IgG4-Related Sclerosing Cholangitis Presenting as Klatskin Tumour: A Diagnostic Dilemma - A Case Report and Literature Review
by AbdulAziz Al Hinai, Shahazad Younis, Amit Mahajan, Humaid Al Farii*, Adil Al Zadjali
Department of Surgery, Sultan Qaboos University Hospital (SQUH), Dr Ali Al Bimani St, Seeb, Oman
*Corresponding author: Humaid Al Farii, Department of Surgery, Sultan Qaboos University Hospital (SQUH), Dr Ali Al Bimani St, Seeb, Oman
Received Date: 06 December 2024
Accepted Date: 11 December 2024
Published Date: 13 December 2024
Citation: Hinai AA, Younis S, Mahajan A, Farii HA, Zadjali AA (2024) IgG4-Related Sclerosing Cholangitis Presenting as Klatskin Tumour: A Diagnostic Dilemma - A Case Report and Literature Review. J Surg 9: 11205 https://doi.org/10.29011/2575-9760.011205
Abstract
Background: IgG4‐related sclerosing cholangitis (IgG4‐SC) is benign inflammatory disorder that causes sclerosis and fibrosis of the biliary system. It is characterized by elevation of IgG4 serum levels. Usually, IgG4‐SC is associated with autoimmune pancreatitis. Differentiation of IgG4‐SC primary sclerosing cholangitis and cholangiocarcinoma (CCA) is difficult, but is of utmost important for management of these patients .
Case presentation: We report the case of a 71 years old gentleman who presented with obstructive jaundice. He had been diagnosed from imaging to have Klatskin type IV tumor and the plan was made for operative intervention as per the diagnosis. However, the patient wanted to sought second opinion where they diagnosed him as IgG4‐SC by IgG4 level serum was found elevated. After treatment with steroids, the patient’s jaundice improved.
Conclusions: Surgeons should be aware about IgG4-SC characteristics and how to differentiate Cholangiocarcinoma diagonally from Primary sclerosing cholangitis.
Keywords: Benign biliary stricture; Cholangiocarcinoma; IgG4, Sclerosing cholangitis; Primary sclerosing cholangitis
Introduction
IgG4‐Related Sclerosing Cholangitis (IgG4‐SC) is a fibro inflammatory condition that effects the billiary system . It is a type of secondary sclerosing cholangitis [1] and is characterized by elevation of serum IgG4 levels and is associated frequently with autoimmune pancreatitis (AIP). The pathophysiology of IgG4-SC is unknown, and its clinical features are like that of Primary Sclerosing Cholangitis (PSC) and Cholangiocarcinoma (CCA) [2-4]. In our article , we describe a case of IgG4-SC that was mimicking as Klatskin tumour and review the clinical manifestations , pathologic/radiological findings, diagnosis,management and prognosis of this entity .
Case Report
A 71 years old gentleman was admitted to hospital with a diagnosis of obstructive jaundice for further evaluation. He presented with 3 weeks history of vague abdominal pain, loss of weight (5 kg over two months) and appetite, generalized body itching and jaundice. He was a known case of Hypertension and Hyperlipidemia on medications. On examination the abdomen was soft, not distended, not tender and there was no palpable mass. The laboratory investigations were done (Table 1). On radiology, the MRI showed features suggestive of hilar periductal neoplastic pathology with obstructive biliopathy, focal inflammatory changes of the pancreatic head, few calcified lesions noted in the right diaphragmatic region and along the lateral margin of the splenic parenchyma (Figure 1: A and B). Based on MRI findings a diagnosis of Klatskin type IV tumor was reached and a management plan was made which include surgical intervention. However, before proceeding for surgery, IgG4 had been requested and found to be elevated. For the reason, the diagnosis of IgG4‐SC was made and he was started on steroid therapy leading to resolution of symptoms.
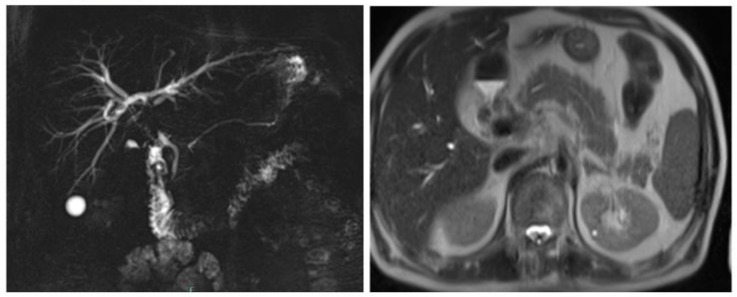
Figure 1(A and B): MRI showed Features suggestive of hilar periductal neoplastic pathology with obstructive biliopathy and focal inflammatory changes of the pancreatic head.
