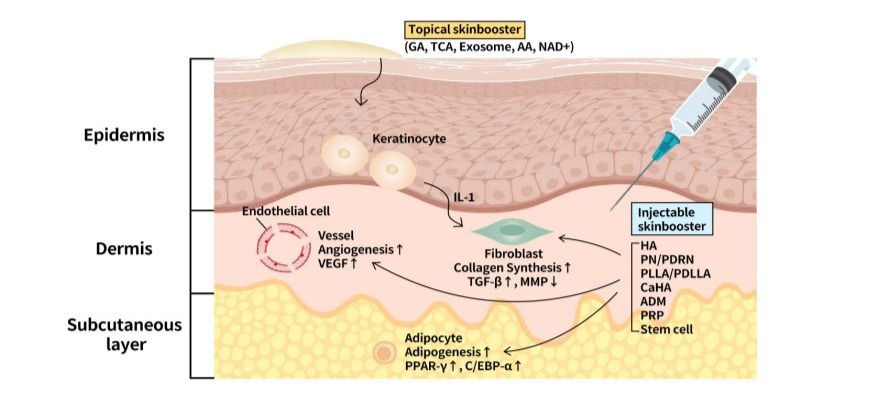
Figure 2: The mechanism how skin boosters work on skin. Collagen stimulation, extracellular matrix remodeling, tissue regeneration and wound healing.
Results
Collagen Stimulation
Beyond hydration, skin boosters stimulate fibroblast activity, leading to increased production of collagen and elastin-two fundamental proteins responsible for maintaining the structural integrity and elasticity of skin. The presence of Hyaluronic Acid (HA) and other bioactive molecules within skin boosters acts as a signaling mechanism, activating fibroblasts through receptormediated pathways such as CD44 and TGF-β. This stimulation enhances collagen types I and III synthesis, reinforcing the dermal framework and increasing skin density [8,9]. Elastin production also improves, contributing to skin’s ability to stretch and recoil, which is essential for resisting gravitational sagging. Over time, consistent fibroblast activation through skin boosters results in thicker, firmer, and more resilient skin that is better equipped to withstand mechanical stress and age-related deterioration.
Extracellular Matrix Remodeling
The Extracellular Matrix (ECM) serves as the structural scaffold, comprising collagen, elastin, Glycosaminoglycans (GAGs), and other essential macromolecules in skin. As fibroblasts synthesize new collagen in response to skin boosters, the ECM undergoes significant remodeling. This process involves the reorganization of collagen fibrils, improved alignment of elastin fibers, and increased deposition of GAGs such as HA and dermatan sulfate. The result is a denser and more structured dermal layer, leading to enhanced skin firmness, elasticity, and texture. In addition, ECM remodeling reduces the appearance of atrophic scars and fine lines by filling in structural gaps left by collagen degradation. Skin boosters also help modulate Matrix Metalloproteinases (MMPs), a group of enzymes responsible for collagen breakdown, thereby slowing down the degradation process and prolonging the effects of skin rejuvenation [8].
Tissue Regeneration and Wound Healing
Skin boosters contribute to tissue regeneration by modulating inflammatory responses and promoting angiogenesis. The injection of HA and other regenerative compounds influences the activity of key signaling molecules such as Vascular Endothelial Growth Factor (VEGF) and Platelet Derived Growth Factor (PDGF), which enhance microcirculation and oxygenation in treated areas. This improved vascularization accelerates wound healing by delivering essential nutrients and immune cells to sites of injury or surgical intervention. Additionally, HA’s anti-inflammatory properties help regulate cytokine activity, reducing excessive inflammation and preventing fibrotic scarring. These regenerative effects make skin boosters particularly valuable in pre- and post-surgical applications, where optimal wound healing and tissue integrity are essential for successful aesthetic and reconstructive outcomes. In recent mixture of BoTN (Botulinum toxin) with HA is well-known to help prevention of surgical scar as well. PNs have demonstrated promising effects in significantly promoting skin regeneration, reducing inflammation, improving skin texture, preventing scar formation, and mitigating wrinkles [10].
