Increased Liver Enzymes and Abnormal Blood Markers in Strength-training Young, Healthy Male
by S Hasselbeck1*, W Hasselbeck1, C Jochem2
1Johann-Wolfgang-Goethe-University Frankfurt am Main, Theodor-W.-Adorno-Platz 1, 60629 Frankfurt am Main, Germany
2Institute for Pathology and Cytodiagnostics Main-Taunus, Germany
*Corresponding author: S Hasselbeck, Johann-Wolfgang-Goethe-University Frankfurt am Main, Theodor-W.-Adorno-Platz 1, 60629 Frankfurt am Main, Germany
Received Date: 13 November 2024
Accepted Date: 18 November 2024
Published Date: 19 November 2024
Citation: Hasselbeck S, Hasselbeck W, Jochem C (2024) Increased Liver Enzymes and Abnormal Blood Markers in Strengthtraining Young, Healthy Male. Ann Case Report. 9: 2081. https://doi.org/10.29011/2574-7754.102081
Abstract
In this case report I want to showcase my own blood values and how caloric intake, exercise and the absence of exercise led to different outcomes of various blood samplings. A suspected liver disease, that was considered, could be ruled out by showing the effects of resistance training on some, as liver-specific-considered, blood markers. A call for more consciousness of medical doctors is included, even if it’s challenging, to provide the best healthcare possible.
Keywords: Resistance Training; Liver Enzymes; Blood Markers; Health-Workers Awareness; Creatine.
Introduction
Physical activity is widely known to improve health in various manners, such as prevention of cancer, diabetes mellitus, obesity, joint diseases and cardiovascular diseases [1]. In special resistance training (RT) with weights is known to improve everyday aspects of life, such as walking speed, physical and functional performance on a visual level and cognitive performance and self-esteem on a more non-visual level [2]. Very importantly RT improves glucose sensibility and can prevent or help manage diabetes mellitus type 2 and it decreases the likelihood of cardiovascular mediated death [3,4]. Even a decreased risk in cancer is directly linked to RT and has been proven in the case of e.g., colon cancer [5]. A further organ that benefits from RT is the liver. I has been shown that even three months of RT can reduce liver fat significantly and help fight non-alcoholic fatty liver disease (NAFLD) and decrease its hallmarks [6,7]. However, there have been reports of elevated liver enzymes (LEs) in resistance-training individuals. In a study with healthy men, known to moderate activity, but not weight training eight clinical blood parameters were sampled with aspartate aminotransferase (AST (also known as glutamic-oxaloacetic transaminase (GOT)) [8], alanine aminotransferase (ALT, also known as glutamate-pyruvate transaminase (GPT)) [9], lactate dehydrogenase (LT), creatine kinase (CK) and myoglobin being elevated for at least seven days after strenuous exercise. Especially AST and ALT were significantly increased. Bilirubin, alkaline phosphatase (AP) and gamma-glutamyl transferase (GGT) remained unchanged after RT [10]. Another case report of a 39-year-old with no drug-use-habits and no known liver diseases within his family documented significantly increased LEs in the subject. ALT reached values of more than double the reference value. Even after ultrasound examination and liver biopsy no clinical alarming findings were observed. However, after one week of RE absence the LE-values nearly fully recovered with only ALT and albumin being 3 and 1 value points, respectively, above the reference-limit [11]. In this case report I want to showcase my own experiences as a weight-lifting, young, healthy and drug-free male that received elevated LE-values after three blood samplings over the course of half a year with no signs of disease. The goal is to put emphasis on the need to interpret blood values in considerations of the lifestyle of a patient.
The Subject
The subject is a 25-year-old (24 when the first blood sample was taken) male that lift weights since being shy to 16 years old. The height is 163 cm and the weight in the morning of the samplings were 59.8 kg at the first sampling, 64.9 kg at the second sampling and 64.3 kg at the third sampling. Always being at a good muscular condition and comparable low body fat. There are no cases of reported liver disease in the family. The subject does not consume alcohol, cigarettes, any medication and isn’t using any other drugs including performance enhancers (PEDs). Thereby it could be ruled out that the liver damaging effects of alcohol [12] or PEDs like anabolic androgenic steroids (AAS) [13] or the synergistic effects of smoking [14] to those factors could have been to blame. The only supplementation applied is on the one hand 400 mg of magnesium twice a day. Which is not known to impact LE-values [15]. On the other hand a daily supplementation of 3-5 g of creatine monohydrate (CM) is applied. CM has been shown multiple times to be not damaging towards the liver while having multiple benefits like strength and endurance increase and improvement of cognitive functions [16,17]. In people aged 65 an older there is even evidence that CM increases liver health [18].
