Impact of Training on Learning, Feedback, and Assessment among Family Medicine Residents
by Ghada Alarfaj, Lina Alelewi, Ayman Afifi, Tarek Elsaid, Mostafa Kofi*
Family Medicine Training Program, Family and Community Medicine Dept, Prince Sultan Military Medical City, Ministry of Defense Health Services, Riyadh, Saudi Arabia
*Corresponding author: Mostafa Kofi, Family Medicine Training Program, Family and Community Medicine Dept, Prince Sultan Military Medical City, Ministry of Defense Health Services, Riyadh, Saudi Arabia
Received Date: 20 May 2025
Accepted Date: 28 May, 2025
Published Date: 30 May, 2025
Citation: Alarfaj G, Alelewi L, AfifiA, Elsaid T, Kofi M (2025) Impact of Training on Learning, Feedback, and Assessment among Family Medicine Residents. Educ Res Appl 9: 240. https://doi.org/10.29011/2575-7032.100240
Abstract
Background: The training of family medicine residents requires a multifaceted and comprehensive approach to developing clinical expertise and interpersonal competencies. Central to this process is the ability to effectively receive, process, and act on feedback-an essential component of adult learning. High-quality feedback fosters reflective practice, enhances self-regulation, and promotes lifelong learning among medical professionals. Methods: This mixed-methods study evaluated 49 residents in a Family Medicine Training Program. The first cohort (20 residents) received no formal training in feedback and assessment, while the second cohort (29 residents) underwent formal training through the SCFHS Training of Trainers (TOT) program. Data collection methods included structured interviews, Likert-scale questionnaires, and open-ended questions. Qualitative data were summarized in tables, while quantitative results were presented as bar graphs. Results: The second cohort, which underwent formal training, reported a stronger sense of trust in their trainers compared to the first cohort. Additionally, they demonstrated higher confidence in their ability to give and receive feedback, provide constructive feedback, and conduct self-assessments and peer assessments. Conclusion: Introducing family medicine residents to contemporary adult learning methodologies for feedback and assessment early in their training yields significant benefits. It enhances trust in trainers, boosts confidence, and strengthens residents' skills in providing constructive feedback and conducting self-assessments. These improvements contribute meaningfully to their professional growth and development.
Keywords: Feedback; Assessment; Family medicine; Training residents
Introduction
The literature consistently highlights the pivotal role of feedback in helping residents identify and address performance gaps while reinforcing their strengths. Emerging evidence from leading medical and family medicine education journals underscores the positive impact of feedback and assessment training on optimizing learning outcomes for family medicine residents. Training programs that emphasize adult learning principles, structured feedback frameworks, and innovative assessment methodologies are increasingly associated with improved outcomes.
Effective Feedback Practices According to Van de Ridder et al. (2015) [1], feedback achieves optimal efficacy when delivered using structured frameworks such as the "feedback sandwich" or Pendleton’s model. These models emphasize the importance of balancing positive reinforcement with constructive critique to create a psychologically safe learning environment. Structured approaches to feedback delivery enhance clarity and reduce defensiveness among recipients, thereby fostering actionable insights that facilitate continuous improvement.
- Challenges in Feedback Delivery from Bing-You et al. (2017) [2] identified several barriers to effective feedback, including:
- Faculty hesitancy to deliver critical feedback due to concerns about potential negative impacts on resident morale.
- Residents’ discomfort in receiving feedback, which may impede their engagement and learning.
Addressing these challenges through targeted faculty development and resident training programs is critical to cultivating a productive feedback culture. The impact on Resident Performance in Empirical studies underscores the transformative potential of high-quality feedback. For instance, Archer et al. (2018) [3] in Medical Teacher demonstrated that consistent, well-structured feedback significantly improved residents' clinical decision-making and communication skills over six months. Training Residents in Feedback Reception and the impact of feedback extends beyond its delivery; it also depends on the recipient's ability to engage with and effectively apply the information. Training residents in feedback reception aligns with adult learning theories and encourages autonomy, self-reflection, and professional growth. Adult Learning Principles by Knowles' andragogical model, which emphasizes self-directed learning and experiential engagement, provides a robust framework for feedback training. Schultz et al. (2020) [4] demonstrated that incorporating these principles into workshops enhanced residents' ability to process and integrate feedback constructively.
Workshops and Role-Playing through Interactive workshops employing role-playing and simulated feedback scenarios have proven effective in enhancing residents’ feedback receptivity. Cantillon and Sargeant (2014) [5] reported a 25% increase in resident satisfaction with feedback sessions following the introduction of such interventions. These methods foster empathy and active listening, enabling residents to approach feedback with openness and curiosity. Assessment Training for Enhanced Learning means that Assessment serves as the foundation for feedback by providing residents with objective measures of their performance relative to established benchmarks. Structured training in self-assessment and peer assessment amplifies the benefits of feedback by fostering self-awareness and collaborative learning.Self-Assessment through Structured self-assessment exercises, as highlighted by Eva et al. (2018) [6] in Academic Medicine, enhance residents' ability to identify their strengths and areas for improvement. These exercises align with principles of reflective practice, empowering learners to take ownership of their professional development. Adapted from Eva et al. (2018).