|
Test Item |
Value |
Units |
Reference Range |
|
CRP ( C - Reactive Protein ) |
12 |
mg / L |
0-5 |
|
CA 19-9 |
146 |
KIU/L |
0-37 |
|
CEA ( Carcino embryonic antigen ) |
2.7 |
ug/L |
0-4 |
|
Haemoglobin |
5.03 |
mg/dl |
10-12 |
|
Lipase |
800 |
U/L |
0-160 |
|
Alanine Aminotransferase |
165 |
U/L |
0-41 |
|
Albumin |
39 |
g/L |
35-52 |
|
Alkaline Phosphatase |
450 |
U/L |
40-129 |
|
Aspartate Aminotransferase |
105 |
U/L |
0-40 |
|
Bilirubin |
242 |
umol/L |
0-17 |
Table 1: The abnormal laboratory findings of our patient have complete blood counts, liver function test and tumor/inflammatory markers.
Discussion
IgG4‐SC presents clinically in 7th or 8th decade of life and is more commonly seen in men as compared to female by ratio of 4:1-8:1 [3,5-7]. Up to 20% of the cases show an association with some allergic diseases which are considered as predisposing factors like sinusitis, bronchial asthma and drug allergies [3,8]. The clinical presentation is very comparable to cholangiocarcinoma. However chronic and recurrent cholestatic jaundice is the most common [75%] presentations [3,9]. Symptoms include pruritus, fever, abdominal pain, and weight loss [3,10]. Also, the main presenting symptom can be caused by another pathology such as Autoimmune pancreatitis type 1 which is associated with IgG4-SC can also mimic symptoms of obstructive jaundice due to a mass formation in the head of pancreas [3]. Cholangiocarcinomas (CCA) are classified into extrahepatic and intrahepatic cholangiocarcinoma based on their anatomical site of origin , the former being most common (90%). Extrahepatic CCA is further divided into perihilar (50%) and distal (40%). Perihilar (Klatskin tumor ) is when a tumor develops at the junction of the right and left hepatic ducts. Only 10% of CCA cases are Intrahepatic cholangiocarcinomas. The peak of incidence of CCA is between 60-70 years age. The main risk factors are ulcerative colitis, primary sclerosing cholangitis, toxins, infective, congenital, alcohol excess and diabetes mellitus [11]. The pathology is usually clinically asymptomatic until advanced stage of the disease [12-15] with painless jaundice as clinical presentation in 90% of the cases. It is also associated with pruritus, pale stools, dark urine and less commonly: weight loss, right upper quadrant abdominal pain, anorexia and malaise. On examination, jaundice and cachexia are more prominent in CCA [12]. Table 2 shows the different characteristic features of IgG4-related sclerosing cholangitis, Cholangiocarcinoma and Primary sclerosing cholangitis [3].
|
Features |
IgG4-SC |
PSC |
CCA |
|
Location |
Extrahepatic > intrahepatic |
Extrahepatic plus intrahepatic mostly |
Hilar more often than extrahepatic more often than intrahepatic |
|
Length of involvement |
Long, continuous |
Short, multiple |
Short, single |
|
Duct wall thickening |
Symmetric, often > 2.5 mm |
Symmetric, usually < 2.5 mm |
Asymmetric, > 5 mm |
|
Margins of thickening |
Sharp and smooth |
Fuzzy and smooth |
Fuzzy and irregular |
|
Lumen of thickened segment |
Often visible |
Often occluded |
Mostly occluded |
|
Duct dilatation |
Less (< 9 mm) |
mild |
Gross |
|
Contrast enhancement |
Single layer |
Uniform |
Double layer |
|
Skip lesions |
Common |
Less common |
Rare |
|
Liver parenchymal changes |
Seen in late stages |
common |
Rare |
|
Others |
Funnel-shaped dilatation |
Pruned tree ducts, diverticula |
Vascular invasion |
|
Associations |
AIP |
Inflammatory bowel disease |
Usually none |
|
Serum IgG4 level |
Elevated in majority |
Usually normal |
Usually normal |
|
Response to steroids |
Good |
Good |
No response |
Table 2: characteristic features of IgG4-SC , PSC and CCA.
