How to Implement Recommendations on Multidisciplinary Heart Failure Management Program into Practice? Lithuanian Experience
by Jelena Čelutkienė1*, Edita Lycholip1,2, Greta Burneikaitė1,2, Gintarė Karaliūtė1,2, Laura Kalakauskaitė1,2, Daiva Kriukelytė3, Jūratė Barysienė1,2, Diana Žaliaduonytė4, Aušra Kavoliūnienė4, Roma Puronaitė1,2,5, Vaida Morkvėnienė6, Algimantas Girčys6, Lukas Žilinskas6, Anna Stromberg7,8, Tiny Jaarsma7,9
1Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
2Vilnius University Hospital Santaros klinikos, Vilnius, Lithuania
3Department of Nursing, Faculty of Nursing, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
4Cardiology Department, Medical Academy, Lithuanian University of Health Sciences, Kaunas, Lithuania
5Institute of Data Science and Digital Technologies, Faculty of Mathematics and Informatics, Vilnius University, Vilnius, Lithuania
6National Health Insurance Fund under the Ministry of Health, Vilnius, Lithuania
7Division of Nursing, Department of Health, Medicine and Caring Science Studies, Linkoping University, Linköping, Sweden
8Department of Cardiology, Linkoping University, Linköping, Sweden
9Julius Center, University Medical Center Utrecht, Utrecht, the Netherlands
*Corresponding author: Jelena Čelutkienė, Institute of Clinical Medicine, Faculty of Medicine, Vilnius University, Vilnius, Lithuania
Received Date: 15 November, 2025
Accepted Date: 24 November, 2025
Published Date: 28 November, 2025
Citation: Čelutkienė J, Lycholip E, Burneikaitė G, Karaliūtė G, Kalakauskaitė L, et al. (2025) How to Implement Recommendations on Multidisciplinary Heart Failure Management Program into Practice? Lithuanian Experience. J Community Med Public Health 9: 545. https://doi.org/10.29011/2577-2228.100545
Abstract
Aims: Despite clear guideline recommendation to involve Heart Failure (HF) patients into Multidisciplinary Programmes (MP), availability of this specialized care remains insufficient throughout European countries. The aim of this study is to analyse the process of establishment, and Quality Indicators (QIs) of Heart Failure Multidisciplinary Programme (HF-MP) in Lithuania. Methods and Results: We conducted a retrospective analysis of the requisites, steps of initiation and development of HF-MP as a national service reimbursed since 2016. HF-MP is structured as 4 encounters with a specialized HF team during 1 year after HF decompensation. Based on the National Health Insurance Fund (NHIF) administrative data we present the impact of HF-MP on cardiovascular readmissions, survival, and ICD implantations in 2018-2022. Aggregated 2018 – 2022 data from the NHIF showed that the odds for 1-year survival were 2.4 – 2.9 times higher in HF-MP cohort compared to usual care (UC), while the chances to survive without readmissions were 1.3 – 1.7 times greater than with UC. Health-related quality of life, index of self-care and 6 min walk test had improved significantly at the last visit of HF-MP service (p<0.001). Conclusion: Sharing practical experience from HF clinics in Sweden and HF recommendations help to effectively implement HF multidisciplinary programmes in the national context. HF care quality indicators contribute to further reduction of morbidity, early mortality and improvement of quality of life of patients with heart failure.
Keywords: Heart failure; Heart failure management plan; Heart failure clinic; Heart failure nurse; MULTI-disciplinary program
Introduction
The prevalence of known heart failure (HF) is 1 to 4% in the adult population of the western world [1] and reaches 3.1% in Lithuania [2]. The rate of HF rehospitalizations in Lithuania remains unacceptably high: among patients admitted to tertial hospitals with acute HF, 21%, 39% and 54% of them are repeatedly hospitalized within 1, 3 and 6 months, respectively [3]. We showed that each rehospitalization increases the risk of death by 3-4 times [3]. In 2016, approximately 23.6 million euros were spent on inpatient treatment of patients with acute HF in Lithuania., making the disease a massive burden for the healthcare system [4]
Although it is widely recognized that the best treatment results can be achieved through meticulous guidelines implementation by specialized care teams, however, in many European countries, there is still a shortage of HF multidisciplinary programmes (HF-MP) and HF nurses. Studies performed in different countries and health care systems [5-11] have proved that the frequency of readmissions decreases when the specialized nursing staff is involved in a multidisciplinary HF-MP after discharge. A systematic review and meta-analysis of randomized controlled trials found that nurse-led interventions contribute to the reduction in hospital readmissions, cost-benefit, higher patient functioning, and improved quality of life (QoL) [12-14]. Based on this evidence, the European Society of Cardiology (ESC) highly recommends (recommendation class I, level of evidence A) that HF management be provided in the multidisciplinary program [15].
The aim of this study is to analyse the establishment process, status, and Quality Indicators (QIs) of HF-MP in Lithuania, as well as to demonstrate its impact on patient survival using administrative data.