Peer Assessment provide a complementary perspective to faculty feedback, fostering a supportive and collaborative learning environment. Wagner et al. (2019) [7] found that residents were more receptive to feedback from peers, reporting reduced defensiveness and increased engagement. Additionally, Green et al. (2019) [8] in Family Medicine demonstrated that peer assessments improved team dynamics and communication skills, essential for interdisciplinary care. Technology-Enhanced Feedback and Assessment and its integration of technology into medical education have expanded the avenues for feedback and assessment. Digital tools and platforms enhance the accessibility, immediacy, and quality of feedback while supporting reflective learning practices. Online Feedback Platforms like MedHub and E*Value internationally, and locally such as One45 platform adopted by the SCFHS facilitate real-time feedback exchanges between faculty and residents. Chen et al. (2020) [9] in BMC Medical Education reported that these tools increased both the frequency and quality of feedback, fostering a continuous feedback culture.
Also, Video-Based Assessments Video recordings, and reviews of clinical encounters offer residents opportunities for self-evaluation and multifaceted feedback. Taylor et al. (2022) in Family Medicine demonstrated that video-based assessments improved diagnostic accuracy, patient communication skills, and reflective practice. Adapted from Taylor et al. (2022) [10]
Rationale: this study will try to investigate the evidence for giving structured courses of feedback and its effect on residents’ competencies in learning.
Methods
A mixed methods study in which we had 4 focus group discussions, each group of 6 to 8 residents using a mixed methods study covering 49 Family Medicine Training program residents. We interviewed two batches, The first batch without doing the feedback and assessment training, The second group was interviewed after conducting the Feedback and assessment training .The first patch had no formal training on feedback and assessment, and another patch of 29 residents had been through the formal training of feedback and assessment, it’s the same contents of the official SCFHS Training of Trainers (TOT) on feedback and assessment and were interviewed through structured interview and mixed methods of Likert scale questions and open-ended questions. Data collected were analyzed and presented as a table format for open-ended questions and also as bar graphs for Likert scale questions. A Google form for questions having a Lickert scale. The questionnaire and focus group questions are attached.
Results
PART 1: Perspectives of the first batch group interview results were as follows without training on feedback and assessment:
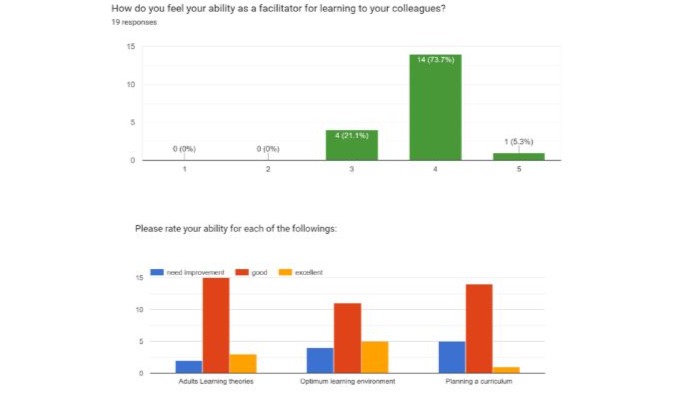
Figures (1-2): Residents' perception of Learning, without training.
|
Residents explain in one paragraph why they selected the above selections. |
|
1. I have a good understanding of adult learning theories, allowing me to tailor educational experiences that resonate with adult learners' unique needs and preferences. I have experience in creating optimum learning environments that foster engagement, collaboration, and practical application of knowledge. My expertise in planning a curriculum ensures a structured yet flexible approach, accommodating diverse learning styles and promoting continuous improvement. This combination enables me to design effective, learner-centered educational programs that drive meaningful outcomes. |
|
2. For me, adult learning theories were first times I heard to me, therefore I understood what to do and what to feel about a good presentation. i can provide such a cooperative environment, finally regarding planning i think i have the skill but i need to be good at it. |
|
3. , i feel that though this year i can manage the learning environment and planing the curriculum with no problems |
|
4. I contacted the consultant a head of time with a well-prepared presentation, that’s why I choose good on planning a curriculum. Regarding the optimum learning environment, I used all the available facilities + tried to give cash ? as gift. |
|
5. The last point which is adult learning theories, I do not have such an expertise that’s why needing improvement was my answer. |
|
6. Boredom during lectures. |
|
7. I feel confident in teaching any subject from my specialty according to the different experiences I had, as much as I have experienced my confidence has increased, and also I had a good experience in providing a good learning environment. Also, I was part of the team that revised the WADA curriculum for 2025, so I feel involved. |
|
8. Adult learning- familiar with the overarching concepts, but not able to list the breakdowns of what each domain is. |
|
9. Optimum learning environment - Having receptive consultants and Professors has helped to foster an open and collaborative environment that doesn't penalize not having knowledge. Any workplace or team culture is infectious. Once there is a positive supportive environment to train in, you are more likely to apply to the same when you are training someone else in the future. |
|
10. Planning a curriculum- this is a little too specialized for the level I'm at right now. Possibly having the residents help design the structure of the curriculum would help |
|
11. I am adept at creating an optimal learning environment that supports interaction and inquiry. This environment encourages students to explore ideas and fosters a culture of academic curiosity and respect, crucial for effective learning. |
|
12. Adults learning theories provide insight into the way learners make connections between new information and prior knowledge, store memories, and transfer knowledge to new contexts. |
|
