How the Other Half Lives: Clinical Insights from a UK Resident Doctor Participating in an Outreach Medical Camp in Pakistan’s Thar Desert
by Syed Ammar Husain1* Kaim Bidiwala2, Moeez Shiraz3, John Anderson4
1Academic Foundation Year Two Doctor, Brighton and Sussex Medical School, UK
2UK NHS Pharmacist King’s College London, Guy’s Campus Great Maze Pond, London, UK
3Medical Student, DOW International Medical School Mission Road, New Labour Colony Nanakwara, Karachi, Pakistan
4Principal Lecturer, Department of Medical Education, MBBS Brighton and Sussex Medical School Watson Building, University of Brighton, Falmer, Brighton, UK
*Corresponding author: Dr Syed Ammar Husain, MBBS, Academic Foundation Year Two Doctor, Brighton and Sussex Medical School; ORCID 0000-0003-4564-3408; Email: S.husain1@uni.bsms.ac.uk
Received Date: 21 October 2025
Accepted Date: 27 October 2025
Published Date: 05 November 2025
Citation: Husain SA, Bidiwala K, Shiraz M, Anderson J (2025) How the Other Half Lives: Clinical Insights from a UK Resident Doctor Participating in an Outreach Medical Camp in Pakistan’s Thar Desert. Ann Case Report. 10: 2435. DOI:10.29011/2574-7754.102435
Introduction
Accessing basic healthcare is particularly difficult for people living in rural and isolated areas of the world… Most (70%) of Pakistan’s population live in areas with poor infrastructure, lack of medical professionals, and growing treatment costs [1]. South Sindh’s Thar Desert is well known for its extreme heat and humidity, inadequate government facilities and poor access to basic healthcare [2].
In October 2024 and February 2025, I (SYH) joined other volunteers in an international outreach “camp” providing medical care to underprivileged communities in the Thar Desert. The charity, ShareForCare UK, invited me to participate in the camp. It was planned with local healthcare practitioners (HCP) and community leaders - essential to avoid being seen to compete with existing service providers in an “imperialist” approach. I learned to identify problem areas and how to plan complementary services. The charity established a basecamp, a deprived neighbouring town to Thar Desert, for easier transport, storage, and deployment of satellite clinics.
Information about outreach camps were disseminated to the local ‘Thar’ community through village leaders, printed flyers and announcements in schools, community and health centres, to promote the free medical care provided.
My fellow volunteers were chosen to represent a multidisciplinary team that included medical students, nurses, juniors and specialist physicians, and administrative staff. Clinicians with ties to Pakistan and the UK contributed to the internationally diverse expertise. A pre-camp briefing outlined our roles, anticipated patient volumes, cultural and linguistic considerations, along with consultation and management protocols.
Local people were also involved in the camp’s planning. Their contributions spanned across volunteering to help with patient registration, triage stations and crowd management to maintain camp flow (Figure 1). Similar planning proved to be of success in the Hong Kong’s Kwun Tong Community Health Project in the 1970s. Through their collaborative approach, they demonstrated the importance of strong community partnerships for sustaining future outreach work [3].
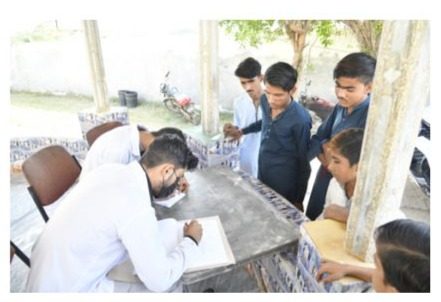
Figure 1: The local community health workers volunteering to help with patient registration and triaging to the appropriate speciality station
I gained approval from the charity trustee members for the use of non-identifiable data to be shared to provide insights for this article (See Appendix 1).
We adopted a collaborative autoethnographic approach 4 in which I wrote a detailed account of personal experiences and affective responses that served as primary date for thematic analysis [4,5].
Personal Observations
An estimated 2,000 patients attended two camps. Data from February 2025 camp assessed 1,047 patients from the local communities of the 1,047 patients, most (67%) were under the age of 35 and 28.6% of those were under the age of 18, with a nearequal gender split (See Appendix 1).