Materials and Methods
Study design
We retrospectively analysed the initiation, organization, and delivery of a national HF-MP service in a public healthcare system. We identified 8 requisite steps in the establishment of HF-MP:
- Gaining experience – meetings and documents of the Heart Failure Association of the ESC and official visit to Linköping University.
- Development of education programmes for HF nurses and HF cardiologists.
- Compiling the HF-MP service design, indications, and quality indicators.
- Completing the decree by the Minister of Health.
- University-based training of HF specialists.
- Initiation phase of HF-MP service with early adopters.
- Establishment of HF-MP quality indicators (QIs).
- Implementation of HF-MP investment project with service expansion.
In Lithuania HF-MP service is specifically designed for patients discharged from the hospital after HF exacerbation, with ICD-10 (the International Classification of Diseases, Tenth Revision) codes I50, I11.0, I13.0. The HF-MP consists of four visits to a specialized HF team within one year after HF decompensation (Figure 1).
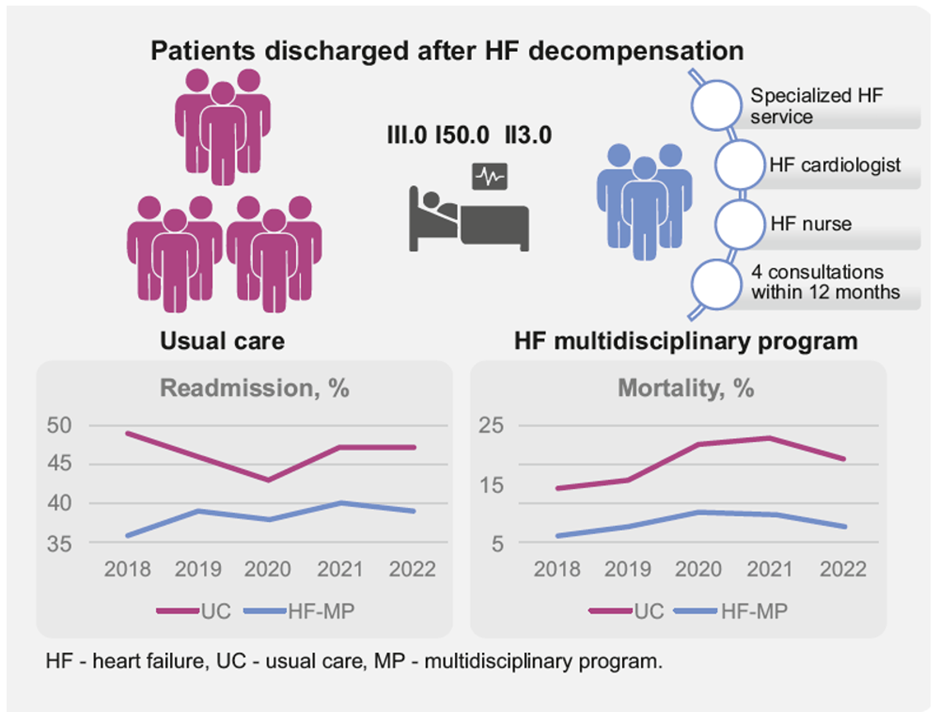
Figure 1: Heart failure management program and outcomes.
For the analysis of QIs based on hard outcomes, we used only aggregated data from nationwide registries, with no individual data. Hospitalisation, mortality and outpatient HF-MP encounters data from 1 January 2018 to 31 December 2022 were obtained from the National Health Insurance Fund (NHIF) and Compulsory Insurance Information System SVEIDRA. Data on rehospitalizations included admissions for any cardiovascular reasons (ICD-10 codes I00-I99). Use of Implantable Cardioverter-Defibrillators (ICDs) was identified using the ACHI codes (648, 653); because we only had access to administrative records at the national level, it was not possible to calculate the use of resynchronization therapy due to the lack of ACHI codes. Aggregated data on outcomes for QIs were obtained from the NHIF comparing two groups of patients: those who underwent specialized HF-MP and patients who received usual care (UC) provided by general practitioners or general cardiologists. Patients referred to inpatient palliative care or nursing facilities during 1 year after active treatment (as having a very poor prognosis and not eligible for HF education) and those admitted with acute coronary syndrome (I21-22) or acute cerebrovascular disease (I60-64) (as a reason for admission other than HF) were excluded from the analysis.
Statistical analysis
Pearson’s chi-square test was used to analyse the impact of HF-MP on aggregated data of readmissions, survival and ICD implantations. Patient-reported outcomes (assessed with the European Heart Failure Self-Care Questionnaire and Minnesota Quality of Life Questionnaire) and functional capacity assessed with the 6-minute walk test (6MWT) were available at one center of Vilnius University Hospital Santaros Klinikos. The Shapiro-Wilk normality test was used to test the normal distribution of the scores of questionnaires and the 6MWT data. The non-parametric Wilcoxon signed-rank test was used to compare the results of the first and last visits. A p-value < 0.05 was considered statistically significant.