13. An optimum learning environment improves academic performance and an overall general understanding of the subject matter being taught. |
|
14. Planning curriculum ensures optimum good coverage of all domains within the curriculum. |
|
15. Because I still need more practice as it’s essential in mastering any skill with consistent practice I will be able to continue to improve and achieve excellence in these aspects of learning and learning facilitation |
|
16. I find my ability in the adult learning theories and the learning environment in the average,, while I think I have a weakness regarding a planning a curriculum |
|
17. In terms of learning theories and planning the curriculum I have the skills but did not improve in the past year, while the learning environment is something I haven’t really tried to optimize before. |
|
18. For me environment plays a major role and the environment in our program is really helping, although may be if we could have 2 WADA sessions instead of 3 to be presented is going to be more comfortable and give a time to focus. |
|
19. I feel like i need more improvement. More experience will help. |
|
20. It was all good and helpful in our learning process |
|
21. I believe we have the time to plan the curriculum as well we have enough time to search for the latest updates regarding the topic. then we come to the last point which is the environment which is fully equipped with the latest tech. |
|
22. So cooperative team, a good learning method |
|
23. I feel that I provided the needed information and knowledge in each subject i was asked to present, also I try to answer all questions asked by them. However, i might need little more improvement to provide more, so that my colleagues benefit fully. |
|
24. I can learn more and want to keep improving and aiming to be excellent |
|
25. These skills need more practice to be excellent as experts, but during the past, since I started the residency program it given me chance to be good at. |
|
26. Moreover, at the end of R2 the skills will be more mature with practice. |
Table 1: The data collected from residents before training were summarized as follows:
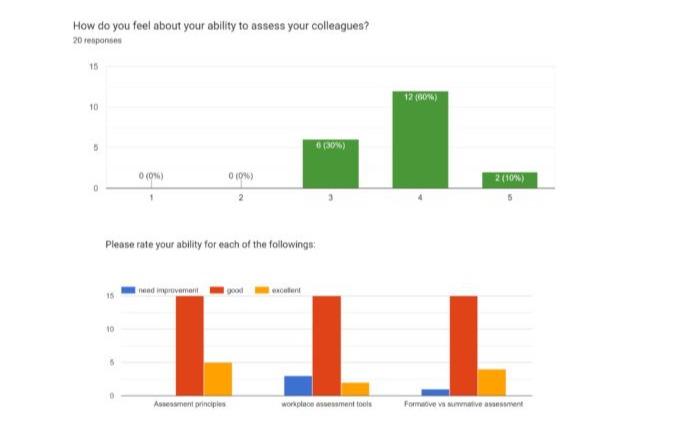
Figures (3-4) Residents' perception of Assessment without training.
|
Residents explain in one paragraph why they selected the above selections. |
|
1. I have a good foundation in assessment principles, which allows me to effectively evaluate learner progress and program effectiveness. My proficiency with workplace assessment tools ensures that assessments are practical, relevant, and aligned with real-world tasks, providing accurate measures of competency. Additionally, I have good experience in implementing both formative and summative assessments; formative assessments offer ongoing feedback to guide learning, while summative assessments provide comprehensive evaluations of learner achievement. This balanced approach ensures a thorough and supportive assessment process that promotes continuous improvement and success. |
|
2. Good to know and definitely it’s important. |
|
3. I have a good idea about it but i think i need more training on it and to practice more assessment overall considered average not excellent and an improvement is always needed! |
|
4. Need for more Family medicine clinics rotations |
|
5. I feel good, thanks to my experience with the instructors who assessed me and my colleagues, every time I learn something new with every instructor as everyone is having different style of assessment. |
|
6. Workplace assessment tools – have not had a chance to apply them in real life myself so i can’t reflect on past experiences to guide my self-perception. It would help if the concepts of KPIs and benchmarks were introduced earlier on to us during training |
|
7. Formative vs summative is clear; |
|
8. Assessment principles good because we can learn how to effectively design and implement assessments that accurately measure a learner's progress and achievements. |
|
9. Workplace assessment tool is drive great learning growth. |
|
10. Formative vs summative assessment is good Because formative assessments are designed to offer feedback about what students need, and when used regularly and appropriately, they drive stronger student performance. |
|
11. Because I still struggle to pick up the strengths and weaknesses in my colleagues |
|
12. I think I have an excellent assessment principle, regarding workplace tools and formative and summative assessment I am on average |
|
13. I believe I could be good at evaluating once i have the proper variables, but did not receive proper training in it. |
|
14. In our program everything is organized and that is really good , may be at the beginning there was misunderstandings and we didn’t really understand the process but then with the help of our instructors it got easier and more organized |
|
15. It is good but I'm not sure how to improve it. |
|
16. At the end of the year I feel more confident |
|
17. I believe I understand the assessment tools the only issue i find in them is that sometimes once we are in an outside rotation we find it hard to get the Mini-Cex or dops done not that the doctors refuse to sign but usually it takes sometime for them to sign . |
|
18. Excellent teaching skills, only need to have extra class for training and provide adequate equipment |
|
19. I understand that assessing each resident is a crucial part in learning, but sometimes it is difficult to obtain a full assessment due to the little time and work load we have during the working hours. |
|
20. I need to be better |
|
21. Clear way to assess a trainee, but the most important part is the agreement from the committee on how to assess and aspects use during the assessment. For example (number of cbd , mini cex )needed from the beginning of training. |
Table 2: Please explain in one paragraph why you selected the above selections.