The Circumstances during Blood Sampling
When the first sampling was conducted the subject sat at the end of a 2 month long hypocaloric diet with the caloric intake being around 1800 kcal/day at the time of the sampling, which marked an estimated deficit of 1200-1300 kcal/day. Furthermore, the need to be fasted at the blood sampling was misinterpreted, which led to an 8-hour abstinence of food and water. During that time, the first training week since the last deload (light training week or no RT at all) took place and six cumulative days of hard RT took place. On the day of the sampling no RT took place but one hour of cycling immediately prior to the sampling.
During the second sampling a hypercaloric diet was applied with a daily intake of about 3400-3500 kcal a day with an estimated surplus of 200 kcal/day. Blood was sampled fasted but hydrated. The sampling took place in the second week of a RT accumulation phase and was done after a RT session.
The third sampling took place in a hypercaloric diet with a daily intake of 3500-3600 kcal with a similar surplus being estimated. Sampling took place after a fasted RT session with normal hydration. The fourth week of accumulative RT was taking place at this point.
Results of Blood Sampling
The first Sampling
The values of the first sampling are shown in Table 1.

Table 1: Original blood sampling data from the first sampling.
The first value that is out of order are the decreased leukocytes. While there is knowledge that in the subject’s family smaller amounts of leucocytes than usual were reported (father, grandmother on the father’s side and uncle on the father’s side), in this case the decreased leucocytes could be explained by the hypocaloric diet that went on since two months. It is reported that caloric restriction, even when no malnutrition is occurring, a decrease in leucocytes can take place because of redistribution of cellular material [19]. Next on, creatinine shows an increased value. This can, however, be attributed to the fact that (fasted) exercise took place just before the blood sampling. Physical activity is linked to higher creatinine values. Further, high protein consume is linked to higher creatinine values, as well as high muscle mass [20]. On top of that, creatine is continuously degraded into creatinine, which also leads to increased creatinine values when creatine supplementation takes place, without indicating organ damage [21,22].
Lastly, even fasting and dieting can be linked to increased creatinine values [23]. The next increased value is urea (in the table termed ‘Harnstoff’). Like before, this value is known to be increased after exercise [24]. The two increased values of AST and ALT follow the same pattern, that was already discussed in the introduction, showing increase in healthy, but active men. Especially interesting is to note, that the values, that did not experience an increase in the study, did not experience an increase in the subject, being bilirubin, AP and GGT [10]. The final value, different from the norm, is the glomerular filtration rate GFR. This could be explained by the fact that the fasting was interpreted as water-fasted. Therefore, it would be possible that the kidneys just ‘had nothing to filtrate’ [25]. Further, it is known that exercise can artificially decrease renal function, because the renal blood flow can decrease to as low as 25% [26]. However, because this value was concerning the most, another blood sampling took place.
The second sampling
The values of the second sampling are shown in Table 2.

Table 2: Original blood sampling data from the second sampling.
The second sampling shows a recovery of the leucocytes. This can be attributed to the fact that the diet was turned into a hypercaloric one and that the cellular distribution of nutrients shifted back to the leucocytes [19]. Creatinine still being increased, but to a lesser extent. This may be attributed to the fact that the subject was better fed, due to the hypocaloric diet. The recovery of the kidneys can be explained by the fact that the water consumption prior to the sampling was normal. The slightly decreased renal function can again be attributed the exercise prior [25,26]. The LE-values show the same pattern like in the study of Petterson et. al. again. GPT and GOT show increases and bilirubin, AP and GGT remain within the normal boundaries [10]. Nonetheless, the examining doctor could not explain the norm-deviant values and therefore transferred the subject to a gastroenterologist. There a third sampling was conducted.