Results
Gaining experience – meetings and documents of the Heart Failure Association of the ESC and visit to Linköping University
The Lithuanian Society of Cardiology (LSC) HF working group of the has set a goal to establish a network of HF clinics staffed by multidisciplinary teams of specially trained medical professionals, in line with the ESC recommendation. The HFA’s standards of care stipulate that 25% of cardiologists in tertiary care centres should have HF expertise and that each hospital should aim to achieve a rate of 1 HF nurse per 100,000 population [16]. In 2015, in cooperation with the Ministry of Health of the Republic of Lithuania, a delegation of medical professionals headed by the Minister Rimantė Šalaševičiūtė, accompanied by Vilnius University professors Aleksandras Laucevičius and Jelena Čelutkienė, visited the HF Clinic of Linköping University Hospital. This clinic is the first nurse-led HF clinic not only in Sweden, but also in the rest of Europe. Professors Anna Stromberg and Tiny Jaarsma and the HF team at Linköping university hospital shared their knowledge in the organization of nurse-led HF clinics and the role of nurses in HF-MP service.
Development of Education Programmes for HF Nurses and HF Cardiologists
Specialised educational programs for cardiologists and nurses were developed by HF experts in Vilnius University (VU) and Lithuanian University of Health Sciences (LUHS). The 288-hour postgraduate course “Specialised Nursing Care of HF Patients” provides nurses with the knowledge they need to work as a team with HF cardiologists to provide evidence-based, high-quality care. This program is based on the HF nurse curriculum (17), ESC Guidelines for diagnosing and treating acute and chronic heart failure [15] and practical recommendations on self-care management of HF from the Patient Care Committee of the HFA. The role of HF nurses includes patient education, assessment of patient status and treatment effect to participate in subsequent clinical decision making in the management of HF (Supplementary Table 1).
|
Patient health status assessment |
- Takes medical history - Assesses patient symptoms - Assesses main heart failure signs -Assesses everyday activities (exercise tolerance expressed in METs) - Measures arterial blood pressure, heart rate, weight and waist circumference - Administers and evaluates blood tests - Performs lung ultrasound (for pleural effusion and B lines) and bioimpedance Cardiography. |
|
Patient education |
- Interviews the patient and evaluates the patient awareness of heart failure - Assesses patient education needs - Creates a plan of educational sessions - Performs patient and his/her family members education using visual aids and methodical material - Evaluates knowledge and skills acquired in previous education sessions. |
|
Other functions: |
- Performs a 6-minute walking test - Reports patient data to HF cardiologist, and discusses the patient condition and helps to draft a plan for further care - Organizes and plans further care. |
Supplementary Table 1: Procedures performed by HF nurses.
The 72-hour postgraduate program “Heart Failure Diagnostics, Treatment and Outpatient Management” is designed to certify specialized HF cardiologists to develop personalized treatment plans, up-titrate medications and identify indications for non-pharmacological therapies. The regulative order states that certification of HF specialists must be renewed every five years [18,19].
Compiling the HF-MP Service Design, Indications, and Quality Indicators
The working group, formed by the Ministry of Health, designed the protocol of the HF-MP service in Lithuania based on ESC HF guidelines and recommendations. Patients after hospitalisation due to HF decompensation are referred to the specialised HF-MP service by cardiologists, internists, or general practitioners. Patients with HF are offered up to 4 consultation services within 12 months from the most recent inpatient treatment due to HF deterioration.
Completing the Decree by the Minister of Health
In 2015, the Minister of Health issued an order “The requirements for provision of specialized care that includes patient education to individuals with heart failure by HF cardiologist and HF nurse”, which entered into force at the beginning of 2016 [20]. It defines the scope of service, the content of education, requirements for certification of specialists and documentation of visits. Consultation services are financed from the Compulsory Health Insurance Fund budget in accordance with the legislation of the Republic of Lithuania.
University-based training of HF specialists
In 2016 the first 27 cardiologists and 28 nurses completed courses for HF professionals in two universities. As of the end of 2023, there were 96 fully trained specialised nurses and 81 HF cardiologists in Lithuania (general country population is about 2.8 million people) (Figure 2).