Figures (5-6) Residents' perception of Feedback without training.
|
Residents explain in one paragraph why they selected the above selections. |
|
1. I have the ability to deliver effective feedback, which is clear, constructive, and tailored to individual needs, facilitating meaningful growth and improvement. I understand the barriers to feedback, such as communication gaps, resistance to criticism, and cultural differences, and I employ strategies to overcome these challenges, ensuring that feedback is received and acted upon positively. By integrating feedback seamlessly into daily practice, I create a culture of continuous learning and development, where feedback is not just an occasional activity but a core component of the learning and improvement process. |
|
2. Effective feedback means talking about tasks and work, not personal feedback. And its aim to improve me and my skills. We all need a good feedback system ?? |
|
3. Giving feedback needs experience and practice and i think i need to work more on that |
|
4. Feedback is my strongest point, As I always start with complimenting the best in the presenter work and when I mention something needs improvement I always bring options and reassure him that we all could do the same and overall it doesn’t affect their performance!. |
|
5. Some trainers give no chance for reflecting |
|
6. I learned a lot since the start of the program alhamdulilah, it has been a cooperative and kindly guiding experience, thanks to my colleagues who helped me a lot in since I was accepted in the 3rd match, I also found all of the instructors keen to help and helped me a lot catching up, I feel warmth and welcomed whenever I have feedback to give from all the instructors and program managers and directors. Also I find actions of change and improvement every time |
|
7. Have been unable to incorporate daily feedback, as time can be tight in clinics. Also it’s easy to forget to give positive feedback when the environment is busy. |
|
8. Barriers such as time constraints and emotional sensitivities can hinder this process. To integrate feedback effectively into daily practices, it’s beneficial to establish regular review sessions and promote an open communication culture. This approach ensures that feedback becomes a constructive part of your academic and research routine, fostering continuous improvement and clearer understanding. |
|
9. Feedback can help to provide confidence, reinforcement and motivation for the performer. |
|
10. Although I get a lot of compliments about my feedback skills I still find some barriers to be in my way such as fear of conflict being reluctant to criticize my colleagues. However I started a new way by which I can overcome such barriers such as communicating clearly and promoting growth oriented mindset towards feedback this allowed me to give the feedback without being too harsh on the other person |
|
11. I see myself I can do effective feedback, and on average regarding the barriers for feedback and doing incorporated feedback into daily practice |
|
12. Constructive Feedback is important, and we are constantly doing it to improve, but I don’t think i am excellent. |
|
13. I didn’t really focus on my feedback to my colleagues but i can say, we are doing a good job in giving feedback and following them |
|
14. I have built good relationship with my colleagues during activities which i feel made my ability in giving effective feedback better and have less barriers. |
|
15. Thank you |
|
16. Lack of time I believe is the barrier to feedback. |
|
17. Only need more practice time or classes for trainers |
|
18. Providing feedback to a colleague is crucial but sometimes i find it difficult to give a resident within my level this information as that we all have some weaknesses and strengths. I need to work on improving this point. |
|
19. Need more improvement in constructive and impactful feedback, need to apply feedback more routinely in practice |
|
20. Effective feedback about a subject needs more experience not about one field but, it is a scientific way to emphasis the maximum benefit. |
Table 3: Please explain in one paragraph why you selected the above selections.