Patients were registered and triaged by nurses then directed to speciality stations. After their consultation, they collected prescribed medications from the pharmacy. The Nizamuddin Foundation Trust, a local pharmacy organisation, supported by dispensing the free medications. Clinicians requested laboratory, where necessary. These were organised through the Essa Laboratory in the camp.
The top five presenting complaints in the camp were ‘fever’ (21.4), ‘rash’ (14.8%), then other non-specific symptoms such as ‘malaise’, ‘body aches’ and ‘dizziness’ (6.4%). Twenty six percent were suspected to be ‘infectious and parasitic”, such as. as ‘Tuberculosis’, ‘Malaria’ and suspected ‘schistosomiasis’; 18.6% dermatological and the rest ‘non-specific’.
Almost half of all diagnoses were ‘unclassified’ with ‘non-specific’ symptoms such as headache, weakness or abdominal pain. Of the defined diagnoses, upper respiratory tract infections (7.9%) and gastric irritation (7.1%) were most prevalent. Nearly 1 in 10 specific cases were dermatological, such as skin infections, allergy, acne and a few more complex cases including ‘Ichthyosis’, ‘Leprosy’ and ‘Tuberculoid variety’.
The data also highlights cases of newly diagnosed and poorly controlled long-term medical conditions. These included ‘Hypertension’, ‘Asthma’, ‘Anaemia’, ‘Osteoarthritis’, ‘Diabetes’, ‘chronic kidney disease’, and ‘Depression/Anxiety’. These combined represent 15% of the patient population. There were some life-threatening medical problems - ‘Intussusception’, ‘hypertensive emergency’ and a ‘paediatric febrile seizure’ - requiring urgent review and transfer to nearby health units for timely management.
Key Lessons
My first outreach volunteering experience, six months after practicing as a new UK doctor, provided valuable insights and perspectives, working in different clinical and cultural environments. The transition from a highly structured, wellequipped, NHS to a remote, resource-limited region provoked different sets of challenges and ethical dilemmas to reflect upon.
Consultations often included family members, especially children (Figure 2). I was surprised at parents’ lack of basic child healthcare knowledge. In my consultations, I would also focus on teaching the parents about managing fever, good hydration and nutrition, along with awareness of ‘red’ flag’ signs in unwell children [6]. Nearly 30% of paediatric attendees had suspected anaemia or malnutrition. These challenges in childcare confirm a need for health education programmes.

Figure 2: A photograph of the volunteer doctors who were assigned to see patients in the ‘Paediatrics’ speciality station.
In the UK I had substantial encounters with patients who did not speak English - a significant barrier to effective communication. Tharipuri Institute nurses acted as interpreters to help international volunteers. However, I noted ‘nuances’ and ‘idioms’ were frequently ‘lost in translation’. Also, some ‘jargon’ in Dakti language misrepresented common symptom descriptions. For example, a patient told the interpreter “dil kamzor hai”, translating to “my heart feels weak”. This vague descriptor can be interpreted as a range of common symptoms – heartburn, chest pain, exertional breathlessness and even signs of decompensated heart failure, which could influence patient management. I believe this third layer of translation of the patient’s story, impacted on clinical decision-making. This also makes it more difficult for the patient to share sensitive information that could be vital.
Effective information and explanations are essential for promoting adherence and effectively treating issues [7]. However, this was hampered by communication barriers. Poor monitoring and restricted access to local pharmacies in these situations made things even more difficult.
Reflecting with the volunteer psychiatrist on our experiences, we concluded that a few patients recognised the impact their mental health has on their physical well-being. In the outreach setting, the psychiatrist noted underlying anxiety and depression that also contributed to the physical manifestations of their symptoms. I concluded that culture and poverty combined, perpetuated worsening mental health, resulting in a situation, which is replicated in underprivileged communities around the world, who suffer from underlying mental health issues that go untreated. The outreach camps served as an important opportunity to screen and treat mental health in rural communities [8].
The camp provided me an unparalleled opportunity to learn about a range of illnesses, seldom encountered in modern western medicine. Malaria, Schistosomiasis, viral hepatitis, pulmonary tuberculosis, and dermatological conditions like xeroderma pigmentosum, tuberous sclerosis, and allergic vasculitis were among the intriguing illnesses I encountered.
