Hydatid Disease of the Iliopsoas Muscle: Case Report
by Ricardo Raniero1*, Bruno Henrique Pieruci Florenzano1, Fábio Goussain Labat2,Gabriel Guimarães Rezende3, Gabriel Ricardo Herênio de Melo4, Giovanna Yumi Asanome Galli4,Ivana Maria Herênio dos Santos5,Jessyca Nobre Silva6, João Ricardo Herênio de Melo5, Laís Cavalcante Alves Cordeiro6, Layla Curi Ferrari Pinheiro de Barros3, Maressa Martins Costa Duarte3, Matheus Henrique Ferreira de Campos2, Natália Silveira Dionísio3, Victor Menezes da Cunha2, Thaís Helena Afonso Magalhães Pereira7, Viviane Aparecida Amaro Morceli3
1Departament of Surgery, Leforte Hospital, São Paulo, São Paulo, Brazil
2Departament of Surgery, Hospital Complex from Mandaqui, São Paulo, São Paulo, Brazil
3Departament of Medicine, Nove de Julho University, São Paulo, São Paulo, Brazil
4Departament of Medicine, Anhembi Morumbi School of Medicine, São Paulo, São Paulo, Brazil
5Departament of Medicine, Faculty of Medical Sciences of Pará, Marabá, Pará, Brazil
6Departament of Medicine, Municipal University of São Caetano do Sul, São Paulo, São Paulo, Brazil
7Departament of Medicine, College of Americas, São Paulo, São Paulo, Brazil
*Corresponding author: Ricardo Raniero, Departament of Surgery, Leforte Hospital, São Paulo, São Paulo, Brazil
Received Date: 02 February 2025
Accepted Date: 06 February 2025
Published Date: 10 February 2025
Citation: Raniero R, Labat FG, Rezende GG, de Melo GRH, de Barros LCFP, Duarte MMC, et al. (2025) Hydatid Disease of the Iliopsoas Muscle: Case Report. J Surg 10: 11250 https://doi.org/10.29011/2575-9760.011250
Summary
This study aims to document, through a case report, the occurrence of Hydatid Disease with parasitic infestation in an atypical location, specifically in the right psoas muscle. Hydatid disease has a global annual incidence rate of 1 to 200 per 100,000 [1], with higher prevalence in regions with sheep and cattle farming, such as Mediterranean countries, the Middle East, Eastern Europe, and South America. The patient in question is a 26-year-old man from Pakistan, residing in Brazil. This is a cross-sectional observational and descriptive study, conducted through the analysis of medical records and interviews with the patient and close family members. The individual presented with severe abdominal pain and weakness, with a computed tomography (CT) of the abdomen suggesting an abscess in the right psoas muscle. The investigation was conducted in the General Surgery ward of the General Hospital of Mandaqui Hospital Complex in São Paulo, maintaining confidentiality of the data. Treatment consisted of surgical removal of the hydatid cysts, followed by clinical therapy with Albendazole.
Keywords: Abscess; Hydatid disease; Iliopsoas muscle; Surgery
Introduction
Echinococcosis, or hydatid disease, is a rare and endemic disease caused by infestation with parasites of the genus Echinococcus. There are two main forms: cystic (echinococcosis) caused by Echinococcus granulosus and polycystic, caused by E. vogeli and E. oligarthrus. The last proglottid of each worm matures to produce eggs that are released in the feces of carnivores into the external environment [2,3]. If the eggs are ingested by humans or intermediate hosts, they hatch in the intestine to release oncospheres that pass through the portal and lymphatic vessels and reach the liver, where they typically settle and develop into larvae (metacestodes or hydatid cysts); less frequently, they can also affect the lungs, brain, bones, or any other organ of the human or intermediate host [3-5]. The cysts are composed of two layers derived from the membrane: an inner, nucleated, germinative membrane, and an outer, acellular, laminated layer [6]. The immune system responds to the cyst by forming a fibrous, calcified capsule around it, which is the most frequently visualized layer in imaging studies [5].
According to the WHO, E. granulosus is endemic in areas of South America, Russia, Eastern Europe, the Middle East, and China. The incidence rates in humans range from 50 to 100 per 100,000 people per year. In some areas of South America, prevalence ranges from 20% to 95% [7]. Its symptoms manifest late due to the slow growth of the cysts. In general, it is asymptomatic, and its manifestations depend on the location and size of the cyst [7]. This study aims to present a case report of a Pakistani patient residing in Brazil who was infected with the parasite in the iliopsoas muscle and describe the clinical characteristics of presentation, diagnosis, treatment, and evolution during hospitalization.