PART 2: Perspectives of FM Residents for the 2nd Batch Who had a Training on Feedback and Assessment:
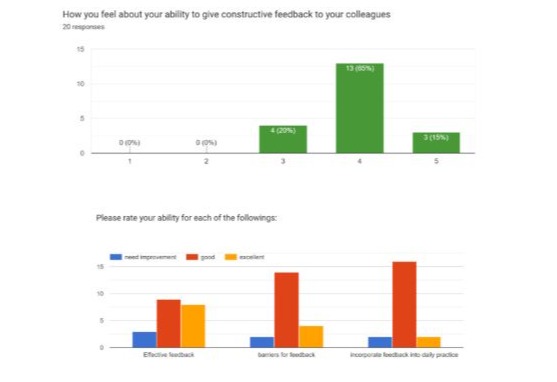
Figures (7-9) Residents' perception as a Facilitator of Learning after training.
|
Residents explain in one paragraph why they selected the above selections. |
|
1. I feel overall okay with the abilities mentioned formerly. |
|
2. I think that I don’t have experience in planning a curriculum. |
|
3. But regarding the learning theories I think I have enough knowledge about it to implement them in the future |
|
4. The workshop was intense and clear on these topics |
|
5. I believe following last Thursday's TOT it improved my awareness of learning theories.. For the learning environment I believe it differs depending on each learner's preference ex: observation, exam based.. etc. |
|
6. After Thursday's TOT, I do feel confident in my abilities to optimize the learning environment and adults learning theories since it was discussed thoroughly. However, at my level I think I need improvement regarding curriculum planning. |
|
7. I’m motivated and oriented to learning, I feel can support learners, |
|
8. The tot was very clear and effective. |
|
9. To always try to improve me in different aspect, and evaluate my self |
|
10. As this is the first time I am introduced to TOT and such learning modalities, it was never introduced neither in medical college or in other career experiences, but from what we have seen during our introductory course I might say we are somehow familiarized with the concept of TOT |
|
11. I feel good and I need more improve and time to be excellent |
|
12. I believe I’m capable of establishing appropriate knowledge regarding the above abilities given their inevitable nature to expand and improve one’s clinical and academic status. |
|
13. I feel more confident about learning and teaching methods and make a good learning environment, thankfully to our trainers |
|
14. I am really interested in participating in different learning methods and improve my learning and my colleagues learning experience the adult way is kind of knew experience to me i am used to other ways of learning and also planning a curriculum not easy also because your setting a timetable for long time and sometimes for a lot of people. I think the best way to know is after practicing. |
|
15. I think I need to improve myself as a facilitator and self-confidence. |
|
16. I rated myself good with previous selections because I attended informative lectures about it in the introductory course and learned about it and I should be excellent in the future after implementing it. |
|
17. I could follow adult learning theories, but not always choose the environment. Quite confident about planning curriculum to be used in knowledge seeking skills and implement in personal life. |
|
18. Because I know each term what does it means, by the teaching of Doctor Ghada, Dr.Aymn, Prof kofi, and Dr.Lina we had a great session by a great explanation with examples that made it easy to understand and guided us to start using it, but i need to use it more and more to be expert on it |
|
19. I feel good about the learning theories and understand them but not very well with planning the curriculum and i think with time i will get the hang of it. |
|
20. i would like to thank Dr. Ghada, Prof. Kofi, Dr ayman , and Dr. Lina who spent the time and effort to help me understand the adult learning theories in a very pleasant and fun way. |
|
21. I think teaching some topics needs some skills how to teach and i don’t think i have these skills |
|
22. I believe that I am good in the first two choices because I have learned them through an induction course. But I don’t just knowing how to make objectives according to taxonomy is enough for me to plan a whole curriculum. |
|
23. I understand them but as they are a lot it may need a little memorization |
|
24. Because it helps me for continuous learning process improvement |
|
25. In Thursday’s session it was a very new learning technique and subject for me. I will consider reflection in my daily routine. However, it’s mandatory to give yourself a chance to explore your feelings and emotions in any situation you face. All the doctors in that session taught me how to deal with any situation. Thank you so much for this amazing welcoming environment |
|
26. I always work and study by planning and using schedules so I think I can plan. |
|
27. Adult learning theories is very good in paper, but it needs to be implemented |
|
28. Optimum learning environment is based on the characteristics of the trainer, even if he or she provides the best environment it won't help without the drive to teach and the confidence and latest knowledge |
|
29. Planning a curriculum is on an administrative level and needs more training and practice at least for me |
|
30. I need to refresh my memory and practice each item in order to give myself a higher / more accurate rating. But for now, this is fair rating. |
|
31. I see myself as good and I can be excellent with the time |
|
32. I chose the above selections based on what we had the last 2 weeks in the introductory course, and because my Wada presentation was on that week as well. Moreover, I’m not expert in the topics listed above, but at least I understand the basics of it and what it means. And I think I can reflect some of them in my practice |
Table 4: Please explain in one paragraph why you selected above selections?