The third sampling
The values of the third sampling are shown in Table 3.
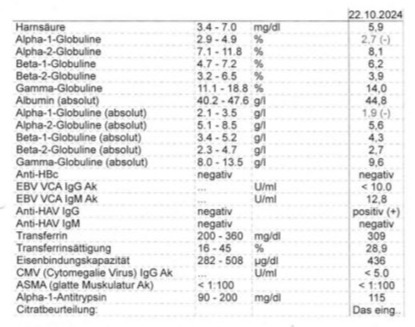
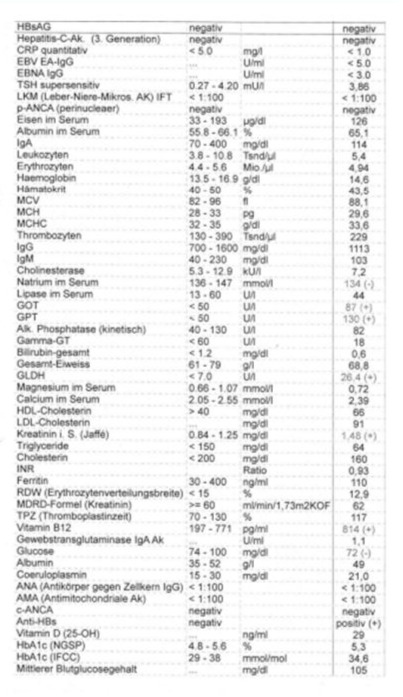
Table 3: Original blood sampling data from the third sampling.
Minor deviations in sodium, vitamin B12, glucose and alpha-1- globuline were observed but interpreted as harmless. However, the already observed pattern of increased GOT- and GPT-values (AST and ALT) was observed. But as beforehand, like in the study of Petterson et. al., AP, GGT and bilirubin didn’t show an increase [10]. Another value that was now measured for the first time and seemed way out of the normal range was the glutamate dehydrogenase (GLDH). However, it is known that glutamate levels increase as soon, as exercise is started and that glutamate levels are increased even at rest in people that are generally active [27,28]. Especially the short-term increase in glutamate levels after exercise, could explain the rise in GLDH because the sampling took place about one hour after a vigorous leg workout [29]. Despite the clear literature, that could explain the increased (liver)-markers and a ultrasound examination that revealed no signs of liver damage, the medical doctor continued to suggest that something has to be wrong with the liver. Even after pointed towards the literature he looked for excuses and blamed the consumed creatine and hypothesized about AAS, which were not even consumed. Also, the literature about the benefits of CM were pointed out towards the examining doctor and the safety regarding the liver [16,23]. Anyhow, the doctor insisted that CM and ‘everything else’ should be stopped taken and that another sampling should be conducted and if the values would not have normalized a liver biopsy would have had to be considered.
At this point it was clear, that the already present published data needed another update and a prove that CM is not harmful and norm-divergent blood- and especially LE-values can be caused by RT.
Therefore, another sample was taken, but under self-determined conditions. The fourth sampling was done with the help of Dr. med. Christopher Jochem, after the subject de-loaded its training routine for six days. That meant in this case no heavy lifting in the six days before the sampling and no lifting for three days immediately before the sampling, at all. During that time 3300-3400 kcal/day were consumed, which equals a roughly isocaloric condition and the average weight in that week was 65,2 kg.
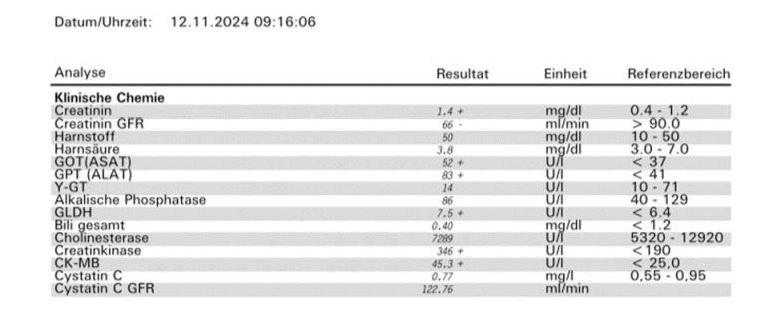
Table 4: Original blood sampling data from the fourth sampling.