Material and Methods
This is an observational, cross-sectional, and descriptive study with a quantitative approach in the form of a case report, conducted through the analysis of medical records and interviews with the patient, their spouse, and a close sibling. The patient is a young adult male, originally from South Asia, specifically Pakistan, and residing in São Paulo. The patient and their family members will be approached in a calm and welcoming manner in the hospital ward to explain how the case report will be conducted and which documents will be needed for data collection. During this conversation, consent for participation in the case report project will be requested. It will be emphasized that participation is entirely voluntary, and at any time, participants have the right to withdraw their consent and be excluded from the project, without any negative consequences or penalties.
Clinical Case
Patient A.G., 26 years old, presented with a one-month history of abdominal pain. A CT scan showed a multiloculated collection centered in the right iliac muscle, measuring 5.0 x 2.5 cm, suggesting an inflammatory process. Surgical intervention was recommended for drainage of an abscess in the iliopsoas muscle. A puncture was performed on the bulging in the right psoas muscle, resulting in immediate drainage of 20 ml of serous secretion. The patient was hospitalized in the ward and showed no significant complaints. He was discharged for outpatient follow-up. Upon return, the patient reported continued abdominal pain, and a new CT scan revealed a multiloculated collection measuring 3.0 x 4.0 x 7.2 cm. The patient was readmitted for further investigation and presented with pain during passive and active movement of the Right Lower Limb (RLL), accompanied by paresthesia for one week. Antibiotic therapy with tazocin and symptomatic treatment were started. No significant clinical improvement was observed, and the collection in the iliopsoas region persisted.
A new surgical approach was recommended for abscess drainage. Intraoperatively, after dissection to the right iliopsoas muscle (Figure 1), no inflammatory processes or collections were identified. In the lower third of the muscle, a softened cystic structure was found. During dissection, rupture occurred, releasing a large amount of hydatid cysts. A decision was made to manually remove all cysts and the capsule (Figure 2), followed by lavage with 3% sodium chloride solution.
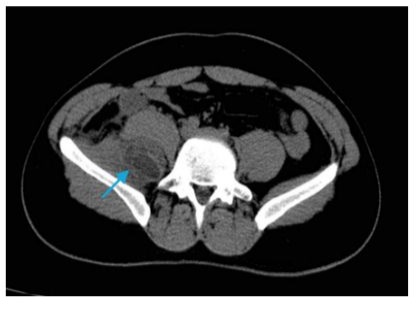
Figure 1: Tomography revealing the presence of a cyst in the iliopsoas muscle region (indicated by the blue arrow).

Figure 2: Post-surgical tomography, showing no cystic image. (indicated by the blue arrow).
After surgery, the patient was transferred to the ward and showed satisfactory progress. He was discharged. The patient returned for follow-up, reporting no symptoms and was being monitored by the infectious disease team at another institution due to hepatitis.
Results
The patient was referred to the Emergency Department of Hospital Mandaqui due to the presence of fever, lower abdominal pain, pain in the lower limbs, and significant functional impairment. The initial diagnosis indicated chronic hepatitis B, with positive serologies and no documented vaccination history. On December 29, 2023, the patient underwent a Computed Tomography (CT) scan (Figure 1), which revealed a multiloculated collection centered in the right iliac muscle, measuring 5.0 x 2.5 cm, suggestive of an inflammatory process or abscess. On January 5, 2024, a follow-up abdominal CT with contrast showed an increase in the collection, now measuring 6.0 cm in its largest axis. On January 6, 2024, an exploratory laparotomy was performed, with drainage of 20 mL of serous secretion from the right psoas muscle. The procedure included lavage with saline solution, placement of a tube -drain, and initiation of antibiotic therapy with 1g ceftriaxone and 500 mg metronidazole intravenously for 7 days. The culture of the abdominal fluid, collected on January 7, 2024, showed no bacterial growth.