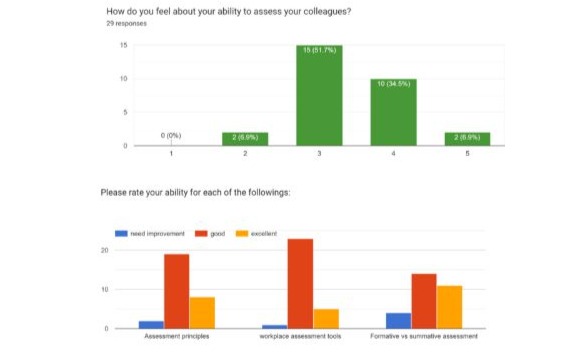
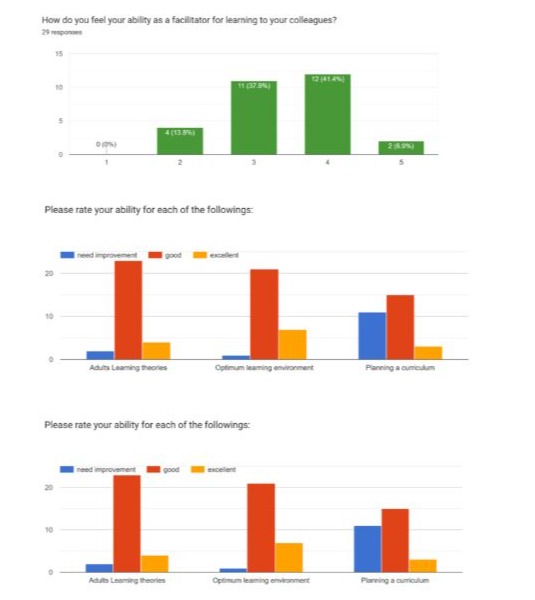
Figures (10-11) Residents' perception of Assessment after training.
|
Residents explain in one paragraph why they selected the above selections. |
|
1. I feel that I can critique and assess my colleagues fairly based on my level and point out areas in which they can improve. |
|
2. Formative and summative assessments is clear for me to use also using workplace assessment tools |
|
3. They have been explained clearly during the TOT |
|
4. And i feel confident to use them in the future |
|
5. Because it includes the skills and knowledge required to be learned |
|
6. I chose 3 in assessing my colleague due to lack of clinical experience in FM. Following TOT session, I became aware of assessment principles, tools and formative vs summative. |
|
7. I feel most confident about work-place assessment as we were clearly informed about them since day one. |
|
8. Assessment principles and formative and summative assessment were well explained that I feel good regarding them. |
|
9. I feel good in Identify area for improvement and evaluation |
|
10. I Understand various assessment tools and how to apply it in various condition. |
|
11. To always try to improve myself in different aspect , and evaluate myself , |
|
12. And i need more time and experience to be able more to reflect |
|
13. As the previous answer i do not have enough experience to decide my ability to do the mentioned |
|
14. I feel good and I need more improve and time to be excellent |
|
15. Integrating those particular skills allows oneself to progressively encourage a more a fundamental approach in betterment regarding assessment skills. Additionally, I reckon I need to improve the first to points to swiftly execute in assessing myself properly. |
|
16. Assessment should provide valid information about the actual idea , using assessments tools |
|
17. Assessment is necessary to test our level of learning and can be done by multiple tools which i want to know i think i still need practice to master all different methods and know the different principles. |
|
18. I learned from the TOT workshop how to assess |
|
19. I think I understand these areas |
|
20. Assessment principles are clearer for me rather than before and I could use them in the future with my colleagues, workplace assessment great tool I could use it as a reflection on theoretical knowledge, and formative and summative assessment reminds me to keep up and do my best to keep achieving and reaching a goal and maintain my effort and excellence. |
|
21. I know what each terminology means by examples, I appreciate all the effort our doctors made by make it possible to assess ourselves and my colleagues to improve our skills throughout the academic year not only at the end of the year which make more opportunities to achieve high level of improvement |
|
22. I understand them well but would need a bit of training using them to fully be able to use these principles |
|
23. I know how to assess my colleagues in general, but I really don’t know to assessment by Formative vs summative way |
|
24. I have learned the principles of assessment and have been taught the elements of formative and summative assessments. |
|
25. I feel I have a solid understanding of the principles, tools, and assessments. |
|
26. It helped me understand and know the tasks |
|
27. In order to get excellent marks i should know the assessment process. I mean i should first know how to do the assignment how to submit it and how the doctor evaluate. Before going into a real assessment. |
|
28. I think it is good to have tools and principles for assessment. |
|
29. Using these tools would help me in assessing my colleges/others and it would be fair. |
|
30. All of the above abilities were explained in the introductory course but unfortunately for me it was a lot of new terminology for me and new field of practice to become a trainer for me Which i want to be Insha’Allah |
|
31. I have good knowledge about the principles, and I need to practice it to improve |
|
32. I think i want to improve myself in assessment in some part I’m good but i think i can be better |
|
33. I don’t like to assess my colleagues because it might cause hard feelings between us, not everyone would accept an assessment from someone at their level. Regarding the choices of the assessments, it is clear and well explained by the faculty. |
Table 5: Please explain in one paragraph why you selected the above selections.