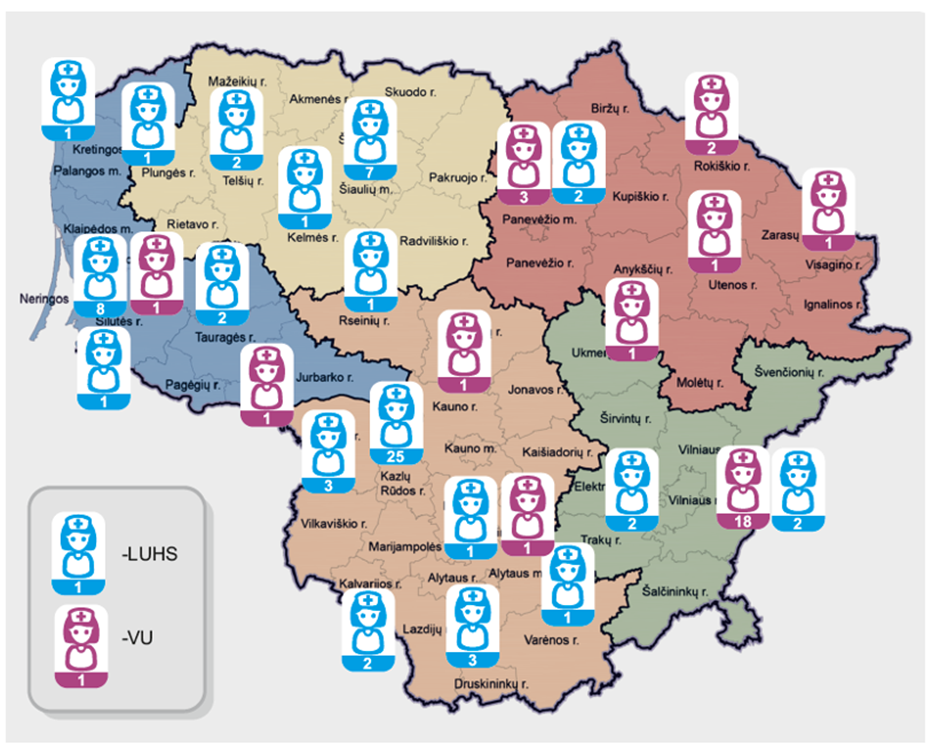
Figure 2: Specialised heart failure nurses who received training at Vilnius University (VU) and at the Lithuanian University of Health Sciences (LUHS) in 2023. In Lithuania, HF-MP services are provided in 5 districts.
The training was based on the ESC guidelines, HFA recommendation documents, knowledge of frequent comorbidities and theories of adult education [17,21-24].
Initiation phase of HF-MP service with early adopters
From mid-2016 to the end of 2022, 3,168 patients received specialised HF-MP services, with 12 HF clinics providing 6,965 encounters (Figure 3A). In 2019, the majority (88%) of all consultations were conducted in five out of twelve healthcare facilities (Figure 3B). Due to the COVID pandemic, access to healthcare services was limited, resulting in a reduction in the number of HF consultations in 2020. Table 1 shows the proportion of patients involved in HF-MP and rate of survival, readmissions and ICD implantations compared to usual care.
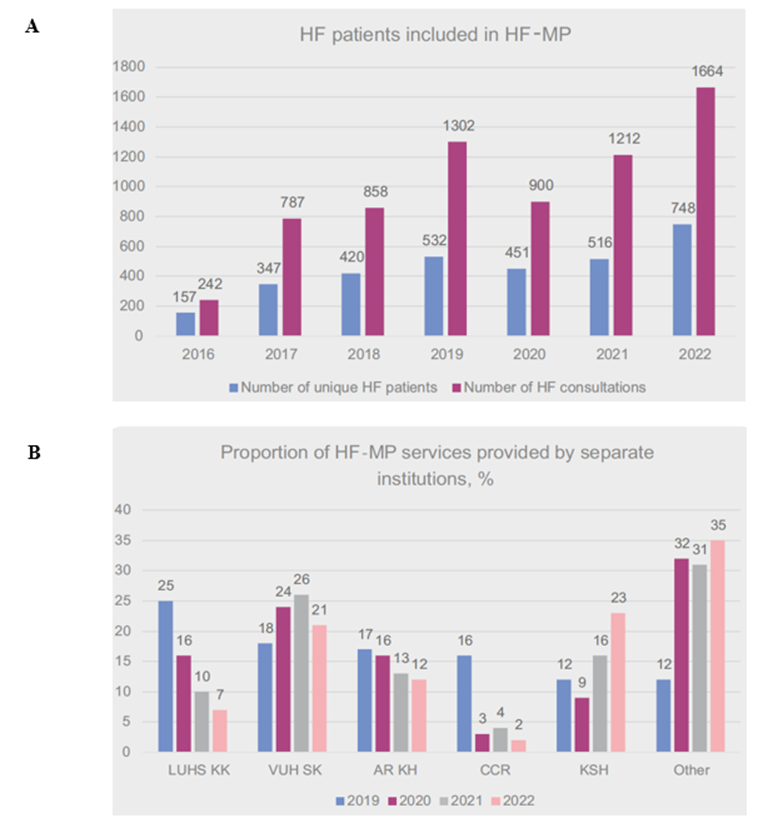
Figure 3: Dynamics of heart failure management program services in Lithuania (2016 – 2022). HF – heart failure, HF-MP – heart failure management program, LUHS KK – Lithuanian University of Health Sciences Kauno klinikos, VUH SK – Vilnius University Hospital Santaros klinikos, AR KH – Alytus region S. Kudirka Hospital, CCR – Clinic of Cardiology and Rehabilitation, KSH – Klaipeda Seamen’s Hospital. A. Number of HF patients included in heart failure management program. B. HF-MP services provided by institution.