Clinical reasoning proved challenging when formulating a diagnosis, with no point-of-care tests and previous documents or history usually available in a western setting. Therefore, relying solely on my clinical history and examinations proved to be a challenging, but exceptional learning opportunity for me to develop confidence in my clinical reasoning and diagnostics.
The extreme temperatures (36-38°C) and humidity tested my resilience, focus, and concentration. Following advice from locals, I increased hydration, timely rest breaks, and paced myself. Other workers were supportive too.
I noted that the involvement of community leaders and healthcare workers was key to addressing healthcare local needs - from planning to delivery of care. This enhanced trust and continuity of care. Collaborations with local healthcare providers facilitated data collection and facilitated referrals, adherence, follow-ups and improved sustainability [9]. “Telemedicine” can help bridge gaps for clinicians in hospitals to follow-up patient treatment and care in rural settings [10]. Can we learn from this …?
I learned how valuable that I – a trainee doctor - could broaden my practice experience by participating in outreach work – locally or abroad. A “universal history-taking translation toolkit” could be created for different languages and cultures.
I appreciated how important Sustainability is. If patients exhaust their courses of medicines with no reliable local supply or structured follow-up, problems such as antibiotic resistance and anti-malarial resistance can arise – as in Vietnam following the American war. Solutions to prevent this must be established to prevent global health threats emerging [11-14]
I reflected upon the importance of my experiences in preparing us for the increasing numbers of refugees in Europe, such experiences can benefit all trainees. First-hand exposure to such health inequities sensitised me to appreciate the nature of inequalities.
Conclusion and Recommendations
Drawing upon my own and volunteer team’s reflections, I feel this could be an important opportunity for all trainees – to go beyond our normal comfort zones and experience healthcare provision in deprived rural areas. Such outreach programmes offer trainees valuable, if humbling, insights beyond the comforts of UK practice.
The transition from western hospitals to remote impoverished communities made me aware of a whole new world of healthcare needs and provision. I realised my own limitations – in that sense it was both a humbling and an awakening experience. It widened my view of challenges, the complexity of establishing patient rapport, clinical reasoning and barriers to communication. Upon critical reflection, these serve as a foundation to developing my own skills and being more prepared to contribute to understanding and improving how the other half lives.
References
- Sarim MR (2021). Pakistani youth uses e-health to change rural lives. United Nations Conference on Trade and Development. UNCTAD. Available in online.
- Burki SJ, Ziring L. (2025). Encyclopaedia Britannica. (2025). Pakistan: The desert areas. Encyclopaedia Britannica, Inc. Available in online.
- Paterson EH. (1978). The Kwun Tong community health project. Trop Doct. 8: 85-9.
- Anderson JL. (2022). Demystifying research for medical & healthcare students: an essential guide. Wiley Blackwell.
- National Institute for Health and Care Excellence. (2019). Traffic light system for identifying risk of serious illness in under 5s. NICE. Available in online.
- Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, et al. (2008). Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 371: 243-60.
- Persaud N, Bedard M, Boozary AS, Glazier RH, Gomes T, et al. (2020). Effect on treatment adherence of distributing essential medicines at no charge: the CLEAN Meds randomized clinical trial. JAMA Intern Med. 180: 27-34.
- Devassy SM, Scaria L, Babu S, Rajeev SP, Lijo KJ, et al. (2025). Community-level mental health screening and referral using tasksharing with student volunteers in Kerala, India: a scalable model for low and middle income countries. BMC Psychiatry. 25: 352.
Nandu KT. (2022). Human resource management in health: an analysis of community medical camp as short-term medical intervention to deal with shortage of health workers in rural India. Authorea Preprints. Available in online.- World Health Organization Regional Office for Europe. (2024). WHO develops guidance to improve telemedicine services. WHO Regional Office for Europe. Available in online.
- Lonsdale J. (1968). The Tanzanian experiment. Afr Aff. 67: 330-44.
- World Health Organization. (2024). Compendium of innovative health technologies for low-resource settings. WHO. Available in online.
- Doe J, Smith A. (2022). Reciprocal learning in global health partnerships: a framework for bidirectional exchange. BMJ Glob Health. 7: e008000.
- Riis JA. (1890). How the other half lives: studies among the tenements of New York. Charles Scribner’s Sons. Available in online.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.