On January 18, 2024, new CT scans showed the persistence of the multiloculated collection in the right psoas muscle, with enlargement of the right iliac muscle, which appeared heterogeneous due to the multiloculated formation, consistent with an inflammatory or infectious process, measuring approximately 7.2 cm in size. Despite initial treatment, on January 23, 2024, the patient returned to the hospital, referred to the Emergency Department, presenting with intense pain in the right lower limb, numbness, and functional limitation. Symptomatic treatment, hydration, and initiation of antibiotic therapy with piperacillin-tazobactam were administered. Additionally, Albendazole 400 mg/day was introduced as part of the pre- and postoperative clinical treatment, started on February 10, 2024, and maintained for 5 days. A new CT scan performed on January 24, 2024, showed that the collection in the right psoas remained stable, measuring 7.2 cm, with no significant changes in other findings. On January 25, 2024, the patient underwent serological tests. The VDRL test was non-reactive, indicating no active syphilis infection. The serologic test for hepatitis A showed elevated IgG antibody levels (9.17), suggesting prior exposure to the virus and acquired immunity, while the absence of IgM antibodies (0.17) indicated no acute infection. Regarding hepatitis B, the positive HBsAg test confirmed active infection with the virus. The presence of IgG anti-HBc antibodies, along with the absence of IgM anti-HBc antibodies, confirmed chronic infection.
The detection of reactive anti-HBe antibodies combined with a non-reactive HBeAg indicated a phase of lower viral replication and reduced infectivity. The absence of anti-HBs antibodies (<2.0 mIU/mL) demonstrated that the patient did not develop protective immunity, either through infection or vaccination, which was not documented. Rapid tests and serological tests for HIV were nonreactive, ruling out HIV infection.
On February 6, 2024, CT scans continued to show no significant changes, with the dimensions of the collection remaining virtually unchanged, measuring approximately 7.6 x 4.4 x 2.5 cm at its largest axes. During a new surgical approach, performed on February 14, 2024, a softened cystic structure was identified in the lower third of the right iliopsoas muscle via an extraperitoneal approach. During dissection (Figure 3), the structure ruptured, releasing a large amount of hydatid cysts (Figure 4). Manual extraction of all cysts was performed, followed by abundant lavage with 3% saline solution. The collected material was sent for histopathological analysis, which confirmed the presence of hydatid cysts (echinococcosis) in the right psoas.

Figure 3: Access to the right extraperitoneal region up to the iliopsoas muscle.
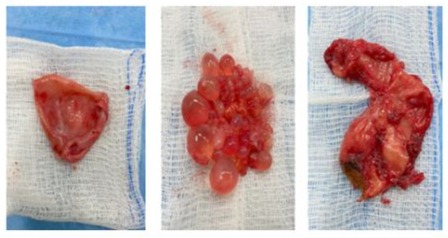
Figure 4: Hydatid cysts and hydatid capsules.
On March 8, 2024, a follow-up CT scan (Figure 2) showed a reduction in the multiloculated collection or abscess in the right iliac muscle and fossa, measuring approximately 6.4 x 4.7 x 2.6 cm, compared to previous measurements of 7.6 x 4.4 x 2.5 cm. Finally, on April 11, 2024, resolution of the collection in the right iliac muscle was observed, with only residual soft tissue densification remaining in the lower right quadrant of the abdominal cavity, consistent with residual changes or those related to prior surgical manipulation. The patient had a favorable clinical outcome after the diagnosis, with resolution of pain and progressive reduction in the tomographic findings, continuing follow-up with the infectious disease team.
Discussion
Cystic hydatidosis is one of the 20 neglected tropical diseases recognized by the World Health Organization (WHO) [8]. It is a notifiable disease in Argentina, Chile, Uruguay, and only one state in Brazil (Rio Grande do Sul). Therefore, there is underreporting, and the actual number of cases is uncertain. From January 2009 to December 2014, a total of 29,559 new human cases of CE were reported in Argentina, Brazil, Peru, Uruguay, and Chile [9]. This case highlights the complexity of diagnosing and treating a hydatid cyst involving the right iliopsoas muscle, an atypical site for the disease, which is usually associated with liver and lung involvement, accounting for at least 90% of cyst locations, depending on the country [10].
Initially, the clinical presentation of fever, lower abdominal pain, and functional impairment was suggestive of a psoas abscess. The absence of bacterial growth in cultures and the persistence of the multiloculated collection in imaging exams required careful diagnostic review. Confirmation of hydatid cysts during surgery reinforced the need to consider parasitic etiologies, particularly in patients with environmental or food exposure risks. Another important point is the patient’s lack of hepatitis B vaccination, a critical public health issue. This case emphasizes the importance of vaccination campaigns in at-risk populations and early detection of chronic hepatitis to avoid secondary complications. The coexistence of chronic hepatitis B added therapeutic challenges, including the monitoring of liver function and the choice of compatible antimicrobial agents. From a therapeutic perspective, exploratory laparotomy and initial drainage, followed by the administration of the antiparasitic Albendazole, proved to be effective strategies. A Chinese study with 15,289 surgical cases showed that 92% of patients needed only one surgical approach, 7% required two, 0.8% three, and 0.2% required four to eight operations [11]. Other studies with different groups of patients with cystic echinococcosis showed that after treatment with Albendazole, 48% of the 665 cysts disappeared, and 24% improved, while 28% of the 516 cysts disappeared and 30% improved after treatment with Mebendazole [12].