Minor deviations in sodium, vitamin B12, glucose and alpha-1globuline were observed but interpreted as harmless. However, the already observed pattern of increased GOT- and GPT-values (AST and ALT) was observed. But as beforehand, like in the study of Petterson et. al., AP, GGT and bilirubin didn’t show an increase [10]. Another value that was now measured for the first time and seemed way out of the normal range was the glutamate dehydrogenase (GLDH). However, it is known that glutamate levels increase as soon, as exercise is started and that glutamate levels are increased even at rest in people that are generally active [27,28]. Especially the short-term increase in glutamate levels after exercise, could explain the rise in GLDH because the sampling took place about one hour after a vigorous leg workout [29]. Despite the clear literature, that could explain the increased (liver)-markers and a ultrasound examination that revealed no signs of liver damage, the medical doctor continued to suggest that something has to be wrong with the liver. Even after pointed towards the literature he looked for excuses and blamed the consumed creatine and hypothesized about AAS, which were not even consumed. Also, the literature about the benefits of CM were pointed out towards the examining doctor and the safety regarding the liver [16,23]. Anyhow, the doctor insisted that CM and ‘everything else’ should be stopped taken and that another sampling should be conducted and if the values would not have normalized a liver biopsy would have had to be considered.
At this point it was clear, that the already present published data needed another update and a prove that CM is not harmful and norm-divergent blood- and especially LE-values can be caused by RT.
Therefore, another sample was taken, but under self-determined conditions. The fourth sampling was done with the help of Dr. med. Christopher Jochem, after the subject de-loaded its training routine for six days. That meant in this case no heavy lifting in the six days before the sampling and no lifting for three days immediately before the sampling, at all. During that time 3300-3400 kcal/day were consumed, which equals a roughly isocaloric condition and the average weight in that week was 65,2 kg.
The fourth sampling
On the day of the fourth sampling the subject slept for 10 hours, walked about 3000 steps before the sampling and had not drunk or eaten for 12 hours. The resulting data is shown in Table 4.
While creatinine decreased by 0,08 mg/dl it was still about the reference value. However, this could be linked to the continued high protein consume [20]. Furthermore, the increased creatinine value, compared to the norm, could still be attributed to the higher than usual muscle mass of the subject. Therefore, the cystatin C value is more interesting, because this is mass independent. This value shows, in fact, no deviation from the norm [20]. Adding to that, the GFR is low again. This could be attributed to the 12-hour water-fast, what was already discussed to be known to increase serum creatinine values [25-29]. Very importantly, the beforehand normal values of bilirubin, GGT and AP remained in the normal boundaries. Simultaneously GOT experienced a decrease of 35 U/l (40,2%) compared to the previous sampling, GPT a decrease of 47 U/l (36,2%) and GLDH a tremendous decrease of 18,9 U/l (71,6%). Depending on which referencing-values are taken, GOT was now only 2 U/l away from the norm and GLDH 0,5 U/l. All this in just three days of complete RT-abstinence while a moderate level of activity was held up. This goes very well along with the findings of Petterson et. al. in that RT can significantly and artificially increase LE-blood values [10]. It is to hypothesize that one or two more days of abstinence could have been enough to fully reach the normal boundaries again. Furthermore, it was proven again that CM does not have negative influence on LE-values, because it was continuously taken during the RT-reduced and -free time. Lastly, the creatine kinase (CK) was tracked for the first time. The value is way out from the norm. It’s however, hard to interpret this value, because it was not investigated during previous samplings. It cannot be attributed to the CM supplementation, as the literature shows [30]. However, CK is known to be able to shoot up to 30-times the normal value after strenuous exercise and then decline over up to a weak. With the last hard RT-session being six days prior to the sampling and the last intensity-reduced session three days, it’s very likely that a slight elevation of 1,82-times (slight compared to 30-times) could have still been present [31].