|
All patients discharged after AHF, N |
Patients involved in HF-MP, N |
Patients referred to HF-MP within 30 d., N (%) |
Survival without readmissions in HF-MP vs UC, OR (CI) |
Overall survival in HF-MP vs UC, OR (CI) |
Chance to receive ICD in HF-MP vs UC, OR (CI) |
|
|
2018 |
26,993 |
317 |
80 (25) |
1.7 (1.4-2.1)* |
2.6 (1.6-4.2)* |
19.0 (7.8-46.5)* |
|
2019 |
26,241 |
336 |
90 (27) |
1.4 (1.1-1.7)** |
2.9 (2.8-4.6)* |
7.8 (2.8-21.9)* |
|
2020 |
19,009 |
259 |
61 (24) |
1.3 (1.0-1.6) |
2.4 (1.6-3.6) |
n.a. |
|
2021 |
17,486 |
368 |
101 (27) |
1.3 (1.1-1.6)*** |
2.7 (1.9-3.8)* |
n.a. |
|
2022 |
20,192 |
534 |
181 (34) |
1.4 (1.2-1.7)* |
2.8 (2-3.8)* |
n.a. |
|
*p<0.001, **p=0.03, ***p=0.035 Pearson’s chi-square test was used to calculate Odds Ratio (OR); no data were available for ICD in 2020-2022 HF-MP: Heart Failure Management Program, ICD: Implantable Cardioverter Defibrilator, UC: Usual Care. |
||||||
Table 1: The proportion of patients involved in specialized HF-MP service and rate of readmissions, survival and ICD implantations in 2018-2022 compared with usual care.
Establishment of HF-MP quality indicators
In 2020, following an exploratory analysis of clinical outcomes from initial HF-MP encounters, the Ministry of Health working group developed quality indicators to assess the effectiveness of specialised HF care (Supplementary Table 2). The QIs included:
- timing of the first HF-MP visit (target visit within 30 days after discharge), service completeness (all four HF visits within 1 year), and natriuretic peptide testing.
- nationwide proportion of patients receiving HF-MP and number of patients managed at each HF clinic.
- 1-year mortality rate, number of CV readmissions, ICD implantations, and improvement in quality of life, self-care skills, and functional capacity [25]
|
No. |
Indicator description |
Target value of the indicator |
|
1. |
Proportion of HF patients who received the service out of all discharged after decompensation HF patients (%) |
Observation of service intensity |
|
2. |
Patients with HF who did not receive service and died [2] within 12 months from the provision of inpatient services for active treatment, share of all HF patients (%) |
Indicators for comparison |
|
3. |
In patients with HF who received service 12 – month death rate after HF hospitalization (%) |
Not more than 7 % - outcome measure |
|
4. |
Proportion of all patients who did not receive the service and who were re-hospitalized for inpatient active treatment (diagnosis I00−I99) within 12 months after the provision of inpatient services, (%) |
|
|
5. |
The proportion of all patients who received the service and who were re-hospitalized for inpatient active treatment (diagnosis I00−I99) within 12 months after the provision of inpatient services, (% ) |
Not more than 36 % |
|
6. |
Proportion of HF patients with implanted defibrillators out of all HF patients who received HF service (%) |
Not less than 2 % |
|
7. |
Proportion of all HF patients who received the service and who had been tested for natriuretic peptides at least 2 times, out of all HF patients who received the HF service (%) |
Not less than 30 % - process indicator |
|
8. |
Proportion of all HF patients with a self - care score difference improvement of at least 10 in the first and last consultation according to the European Self - Care Questionnaire for Heart Failure (%) |
At least 60 % - outcome measure |
|
9. |
Proportion of all HF patients who received the service and whose quality of life index according to the Minnesota Quality of Life Questionnaire decreased improved by at least 10 points during the first and last consultation, out of all HF patients who received the service (%) |
At least 55 % - outcome measure |
|
10. |
Proportion of all HF patients who received the service and whose 6-minute walk test result increased by at least 30 meters during between the first and last consultation (%) |
At least 40 % - outcome measure |
|
11. |
HF patients who received the service timely, within 30 days after hospitalization or diagnosis of HF (for the first time), out of all HF patients who received the service (%) |
At least 40 % - process indicator |
|
12. |
Proportion of HF patients who received fulfilled services all 4 times visits out of all HF patients who received the service (%) |
At least 30 % - process indicator |
|
13. |
Number of patients with HF who were provided with a service in one of the HF clinics during one calendar year. |
At least 100 patients - process indicator |
Supplement Table 2: Indicators of HF-MP service availability and quality.
The choice of QIs was motivated by the absence of a dedicated HF registry in Lithuania and the lack of systematic data on HF medications and resynchronization therapy; therefore, variables available in the administrative database were used, supplemented by patient-reported outcomes that were prospectively collected by HF nurses.
The analysis revealed significantly lower one-year readmission and mortality rates among patients receiving HF-MP services compared to those receiving usual care (Table 1, Figure 4). Table 2 represents the single-centre results from VUH SK, showing positive changes in patient-reported outcomes and functional capacity.