Discussion
Preconditioning with Skin Boosters: Optimizing Surgical Outcomes (Figure 3)
The concept of preconditioning prior to surgery is not a new one. Plastic surgeons and dermatologists have utilized various techniques and agents prior to surgery, as well as treatment with laser/energy-based devices, in an attempt to influence the final surgical outcome. Whether the aim was to improve vascularity, pigmentation, or immunity, the ultimate goal was to optimize the healing process followed by optimal surgical outcomes. Preconditioning with skin boosters for surgical interventions, such as face/neck lifts and blepharoplasties may offer several advantages by improving quality of skin itself prior to surgical trauma. Since aged dermis has been shown through structural examination to be relatively acellular and avascular, preoperative optimizing strategies on skin hydration, elasticity, and resilience may enhance the response of skin toward surgery and promote a faster and smoother recovery. It is similar with preconditioning for general flap surgery by improving blood supply, oxygenation, and healing, which reduces the risk of flap failure. Skin boosters are included in pharmacological preconditioning category using drugs like vasodilators, antioxidants and growth factors, among various techniques such as ischemic preconditioning, hypoxia preconditioning, surgical delay technique, PRP (Platelet-Rich Plasma) and stem cell.
Preoperative skin boosters offer multiple benefits by enhancing skin hydration, elasticity, and resilience, ultimately improving surgical outcomes. Increased tissue pliability allows for better adaptability during surgical manipulations, facilitating more precise repositioning and reducing mechanical stress on the skin. In addition, well-hydrated skin is less prone to postoperative swelling and bruising, as improved microcirculation and strengthened dermal structure help minimize trauma and accelerate recovery. The refined hydration and collagen stimulation also contribute to smoother, more natural-looking results, ensuring a harmonious transition between treated and untreated areas. Furthermore, by reinforcing the skin barrier and modulating inflammatory responses, skin boosters reduce the risk of post-surgical dryness, irritation, and scarring, ultimately optimizing wound healing and minimizing postoperative complications [2].
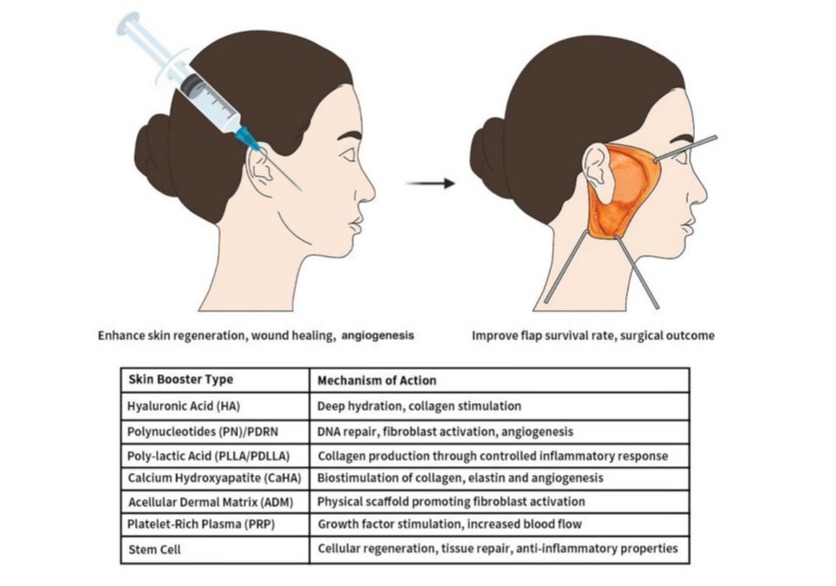
Figure 3: Preconditioning with skin boosters for rejuvenation surgery. Mechanism of action and preconditioning benefits are described for each type of skin boosters.