The pathology of IgG4‐SC shows sclerosing fibrosis and infiltration of lymphoplasmacytic with IgG4-positive plasma cells of bile duct [16]. IgG4‐SC is strongly suggested to cause stenosis however thickened bile duct wall with smooth outer margin without stenosis ( visible lumen ) are more commonly seen in IgG4-SC patients, figure 2 [17]. Most cases of IgG4‐SC that are associated with autoimmune pancreatitis shows stenosis of the lower bile duct the cause of which is still unknown and can be mostly due to pancreatitis enlargement or IgG4-SC. Gallbladder lesion of IgG4-related disease which present as thickened wall of the gallbladder is considered as a significant difference between IgG4‐SC and CCA. Thickened wall of the gallbladder is strongly suggestive of IgG4‐SC [17-19]. Cholangiocarcinoma is an adenocarcinoma which is a malignant epithelial neoplasm arising from the biliary tree. Usually, CCA causes obstruction of bile duct which lead to obstructive jaundice and there is increase of serum total bilirubin levels [17]. CCA does not involve other organs unless it is metastasized. Some cases of CCA shows abundant infiltration of IgG4-positive plasma that mean infiltration of IgG4-positive plasma is not specific for IgG4-SC and hence could not be diagnosed as IgG4-SC only by immunostaining (Figure 2) [17,20-22].
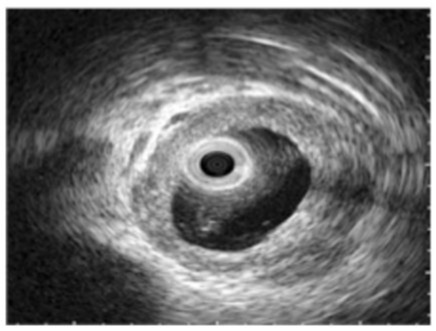
Figure 2: Intraductal ultrasonography shows wall thickness with smooth outer margins in the bile ducts without stenosis in immunoglobulin G4-related sclerosing cholangitis patients [17].
Ultrasound [US]) is done as initial investigation for most patients who are thought to have IgG4‐SC or CCA [3,23]. Usually US finding are normally in the early stages of IgG4‐SC but in the late stages it will show circumferential wall thickening of the bile duct without stenosis and dilatation of intrahepatic bile ducts [3,24]. Also, US helps in the identification of associated findings in gallbladder and pancreases. Intraductal US (IDUS ) of IgG4‐SC shows high accuracy of imaging of the duct wall. IDUS shows diffuse symmetric homogeneous wall thickening with smooth margins and the lumen is preserved [10,25]. On IDUS, the cutoff value of bile duct wall thickness without strictures is 0.8mm and it is a characteristic feature of IgG4‐SC (sensitivity 95-100% and specificity 91%) and it is an important feature which can help to differentiate IgG4‐SC from cholangiocarcinoma [10,25,26]. The finding of CT and MRI in IgG4‐SC and CCA mostly same in US but more accuracy in CT and MRI. CT and MRI finding of IgG4‐SC was circumferential symmetric bile duct wall thickness with smooth inner and outer margin, and lumen is visible [3,27,28]. These findings can be used to differentiate between IgG4‐SC and CAA (80% sensitive, 90% specific) [3,26,27].
Serum IgG4 level is one of the most important characteristic to diagnosis of IgG4-SC. The cutoff of serum level IgG4 is 135 mg/dl and it show 74% of sensitivity to diagnose IgG4-SC. This cutoff level showed lower specificity in distinguish diagonally between IgG4-SC and CCA [2,28,29]. the IgG4 serum level is elevated in some cases of CCA and patients who has both CCA+PSC are more likely to exhibit high level of IgG4 than those with only CCA. So increased serum IgG4 level alone cannot use to diagnoses the IgG4-SC [4,29,23,30]. However, to diagnose IgG4-SC from serum IgG4 level alone, the level of IgG4 should be four time higher than normal level which showed 100% specific for IgG4-SC [10,29,30].
The diagnosis of IgG4-SC is very difficult due lack of specific diagnostic features. There are two sets of diagnostic criteria for IgG4-SC have been proposed: HISORt criteria and Japanese and Korean guidelines of IgG4-SC diagnosis. HISORt criteria (Histology, Imaging, Serum IgG4, Other organ involvement and Response to therapy), according to this criteria , to diagnose a patient with IgG4-SC should go over histological bile duct investigation , bile duct imaging , IgG4 serum level, other organ involvement such as AIP, and response to steroid therapy [3,4,29]. The Japanese and Korean guidelines are more recommended comparing HISORt criteria Table 3 [31,32]. It includes similar diagnostic features of IgG4-SC and suggestion of different diagnostic categories (possible diagnoses, probable and definitive) based on combinations of these features. Also, Japanese guideline included three distinguished histopathological findings which are Marked lymphocytic and plasmacyte infiltration, Infiltration of IgG4-positive plasma cells, Storiform fibrosis and Obliterative phlebitis [2,3,32] (Table 3).