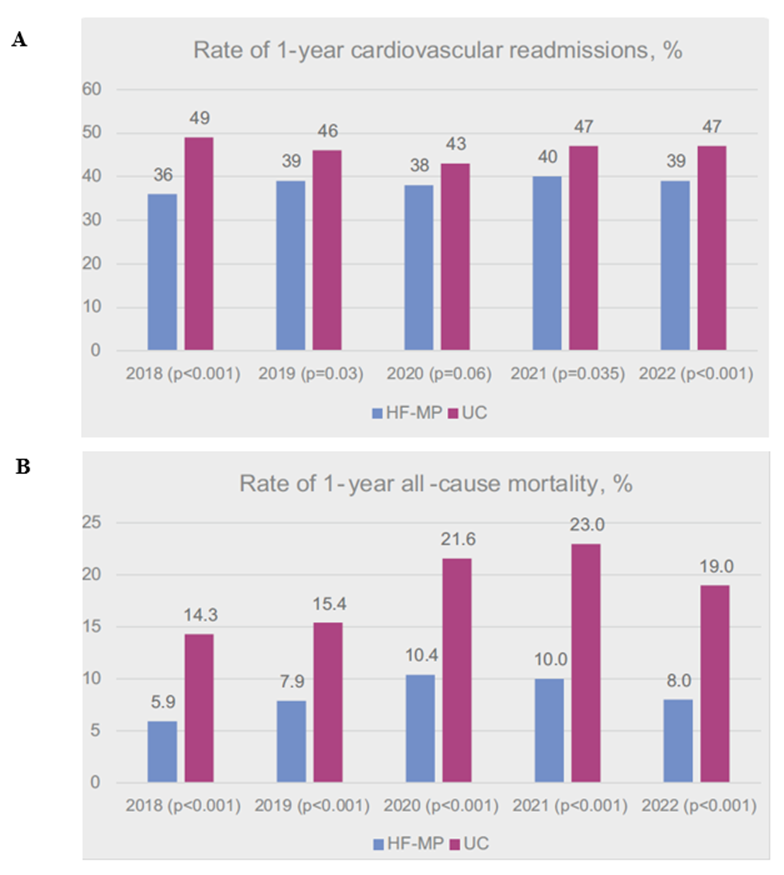
Figure 4: Readmission and mortality rates. A. Readmission rates of patients receiving specialized heart failure services (HF-MP) compared to patients receiving usual care (UC). B. Mortality rates of patients receiving specialized heart failure services (HF-MP) compared to patients receiving usual care (UC).
|
Year |
Number of patients |
First visit score, median (Q1;Q3) |
Last visit score, median (Q1;Q3) |
Average change (SE) |
Target value of the indicator |
Number of patients with target reached, N (%) |
|
|
MLHFQ score |
2021 |
67 |
39 (22;50) |
18 (13;32) |
-15.0 (1.8)* |
At least 55 % improved by at least 10 points |
37 (55.2) |
|
2022 |
69 |
35 (15;52) |
15 (9;25) |
-16.7 (2.4)* |
42 (60.9) |
||
|
EHFScBs score |
2021 |
67 |
27 (24;35) |
17 (15;20) |
-11.5 (1.0)* |
At least 60 % improvement of at least 10 |
39 (58.2) |
|
2022 |
69 |
28 (21;37) |
16 (13;20) |
-11.6 (1.2)* |
38 (55.1) |
||
|
6MWT, m |
2021 |
60 |
390 (328;470) |
420 (355;511) |
34.5 (7.4)* |
At least 40 % increased by at least 30 meters |
33 (55.0) |
|
2022 |
61 |
390 (330;450) |
420 (375;480) |
47.3 (5.8)* |
41 (67.2) |
||
|
EHFScBs - European Self-care Behaviour scale; MLHFQ - Minnesota Living with Heart Failure Questionnaire. 6 MWT - 6-minute walk test. * - p value <0.001. |
|||||||
Table 2: Dynamics of quality of life score, self-care score and the 6-minute walk test at VU Hospital Santaros Clinics (2021-2022).
Implementation of HF-MP Investment Project with Service Expansion
Positive quality assessment results have contributed to the expansion of specialized HF-MP services. This was achieved through a public investment program funded by the European Union (EU) for the 2014–2020 period, with a total allocation of 2.7 million euros [26].
The Minister of Health has issued an order to allocate these funds to improve the availability of specialized HF services with the aim of reducing morbidity and early mortality among HF patients. Funded activities included training of HF specialists and the purchase of impedance cardiographers, echocardiographers and other medical equipment [26]. The result of the program was the establishment of 35 specialized HF clinics in Lithuania. Priority was given to regions where the cardiovascular mortality rate exceeds the national average.
Discussion
Despite the ESC guidelines for multidisciplinary care for patients with HF [15], significant gaps in real-world practice remain, contributing to high rates of hospitalisations and mortality. Patients admitted with HF have a 20-30% risk of dying within a year [27]. The 2024 American College of Cardiology (ACC) expert consensus decision pathway on patients hospitalized with HF emphasizes the need for continuation of care early after discharge and the critical importance of up-titration of neurohormonal modulation along with education of patients, families and caregivers [28].
The recent multinational STRONG-HF study demonstrated that patient outcomes can be significantly improved by high intensity care, including an up-titration of treatments to 100% of recommended doses within 2 weeks of discharge and four scheduled outpatient visits over the next 2 months. After 180 days, the risk of HF readmission or all-cause death was 8.1% lower in the high intensity care group than in usual care group (15.2% and 23.2%, respectively) [29].