Conclusion
All in all, it was shown in another case report, that RT can artificially lead to increase in some, thought to be liver specific, blood-markers like GOT/AST, GPT/ALT10 and GLDH [27,28]. At the same time, some markers remain unaffected like bilirubin, GGT and AP [10]. Other markers like creatinine has to be looked at while the body type is considered, because not only exercise, but also muscle mass can falsify creatinine values. A more relevant markers is therefore cystatin C, because its independent from a person’s mass [20]. And the decrease of values like GFR and leucocytes also have to be interpreted with hydration-levels, exercise status and caloric situation of each individual patient [19,25,26]. Furthermore, it was again shown, that CM-supplementation does not lead to an increase in LE-values [16,23]. Because of this all, it is essential to consider the life situation of each patient for a medical doctor, before he concludes damage. This can not only lead to fear and stress in a patient, but also to unnecessary medical interventions like biopsies. Even in such scientifically fruitful times, where knowledge is gained at high rates, a medical doctor should always be motivated to update its knowledge regarding the latest literature. Thereby, he can grant an optimal treatment and advice for his patients.
This also shows that an absence of sports for a couple of days or even a week can be a good idea if a subject wants to prevent unnecessary visits at a doctor’s office or even worse, unnecessary medical interventions.
I hereby hope to do my part in presenting a case report, that emphasizes the need to look at each patient individually and have in mind, which values are really meaningful and which aren’t. Adding to that, the presentation of data from a patient’s site towards a medical doctor should be considered as support, and not threat.
Author Contributions: S.H. served as the subject, did the research, analysis and writing. W.H. supported the analysis with discussion. C.J. supported the analysis with discussion and enabled the selfdetermined blood-sampling. All authors have read and agreed to manuscript. Special thanks go also out to Athina Zerva, who insisted on a blood sampling in the first place.
Funding: This research did not receive any funding.
References
- Warburton, D. E. R., Nicol, C. W. & Bredin, S. S. D. (2006) Health benefits of physical activity: the evidence. CMAJ : Canadian Medical Association Journal 174: 801.
- Westcott, W. L. (2012) Resistance training is medicine: effects of strength training on health. Curr Sports Med Rep 11: 209–216.
- Kobayashi, Y. Long J, Dan S, Johannsen NM, Talamoa R, et al. (2023) Strength training is more effective than aerobic exercise for improving glycaemic control and body composition in people with normal-weight type 2 diabetes: a randomised controlled trial. Diabetologia 66: 1897– 1907.
- Liu, Y. Lee DC, Li Y, Zhu W, Zhang R, et al. (2019) Associations of Resistance Exercise with Cardiovascular Disease Morbidity and Mortality. Med Sci Sports Exerc 51: 499.
- Mazzilli, K. M., Matthews, C. E., Salerno, E. A. & Moore, S. C. (2019) Weight Training and Risk of 10 Common Types of Cancer. Med Sci Sports Exerc 51: 1845.
- Zelber-Sagi, S. Buch A, Yesua H, Vaisman N, Webb M, et al. (2014) Effect of resistance training on non-alcoholic fatty-liver disease a randomized-clinical trial. World Journal of Gastroenterology : WJG 20, 4382.
- Hallsworth, K. Fattakhova G, Thoma C, Moore S, et al. (2011) Resistance exercise reduces liver fat and its mediators in non-alcoholic fatty liver disease independent of weight loss. Gut 60, 1278–1283.
- Dhillon, A. & Steadman, R. H. (2012) Liver Diseases. Anesthesia and Uncommon Diseases: Sixth Edition 162–214.
- Washington, I. M. & Van Hoosier, G. Clinical Biochemistry and Hematology. The Laboratory Rabbit, Guinea Pig, Hamster, and Other Rodents 57–116.
- Pettersson, J. Hindrof U, Persson P, Bengtsson T, Malmqvist U, et al. Muscular exercise can cause highly pathological liver function tests in healthy men. Br J Clin Pharmacol 65: 253.
- Tiller, N. B. & Stringer, W. W. (2020) Exercise-induced increases in “liver function tests” in a healthy adult male: Is there a knowledge gap in primary care? J Family Med Prim Care 12: 177.
- Agarwal, S., Fulgoni, V. L. & Lieberman, H. R. (2016) Assessing alcohol intake & its dose-dependent effects on liver enzymes by 24-h recall and questionnaire using NHANES 2001-2010 data. Nutr J 15: 62.