Table 3: Japanese Diagnostic criteria for Diagnosis of IgG4-SC.
Diagnosis of IgG4-SC should be done before starting therapy. A steroid trait is a diagnostic feature of IgG4-SC therapeutic management to continue if diagnosis is confirmed [31]. A short-term steroid trial is recommended by a specialists in diagnostically challenging cases or suspicion mimicking PSC or cholangiocarcinoma. Also recommended in all cases that associated with AIP. The assessment of effectiveness of steroid trials should be done after 1 or 2 weeks of steroid administration and confirming diagnosis by resolution of findings on bile duct images. However sometimes in advanced-stage IgG4-SC, steroid therapy may be ineffective because of fibrous scarring of bile duct which not response to steroid therapy, so that should be considered in steroid trail attempt for diagnosis IgG4-SC [4].
IgG4-SC is treated by high dose of corticosteroids ( oral prednisolone, 30-40 mg/day ) with gradual reduction of dose depending on response. After remission occurred, the dose (2.5-5 mg/ day) will be maintenance for minimal of 3 year. Usually the response of medication will be in 4-6 weeks and it will be shown as reduction in serum IgG4, improvement in biliary strictures and normal liver function test. Patients who show comfortable radiological and serological improvement, the treatment can be is discontinued but they need to be up for relapse [3,4,31]. Surgery in IgG4-SC is not necessary except if there is chronic biliary obstruction or is high risk of developing malignancies.
Conclusion
IgG4-SC is a benign bile duct disorder that could mimic serious diseases such as CCA. Surgeons should be aware about IgG4-SC characteristics and how to differentiate this disease from PSC and CCA. Whenever IgG4-SC is suspected we recommend that IgG4 serum levels should be examined. HISORt criteria or Japanese guidelines are most recommended to guide for diagnosis. Steroid is the effective treatment of IgG4-SC.
References
- Rungsakulkij N, Sornmayura P, Tannaphai P (2017) Isolated IgG4-related sclerosing cholangitis misdiagnosed as malignancy in an area with endemic cholangiocarcinoma: a case report. BMC Surg 17: 17.
- Ghazale A, Chari S, Zhang L, Smyrk TC, Takahashi N, et al. (2008) Immunoglobulin G4-associated cholangitis: clinical profile and response to therapy. Gastroenterol 134: 706-715.
- Madhusudhan KS, Das P, Gunjan D, Srivastava DN, Garg PK (2019) IgG4-Related Sclerosing Cholangitis: A Clinical and Imaging Review. AJR Am J Roentgenol 213: 1221-1231.
- Joshi D, Webster GJ (2014) Biliary and hepatic involvement in IgG4-related disease. Aliment Pharmacol Ther 40: 1251-1261.
- Inoue D, Yoshida K, Yoneda N, et al. (2015) IgG4-related disease: dataset of 235 consecutive patients. Medicine (Baltimore) 94: e680.
- Wolfson A R, Hamilos DL (2017) Recent advances in understanding and managing IgG4-related disease. F1000Res 2017.
- Zen Y, Kawakami H, Kim JH (2016) IgG4-related sclerosing cholangitis: all we need to know. J Gastroenterol 51: 295-312.
- Björnsson E, Chari ST, Smyrk TC, Lindor K (2007) Immunoglobulin G4 associated cholangitis: description of an emerging clinical entity based on review of the literature. Hepatology 45: 1547-1554.
- Vlachou PA, Khalili K, Jang HJ, Fischer S, Hirschfield GM, et al. (2011) IgG4-related sclerosing disease: autoimmune pancreatitis and extrapancreatic manifestations. RadioGraphics 31: 1379-1402.
- Naitoh I, Nakazawa T, Ohara H, et al. (2009) Endoscopic transpapillary intraductal ultrasonography and biopsy in the diagnosis of IgG4-related sclerosing cholangitis. J Gastroenterol 44: 1147-1155.
- Itoh S, Nagasaka T, Suzuki K, Satake H, Ota T, et al. (2009) Lymphoplasmacytic sclerosing cholangitis: assessment of clinical, CT, and pathological findings. Clin Radiol 64: 1104-1114.
- Koyama R, Imamura T, Okuda C, Sakamoto N, Honjo H, et al. (2008) Ultrasonographic imaging of bile duct lesions in autoimmune pancreatitis. Pancreas 37: 259-264.