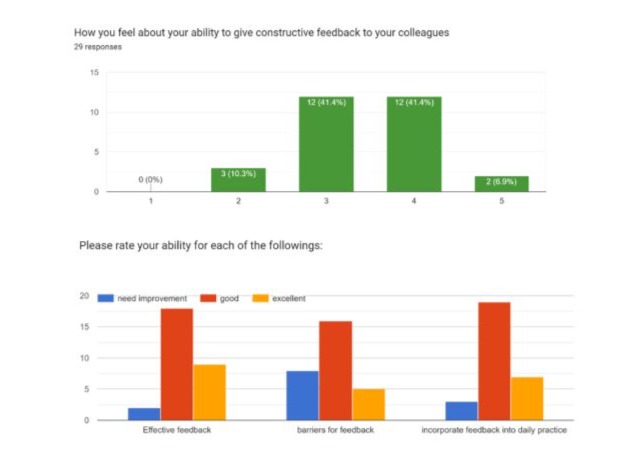
Figures (12-13) Residents' perception of Feedback after training.
|
Residents explain in one paragraph why they selected the above selections. |
|
1. In my opinion, i can provide positive feedback for my colleagues in case they ask for it or I notice an area in which they need to improve in. I feel that i can provide feedback without being personally or biased. |
|
2. My goal will be to improve me and my colleagues work and practice and this will be the motivation to give them feedback in a proper way and receive their feedback with no hard feelings |
|
3. Feedback lead to continuous learning, to enhance learning process |
|
4. I am aware now of how to give a constructive FB for example using the sandwich method, 1min preceptor, barriers to FB and how to incorporate it in daily practice. |
|
5. I think i can give effective feedback using the sandwich technique, trying to be professional, nonjudgmental, and helpful. |
|
6. I'm also aware about the feedback barrier such as fear of criticism or being judged and lack of good communication. |
|
7. I intend to involve feedback in my daily practice to improve myself personally and professionally. |
|
8. Feedback I try to aim positive first than negative And apply it on daily practice for improvement Because importance of providing constructive feedback to colleagues to insure promoting continuous improvement. |
|
9. In wada i think it is going to be effective way to reflect my feedback. |
|
10. Giving feedback is both positive for the assessor and the recipient, unlike the other questions i might have some previous experience in receiving and sometimes giving feedback, yet i might think there are some areas of improvement |
|
11. I feel good and I need more improve and time to be excellent |
|
12. Incorporation of feedback requires factual application of critique without emotional establishment which entirely enables oneself to truly acquire a beneficial judgement. |
|
13. Appreciative feedback. It helps to reinforce positive habits and encourages more of the performance that you want to see. |
|
14. As i never take or given feedback i am excited in to participate in it in my point of view I see feedback as reflection of all the work we have done. |
|
15. I think barriers for feedback will hold me and including feedback into daily practice might be difficult, but I will learn how to overcome this barrier |
|
16. We got the theoretical but with practice in future we will be better |
|
17. I could give feedback upon feedback models if I am aware enough on the subject, nevertheless some barriers for feedback may occur as the time and environment and personal situations, feedback always a great tool i could use on my daily practice. |
|
18. Many thanks for our outstanding doctors they made feedback skill easy to know and to use, they teach us the importance of feedback even if you are the one who will give the feedback, and we are aware about barriers of feedback and when& how to give it. |
|
19. I understand the techniques of giving feedback and the barriers and the terms but would need to get used to giving feedback in order to become more familiar with it and excel at it. I really appreciate the time and effort spent by my instructors to teach me these techniques. |
|
20. I feel some of my feedback my broken relationships between my and my colleagues especially if they are close friends |
|
21. I know when giving feedback there a lot of methods (e.g. feedback sandwich) so I have confidence in giving to my peers. I can think of a couple of barriers to giving feedback (state of the person receiving it, level of seniority in some cases) but I don’t get the question frankly. |
|
22. I feel I might struggle to give feedback due to fear of delivering it constructively and being well received. |
|
23. Because the feedback leads to continuous improvement, and knowing our weak points and improving it. |
|
24. Feedback for any person usually they will take it personally. How you handle it well varies from person to person. For me, I selected my answers as good because I’m not excellent in negative feedback although respect will be given to everyone. I hope I will be able to handle negative feedback and improve myself in the residency program. |
|
25. Feedback is important for growth and improvement. |
|
26. Effective feedback is I think is dependent on the person who is receiving it, If he takes it or not, But of course, it needs to be presented in a professional manner and based on real error or excellence |
|
27. In the 1/ 3 i believe in my ability to give effective feedback, 2/ I does not recall the barriers, so I need to refresh my memory |
|
28. Giving feedback is the best think to show you understand and what you want, i see my self is goon on that |
|
29. As I mentioned above, in case of feedback if my colleague is willing to listen to the feedback, I will gladly give feedback otherwise I would not. |
|
30. Regarding the introductory course, the only issue is that there were a lot of repetition in the topics, But in the end, thank you it was very helpful ??. |
Table 6: Please explain in one paragraph why you selected the above selections.
Visual Comparison of Graphical Likert scales answers of figures 1-3 with figures 4-6 gave interesting findings. So, as a summary of these results, from figures (1-3) residents are hesitant to express trust in their ability to conduct feedback and conduct assessments for themselves and their colleagues, while after training in figures (4-6); it apparent that after training residents had more sense of being able to conduct learning facilitation, feedback, and assessment very well, yet after training, residents were more cautious to express their abilities in facilitating learning, giving feedback and assessment.