- Androgenic Steroids. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury.
- Rutledge, S. M. & Asgharpour, A. (2020) Smoking and Liver Disease. Gastroenterol Hepatol (N Y) 16: 617.
- Karandish, M., Tamimi, M., Shayesteh, A. A., Haghighizadeh, M. H. et al (2013)The effect of magnesium supplementation and weight loss on liver enzymes in patients with nonalcoholic fatty liver disease. J Res Med Sci 18: 573.
- Todorovic, N., Korovljev, D., Stajer, V., Jorga, J. & Ostojic, S. M. (2022) Creatine consumption and liver disease manifestations in individuals aged 12 years and over. Food Sci Nutr 11: 1134.
- Kreider, R. B. Kalman DS, Antonio J, Ziegenfuss TN, Wildman R, et al. (2020) International Society of Sports Nutrition position stand: safety and efficacy of creatine supplementation in exercise, sport, and medicine. J Int Soc Sports Nutr 14: 18.
- Ostojic, S. M., Korovljev, D. & Stajer, V. (2021) Dietary intake of creatine and risk of medical conditions in U.S. older men and women: Data from the 2017–2018 National Health and Nutrition Examination Survey. Food Sci Nutr 9: 5746–5754.
- Contreras, N. A., Fontana, L., Tosti, V. & Nikolich-Žugich, J. (2018) Calorie restriction induces reversible lymphopenia and lymphoid organ atrophy due to cell redistribution. Geroscience 40: 279.
- Baxmann, A. C. Ahmed MS, Marques NC, Menon VB, Pereira AB, et al. (2008) Influence of Muscle Mass and Physical Activity on Serum and Urinary Creatinine and Serum Cystatin C. Clin J Am Soc Nephrol 3: 348.
- Longobardi, I., Gualano, B., Seguro, A. C. & Roschel, H. (2023) Is It Time for a Requiem for Creatine Supplementation-Induced Kidney Failure? A Narrative Review. Nutrients 15: 1466.
- Post, A., Tsikas, D. & Bakker, S. J. L. (2019) Creatine is a Conditionally Essential Nutrient in Chronic Kidney Disease: A Hypothesis and Narrative Literature Review. Nutrients 11: 1044.
- Kreider, R. B., Jäger, R. & Purpura, M. (2022) Bioavailability, Efficacy, Safety, and Regulatory Status of Creatine and Related Compounds: A Critical Review. Nutrients 14.
- J, C.-E. Cunningham JJ, Snyder P,Jacob R, Huszar G, et al. (1984) Influence of exercise on urea, creatinine, and 3-methylhistidine excretion in normal human subjects. Am J Physiol 246.
- Telford, T. Keane D, Garner AE, Waller ML, Scarsbrook AF, et al. Assessing the impact of inadequate hydration on isotope-GFR measurement. Scand J Clin Lab Invest 79: 86–90.
- Poortmans, J. R. (1984) Exercise and renal function. Sports Med 1: 125–153.
- Maddock, R. J., Casazza, G. A., Fernandez, D. H. & Maddock, M. I. (2020) Acute Modulation of Cortical Glutamate and GABA Content by Physical Activity. J Neurosci 36: 2449–2457.
- Abdullah, M. Lin SH, Huang LC, Chen PS, Tseng HH, et al. Fat loss and muscle gain: The possible role of cortical glutamate in determining the efficacy of physical exercise. Obes Res Clin Pract 18: 163–170.
- Walsh, N. P., Blannin, A. K., Robson, P. J. & Gleeson, M. (2018) Glutamine, exercise and immune function: Links and possible mechanisms. Sports Medicine 26: 177–191.
- Taylor, B. A., Panza, G., Ballard, K. D., White, C. M. & Thompson, P. D. (2018) Creatine supplementation does not alter the creatine kinase response to eccentric exercise in healthy adults on atorvastatin. J Clin Lipidol 12: 1305–1312.
- Moghadam-Kia, S., Oddis, C. V. & Aggarwal, R. (2016) Approach to asymptomatic creatine kinase elevation. Cleve Clin J Med 83: 37.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.