However, many European countries lack a structured HF post-discharge management. The independent interdisciplinary Heart Failure Policy Network conducted a comprehensive analysis of national policies regarded to heart failure across 11 European countries: Belgium, Denmark, England, France, Germany, Greece, Ireland, Italy, Poland, Portugal, and Spain. This analysis identifies key gaps in existing policies and shows barriers such as insufficient funding, poor continuity of care and limited access to HF specialists that many European countries face [30,31]. Only 3 of the 11 countries have dedicated strategy on HF, and in the others, the plans may need to be updated, lack funding or may have stalled [30]. Despite evidence that HF nurse-led programs reduce hospital admissions [13,14,16,32], the role of HF nurses is formally accredited only in England, Germany, and Ireland.
In Central and Eastern Europe, only four out of the 11 countries (Czechia, Hungary, Lithuania, and Serbia) have developed national HF strategies. Furthermore, only Hungary and Lithuania have patient pathway programs in place, while most countries in the region lack coordinated care programs that include HF specialists and nursing support. Additionally, these countries do not have long-term national HF registries; instead, they rely on administrative databases [33].
Despite EU investment funds aimed at improving access to HF treatment in order to reduce morbidity and early mortality in the Lithuanian population, this funding did not reach healthcare institutions in a timely manner. The limited interest of politicians and hospital administrators to such kind of activities along with substantial bureaucracy are the biggest obstacles to the faster development of services. As a result, many Lithuanian institutions that trained specialists did not start providing HF-MP. Still, only a small sample of discharged HF patients undergo encounters with the specialized team in Lithuania. Furthermore, due to the COVID-19 pandemic, the European Union investment action program has come to a near standstill for some time. In addition, the development of the service was negatively affected by such factors as the low initial reimbursement of the service set by the NHIF, high workload, and shortage of nursing staff. Thus, by the end of 2021, there were only 12 HF-MP facilities in 8 cities, with more than half of them providing only a few specialized consultations. Some of HF nurses either do not provide services at all or do that only a small part of their working time. Although slowly, the number of specialized HF consultations in Lithuania is growing. According to regulations adopted by the Ministry of Health in 2020, each institution providing specialized service must consult at least 100 patients per year (meaning 400 consultations in total); in addition, the procedure for referral to HF specialists is simplified by including internists and general practitioners. These measures should increase the availability of services while reducing the number of readmissions.
It is hoped that further investment in the training of specialized HF nurses will allow them to expand their competencies, gain higher professional status and receive a greater financial reward.
Lessons Learned
- International experience (in our case Swedish and Dutch) together with the published recommendations of the HFA of the ESC provide a solid basis for the establishment of a national heart failure management program.
- Advocating for specialized services and building up strategic relationships with healthcare policymakers are essential steps for developing and securing reimbursement for new care programs.
- Empowering nurses to provide independent patient counseling enhances patient satisfaction and strengthens collaboration between HF teams, patients, and caregivers. However, more comprehensive training programs and greater level of autonomy are needed.
- Clinical practice in Lithuania confirms that a multidisciplinary heart failure management program significantly improves clinical outcomes compared to usual care.
Conclusion
A specialized multidisciplinary heart failure management program has been successfully implemented in Lithuania under the guidance of international experts. Although a significant number of specialized heart failure nurses and cardiologists have been trained in recent years, the number of patients receiving specialized services remains quite low in Lithuania. Specialized services for heart failure patients are likely to become more accessible with the help of the European Union-funded investment action program 2014 - 2020.
References
- Groenewegen A, Rutten FH, Mosterd A, Hoes AW (2020) Epidemiology of heart failure. Eur J Heart Fail 22: 1342-1356.
- Seferovic PM, Vardas P, Jankowska EA, Maggioni AP, Timmis A, et al. (2021) The Heart Failure Association Atlas: Heart Failure Epidemiology and Management Statistics 2019. Eur J Heart Fail 23: 906-914.
- Cerlinskaite K, Mebazaa A, Cinotti R, Matthay M, Wussler DN, et al. (2021) Readmission following both cardiac and non-cardiac acute dyspnoea is associated with a striking risk of death. ESC Heart Fail 8: 2473-2484.
- Valstybine ligoniu kasa prie Sveikatos apsaugos ministerijos].
- Strömberg A, Mårtensson J, Fridlund B, Levin LA, Karlsson JE, et al. (2003) Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: results from a prospective, randomised trial. Eur Heart J 24: 1014-1023.
- Blue L, Lang E, McMurray JJ, Davie AP, McDonagh TA, et al. (2001) Randomised controlled trial of specialist nurse intervention in heart failure. BMJ 323: 715-718.
- You J, Wang S, Li J, Luo Y (2020) Usefulness of a Nurse-Led Program of Care for Management of Patients with Chronic Heart Failure. Med Sci Monit 26: e920469.
- Shojaee A, Nehrir B, Naderi N, Zareyan A (2013) Assessment of the effect of patient’s education and telephone follow up by nurse on readmissions of the patients with heart failure. Iran J Crit Care Nurs 6: 29-38.