The use of hypertonic saline solutions during the surgical procedure is essential to avoid cyst dissemination and anaphylactic reactions due to ruptured cysts. Currently, a 20% hypertonic saline solution is recommended, which should be in contact with the cysts for at least 15 minutes. It should be avoided when there is communication between the cyst and the bile ducts, to prevent chemically induced sclerosing cholangitis [13].
Tomographic follow-up revealed progressive resolution of the collection, although with residual densification due to surgical manipulation and postoperative inflammatory response. The favorable clinical response after surgery and the reduction of lesions observed in the tomographies indicate that the adopted therapeutic approach was effective, despite the complexity of the case.
Conclusion
This case highlights the importance of accurate differential diagnosis, rigorous clinical surveillance, and appropriate treatment for complex infectious diseases such as echinococcosis. These diseases can mimic more common inflammatory processes but require a distinct therapeutic approach. The patient was initially diagnosed with a psoas abscess, but the persistence of the collection and the absence of bacterial growth in the exams led to a diagnostic reassessment, ultimately identifying hydatid cysts. The treatment consisted of surgical drainage and the administration of Albendazole, resulting in progressive resolution of the infection. Continuous follow-up, along with monitoring of liver function, is essential to ensure full recovery and prevent long-term complications. Furthermore, vaccination against hepatitis B and surveillance of parasitic diseases should be prioritized, especially in at-risk populations, to reduce the burden of neglected tropical diseases.
References
- Nunnari G, Pinzone MR, Gruttadauria S, Celesia BM, et al. (2012) Hepatic echinococcosis: Clinical and therapeutic aspects. World J Gastroenterol 18: 1448-1458.
- Martel G, Ismail S, Bégin A, Vandenbroucke-Menu F, Lapointe R (2024) Surgical management of symptomatic hydatid liver disease: experience from a Western centre. Can J Surg 57: 320-326.
- Galan LEB, Santos NM, Dantas DSM, Carbonell RCC, Araújo AMM, et al. (2022) HIDATIDOSE HEPÁTICA EM PACIENTE COM HEPATITE B: RELATO DE CASO, The Brazilian Journal of Infectious Diseases 26.
- Castro AR, Hyppolito EB, Valença-Júnior JT, Coelho GR, Garcia JHP (2022) ABCD Arq Bras Cir Dig. 2022.
- Wen H, Vuitton L, Tuxun T, Li J, Vuitton DA, et al. (2019) Echinococcosis: Advances in the 21st Century. Clin Microbiol Rev 32: e00075-18.
- Pakala T, Molina M, Wu GY (2016) Hepatic Echinococcal Cysts: A Review. J Clin Transl Hepatol 4: 39-46.
- Obrigon AM, Rangel MG, de Camargo Traldi MC (2018) Hidatidose pulmonar e hepática com múltiplos cistos: um relato de caso 2018.
- World Health Organization (2020) Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021-2030. Geneva: WHO 2020.
- Pavletic CF, Larrieu E, Guarnera EA, Casas N, Irabedra P, et al. (2017) Cystic echinococcosis in South America: a call for action 2017.
- Eckert J, et al. (2001) WHO/OIE manual on echinococcosis in humans and animals: a public health problem of global concern. World Organisation for Animal Health 2001.
- Menghebat L, Jiang L, Chai J (1993) A retrospective survey for surgical cases of cystic echinococcosis in the Xinjiang Uygur Autonomous Region, PRC (1951-90). In Compendium on cystic echinococcosis with special reference to the Xinjiang Ugur Autonomous Region, the People’s Republic of China (F.L. Andersen, J. Chai & F. Liu, eds). Brigham Young University, Print Services, Provo, Utah 1993: 135-145.
- Horton RJ (1997) Albendazole in treatment of human cystic echinococcosis: 12 years of experience. Acta trop 64: 79-93.
- World Health Organization (WHO) (1996) Guidelines for treatment of cystic and alveolar echinococcosis. WHO Informal Working Group on Echinococcosis. Bull. WHO 74: 231-242.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.