- Yata M, Suzuki K, Furuhashi N, Kawakami K, Kawai Y, et al. (2016) Comparison of the multi- detector-row computed tomography findings of IgG4-related sclerosing cholangitis and extrahepatic cholangiocarcinoma. Clin Radiol 71: 203-210.
- Nakazawa T, Naitoh I, Hayashi K, et al. (2012) Diagnostic criteria for IgG4-related sclerosing cholangitis based on cholangiographic classification. J Gastroenterol 47: 79-87.
- Kato A, Naitoh I, Miyabe K, et al. (2018) Differential diagnosis of cholangiocarcinoma and IgG4-related sclerosing cholangitis by fluorescence in situ hybridization using transpapillary forceps biopsy specimens. J Hepatobiliary Pancreat Sci 25: 188-194.
- Ohara H, Okazaki K, Tsubouchi H, et al. (2012) Research Committee of IgG4-related Diseases. Re- search Committee of Intractable Diseases of Liver and Biliary Tract; Ministry of Health, Labor and Welfare, Japan; Japan Biliary Association. Clinical diagnostic criteria of IgG4-related sclerosing cholangitis. J Hepatobiliary Pancreat Sci 19: 536-542.
- Dodd GD 3rd, Baron RL, Oliver JH 3rd, Federle MP (1999) End-stage primary sclerosing cholangitis: CT findings of hepatic morphology in 36 patients. Radiology 211: 357-362.
- https://next.amboss.com/us/article/e30xhf?q=cholangiocarcinoma#Ze752ce7897a26cb713e3e45a36ed68fd
- Gatto M, Alvaro D (2010) Cholangiocarcinoma: risk factors and clinical presentation. Eur Rev Med Pharmacol Sci 14: 363-367.
- Cha Jm, Kim Mh, Lee Sk, Seo Dw, Lee Ss, et al. (2006) Clinicopathological review of 61 patients with early bile duct cancer. Clin Oncol 18: 669-677.
- Anderson CD, Pinson CW, Berlin J, Chari RS (2004) Diagnosis and treatment of cholangiocarcinoma. Oncologist 9: 43-57.
- Fevery J, Verslype C, Lai G, Aerts R, Van Steenber, et al. (2007) Incidence, diagnosis, and therapy of cholangiocarcinoma in patients with primary sclerosing cholangitis. Dig Dis Sci 52: 3123-3135.
- Tabata T, Kamisawa T, Hara S, et al. (2013) Differentiating immunoglobulin g4-related sclerosing cholangitis from hilar cholangiocarcinoma. Gut Liver 7: 234-238.
- Naitoh I, Nakazawa T, Ohara H, et al. (2009) Endoscopic transpapillary intraductal ultrasonography and biopsy in the diagnosis of IgG4- related sclerosing cholangitis. J Gastroenterol 44: 1147-1155.
- Kawakami H, Zen Y, Kuwatani M, et al. (2010) IgG4-related sclerosing cholangitis and autoimmune pancreatitis: histological assessment of biopsies from Vater’s ampulla and the bile duct. J Gastroenterol Hepatol 25: 1648-1655.
- Kamisawa T, Tu Y, Nakajima H, et al. (2006) Sclerosing cholecystitis associated with autoimmune pancreatitis. World J Gastroenterol 12: 3736-3739.
- Leise MD, Smyrk TC, Takahashi N, Sweetser SR, Vege SS, et al. (2011) IgG4-associated cholecystitis: another clue in the diagnosis of autoimmune pancreatitis. Dig Dis Sci 56: 1290-1294.
- Kamisawa T, Nakazawa T, Tazuma S, Zen Y, Tanaka A, et al. (2019) Clinical practice guidelines for IgG4-related sclerosing cholangitis. J Hepatobiliary Pancreat Sci 26: 9-42.
- Gaillard F, Glick Y (2022) Cholangiocarcinoma. Reference article, Radiopaedia.org 2022.
- Kamisawa T, Tabata T (2011) IgG4-related sclerosing cholangitis. Ann Hepatol 10: 552-555.
- Oseini AM, Chaiteerakij R, Shire AM, Ghazale A, Kaiya J, et al. (2011) Utility of serum immunoglobulin G4 in distinguishing immunoglobulin G4-associated cholangitis from cholangiocarcinoma. Hepatology 54: 940-948.
- Nakazawa T, Naitoh I, Hayashi K, Miyabe K, Simizu S, et al. (2013) Diagnosis of IgG4-related sclerosing cholangitis. World J Gastroenterol 19: 7661-7670.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.