- Stewart S (2012) Nurse-led care of heart failure: will it work in remote settings? Heart Lung Circ 21: 644-647.
- de Souza EN, Rohde LE, Ruschel KB, Mussi CM, Beck-da-Silva L, et al. (2014) A nurse-based strategy reduces heart failure morbidity in patients admitted for acute decompensated heart failure in Brazil: the HELEN-II clinical trial. Eur J Heart Fail 16: 1002-1008.
- Savarese G, Lund LH, Dahlström U, Strömberg A (2019) Nurse-Led Heart Failure Clinics Are Associated With Reduced Mortality but Not Heart Failure Hospitalization. J Am Heart Assoc 8: e011737.
- Cui X, Zhou X, Ma L le, Sun TW, Bishop L, et al. (2019) A nurse-led structured education program improves self-management skills and reduces hospital readmissions in patients with chronic heart failure: a randomized and controlled trial in China. Rural Remote Health 19: 5270.
- Rice H, Say R, Betihavas V (2018) The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Educ Couns 101: 363-374.
- Adib-Hajbaghery M, Maghaminejad F, Abbasi A (2013) The role of continuous care in reducing readmission for patients with heart failure. J Caring Sci 2: 255-267.
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, et al. (2021) 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42: 3599-3726.
- McDonagh TA, Blue L, Clark AL, Dahlström U, Ekman I, et al. (2011) European Society of Cardiology Heart Failure Association Standards for delivering heart failure care. Eur J Heart Fail 13: 235-241.
- Riley JP, Astin F, Crespo-Leiro MG, Deaton CM, Kienhorst J, et al. (2016) Heart Failure Association of the European Society of Cardiology heart failure nurse curriculum. Eur J Heart Fail 18: 736-743.
- Lainscak M, Blue L, Clark AL, Dahlström U, Dickstein K, et al. (2011) Self-care management of heart failure: practical recommendations from the Patient Care Committee of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 13: 115-126.
- Jaarsma T, Hill L, Bayes-Genis A, La Rocca HPB, Castiello T, et al. (2021) Self-care of heart failure patients: practical management recommendations from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 23: 157-174.
- V-1495 Del Lietuvos Respublikos sveikatos apsaugos ministro 2015 m. lapkricio 24 d. isakymo Nr. V-1330.
- McMurray JJV, Adamopoulos S, Anker SD, Auricchio A, Böhm M, et al. (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33: 1787-1847.
- Triposkiadis F, Giamouzis G, Parissis J, Starling RC, Boudoulas H, et al. (2016) Reframing the association and significance of co-morbidities in heart failure. Eur J Heart Fail 18: 744-758.
- van Deursen VM, Urso R, Laroche C, Damman K, Dahlström U, et al. (2014) Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail 16: 103-111.
- Tereseviciene M (2008) Suaugusiuju mokymasis. Andragogines veiklos perspektyva: mokslo studija. Kaunas: Vytauto Didžiojo universiteto leidykla.
- V-1495 Del Lietuvos Respublikos sveikatos apsaugos ministro 2015 m. lapkricio 24 d. isakymo Nr. V-1330.
- V-1062 Dėl 2014–2020 metų Europos Sąjungos fondų investicijų veiksmų programos 8 prioriteto “Socialinės įtraukties didinimas ir kova su skurdu” įgyvendinimo priemonės Nr. 08.1.3-CPVA-V-610 “Kraujotakos sistemos ligų gydymo ir diagnostikos paslaugų infrastruktūros gerinimas” projektų finansavimo sąlygų aprašo Nr. 2 patvirtinimo.
- Bozkurt B, Ahmad T, Alexander KM, Baker WL, Bosak K, et al. (2023) Heart Failure Epidemiology and Outcomes Statistics: A Report of the Heart Failure Society of America. J Card Fail 29: 1412-1451.
- Maddox TM, Januzzi JL, Allen LA, Breathett K, Brouse S, et al. (2024) 2024 ACC Expert Consensus Decision Pathway for Treatment of Heart Failure with Reduced Ejection Fraction: A Report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 83: 1444-1488.
- Mebazaa A, Davison B, Chioncel O, Cohen-Solal A, Diaz R, et al. (2022) Safety, tolerability and efficacy of up-titration of guideline-directed medical therapies for acute heart failure (STRONG-HF): a multinational, open-label, randomised, trial. Lancet 400: 1938-1952.
- The handbook. The Heart Failure Policy Network.
- The Health Policy Partnership. The Heart Failure Policy Network.
- Boyde M, Peters R, New N, Hwang R, Ha T, et al. (2018) Self-care educational intervention to reduce hospitalisations in heart failure: A randomised controlled trial. Eur J Cardiovasc Nurs 17: 178-185.
- Chioncel O, Čelutkienė J, Belohlávek J, Kamzola G, Lainscak M, et al. (2024) Heart failure care in the Central and Eastern Europe and Baltic region: status, barriers, and routes to improvement. ESC Heart Fail 11: 1861-1874.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.