Thematic Analysis: from the comments in tables (1-3) among the cohort of residents with no training,
- Residents have a strong sense of understanding of Adult Learning Theories.
- Residents expressed confidence in teaching the subjects
- Residents reflected feel their ability to assess and give feedback
- Residents expressed interest in providing an optimal learning environment
And for the Cohort with the formal training from comments listed in tables (4-6):
- There is an overall sense that this training helped residents deepen their understanding of the optimal learning environment, feedback, and assessment.
- Residents are hesitant to express their ability to plan and conduct a teaching session for their colleagues.
- Residents express their knowledge of Assessment principles, and their feel of ability to assess their colleagues, yet need more training and understanding of Workplace Based Assessment tools required by the SCFHS.
- Residents expressed more confidence in their ability to give feedback after training, describe barriers, and ability to give feedback.
Discussion
The findings highlight the significant potential of feedback and assessment training in family medicine residency programs. It comes in alignment with international available evidence on positive impact of feedback training on performance of family medicine residents’ trainings [11,12]. By grounding interventions in adult learning principles and leveraging structured frameworks, medical educators can enhance residents’ engagement and skill development. Innovations such as peer assessments, technology-enhanced feedback, and role-playing scenarios address critical gaps in traditional feedback practices.
The context of residents in training active role in learning and assessment have been the subject of research on the local, [13-15] regional [16,17] and international levels; and evidence on its benefits for the training program outcomes are building up, whether in family medicine specialty residents training programs or other programs. Despite these advances, challenges remain, including achieving faculty buy-in, standardizing feedback delivery,
and addressing variability in residents’ receptiveness. Future research should explore longitudinal outcomes and the role of cultural competence in feedback training.
Conclusion
Enhancing the learning experience of family medicine residents through introductory training on adult learning theories, designing a curriculum, giving feedback, barriers to feedback and assessment, represents a positive strategy for advancing clinical competence and reflective practice. By integrating evidence-based feedback and assessment frameworks, optimal learning environment, and aligning with principles of adult learning, educators can foster a robust culture of feedback and reflection that benefits both residents and faculty alike.
References
- Van de Ridder JMM, et al. (2015) What is feedback in clinical education? Medical Education, 49: 757-769.
- Bing-You RG, et al. (2017) Feedback falling on deaf ears: Residents' receptivity to feedback tempered by sender credibility. Medical Teacher 39: 128-134.
- Archer JC, et al. (2018) The impact of feedback on clinical performance: A narrative review. Medical Teacher. 40: 873-885.
- Schultz K, et al. (2020). Enhancing feedback in residency training: A workshop model. Journal of Graduate Medical Education. 12: 255-260.
- Cantillon P, Sargeant J. (2014) Giving feedback in clinical settings. BMJ. 348: g3011.
- Eva KW, et al. (2018) Self-assessment and self-directed learning in medical education: A systematic review. Academic Medicine. 93: 360-365.
- Wagner DP, et al. (2019) Peer assessment in clinical education: Benefits and challenges. Journal of Graduate Medical Education. 11: 45-53.
- Green D, et al. (2019) Peer assessment and its impact on team-based care: A family medicine perspective. Family Medicine. 51: 312-318.
- Chen Y, et al. (2020) Technology-enhanced feedback in medical education: A review of online tools. BMC Medical Education. 20: 123.
- Taylor B, et al. (2022) Video-based feedback in family medicine: Enhancing patient care through reflection. Family Medicine. 54: 472-478.
- Long M, et al. (2020) Improving outpatient feedback delivery in family medicine: A structured approach. Family Medicine 52: 587-593.
- Patel N, et al. (2021) Role-playing as a tool for feedback training in family medicine residency. Family Medicine. 53: 399-404.
- Alrashed DA , Said TE, Kofi MA (2023) Family medicine residents’ perspectives on different teaching modalities used throughout their training. J Family Med Prim Care 12: 1291-1297.
- Gharawi A M, Alateeq A M, Alarfaj G, Afify A, Albatal S, et al. Perception of Family Medicine Residents on the Use of Small Group Discussion in Comparison to Standard Lectures. European Journal of Contemporary Education and E-Learning. 2: 3-18.
- Al Helal AH, Al Turki Y, (2019) Family medicine residents’ educational environment and satisfaction of training program in Riyadh. J Family Med Prim Care 8: 1330-1336.
- Koshmaganbetova G, Zhamaliyeva L, Abenova N, Dilmagambetova G, Zhylkybekova A, et al. (2022) Residents’ Perception of the Educational Program “Family Medicine” in Kazakhstan: A Focus Group Study. Open Access Maced J Med Sci 10: 844-851.
- Nawabi S, Bilal R, Javed MQ (2021) Team-based learning versus Traditional lecture-based learning: An investigation of students’ perceptions and academic achievements. Pak J Med Sci 37: 1080-1085.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.