Clinical Applications: Skin Boosters in Rejuvenation Surgery
Skin boosters have demonstrated efficacy when used as adjuncts to various rejuvenation surgeries, including face/neck lifts and blepharoplasties. These procedures target different aspects of facial aging, and skin boosters offer complementary benefits. Traditional surgical procedures are inherently mechanical, targeting mainly visible outcomes. They often fail to address the underlying molecular and cellular changes driving the aging process, such as oxidative stress, telomere shortening, and chronic inflammation. The integration of regenerative medicine and molecular biology into aesthetic practice has driven the development of non-surgical therapies aimed at addressing the biological basis of aging [11]. A series of clinical studies have demonstrated changes in the Extracellular Matrix (ECM) as early as 2 to 3 weeks after application of skin boosters. Moreover, sonographic imaging revealed that the injected material was no longer detectable at approximately 3 weeks post-injection, indicating its integration or biodegradation within the tissue [12,13]. Clinical studies related to resurfacing procedures show accelerated healing and improved symptomatic relief compared with standard of care by preconditioning the skin 2 weeks prior to the procedure. While a single session is recommended 2 weeks prior to surgery, initiating treatment 6 to 8 weeks in advance with 2 to 3 additional sessions is advisable for optimal outcomes, allowing for cumulative improvements in hydration, texture, and structural integrity of skin. This strategic approach contributes to more refined aesthetic surgical outcomes.
Conclusion
The integration of skin boosters into rejuvenation surgery offers a promising avenue for enhancing surgical outcomes, improving skin quality, and accelerating postoperative recovery. Through their effects on hydration, collagen synthesis, and skin elasticity, skin boosters can provide complementary benefits to traditional surgical interventions, extending the longevity and enhancing the natural appearance of the results. While preliminary evidence supports the feasibility and efficacy of this combination therapy, further research is needed to refine treatment protocols and establish definitive guidelines for their use in clinical practice.
References
- Zheng J (2024) Applications of Exosomal miRNAs from Mesenchymal Stem Cells as Skin Boosters. Biomolecules 14.
- Widgerow, A.D, S.R. Cohen, and S. Fagien (2019) Preoperative Skin Conditioning: Extracellular Matrix Clearance and Skin Bed Preparation, A New Paradigm. Aesthet Surg J 39: S103-S111.
- Liang Y, Su W, Wang F (2023) Skin Ageing: A Progressive, MultiFactorial Condition Demanding an Integrated, Multilayer-Targeted Remedy. Clin Cosmet Investig Dermatol 16: 1215-1229.
- Baumann L (2007) Skin ageing and its treatment. J Pathol 211: 241251.
- Zhu Y (2015) The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell 14: 644-658.
- Canale P (2023) Long Telomeric Repeat-Containing RNA (TERRA): Biological Functions and Challenges in Vascular Aging and Disease. Biomedicines 11.
- Zhu Y (2019) Hyaluronan in adipogenesis, adipose tissue physiology and systemic metabolism. Matrix Biol 2019: 284-291.
- Rho NK (2024) Injectable “Skin Boosters” in Aging Skin Rejuvenation: A Current Overview. Arch Plast Surg 51: 528-541.
- Yi KH (2024) Skin boosters: Definitions and varied classifications. Skin Res Technol 30: 13627.
- Abuyousif HS (2025) In Vitro Evaluation and Clinical Effects of a Regenerative 2025.
- Abuyousif HS, Porcello A, Cerrano M, Marques C, Scaletta C, et al. (2025) Complex with Non-Cross-Linked Hyaluronic Acid and a HighMolecular-Weight Polynucleotide for Periorbital Treatment. Polymers (Basel) 17: 638-658.
- Song SY (2025) Redefining antiaging in aesthetic plastic surgery: from mechanical correction to biological rejuvenation. Arch Aesthetic Plast Surg 31: 31-32.
- Arora G (2021) Biorevitalization of the skin with skin boosters: Concepts, variables, and limitations. J Cosmet Dermatol 20: 24582462.
- Bezpalko L, Filipskiy A (2023) Clinical and Ultrasound Evaluation of Skin Quality After Subdermal Injection of Two Non-Crosslinked Hyaluronic Acid-Based Fillers. Clin Cosmet Investig Dermatol 16: 2175-2183.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.