Holohemispheric Subdural Hematoma: Infantile Acute Subdural Hematoma Localized in the Dural Border Cell Layer
by Nobuhiko Aoki*
Department of Neurosurgery, Tokyo Metropolitan Tama Medical Center, Bethlehem Garden Hospital, 2-8-29 Musashidai, Fuchu, Tokyo 183-8524, Japan
*Corresponding author: Nobuhiko Aoki, Department of Neurosurgery, Tokyo Metropolitan Tama Medical Center, Bethlehem Garden Hospital, 2-8-29 Musashidai, Fuchu, Tokyo 183-8524, Japan
Received Date: 28 August 2024
Accepted Date: 02 September 2024
Published Date: 04 September 2024
Citation: Aoki N (2024) Holohemispheric Subdural Hematoma: Infantile Acute Subdural Hematoma Localized in the Dural Border Cell Layer. Ann Case Report. 9: 1959. https://doi.org/10.29011/2574-7754.101959
Abstract
Background: Acute subdural hematoma (ASDH) in an infant without external signs of head trauma is sometimes thought to be symptomatic of shaken baby syndrome (SBS) or abusive head trauma (AHT) in the United States or of infantile acute subdural hematoma (IASDH) due to minor head trauma in Japan. The present case report aimed to demonstrate that IASDH can occur spontaneously if the dural border cell layer is disrupted in an infant with cranio-cerebral disproportion (CCD).
Case description: A 3-month-old, female patient developed vomiting while being fed with her mother’s breast milk. On the next morning, she vomited again and during the night of the same day suddenly began crying after displaying generalized convulsions. The patient was taken to an emergency room, where head computed tomography found an ASDH on the right side. An ophthalmological examination revealed right-sided retinal hemorrhages. Magnetic resonance imaging on hospital day 2 revealed a thin, film-like, high-intensity ASDH surrounding the entire, cerebral convexity on the right side. In addition, benign enlargement of the subarachnoid space (BESS) and sylvian fissure (LSF) was noted. On hospital day 2, the vomiting and seizures subsided, and the remainder of her clinical course was uneventful.
Conclusion: The present case is invaluable because it demonstrates that IASDH can occur in the absence of an external impact to the head. The diagnostic criteria for SBS/AHT, particularly in terms of their application to very young infants, need to be reviewed, considering that the presence of CCD, including BESS and LSF, may cause IASDH even without trauma. Particularly relevant here is the thin, film-like, holohemispheric appearance on neuroimaging studies characterizing IASDH localized in the disrupted Dural border cell layer. The present study proposes the term, holohemispheric subdual hematoma, to describe this phenomenon.
Keywords: Infantile acute subdural hematoma; shaken baby syndrome; abusive head trauma; benign enlargement of the subarachnoid space; large sylvian fissure; dural border cell layer; holohemispheric subdural hematoma
Introduction
In the English-speaking world, a subdural hematoma (SDH) in infants is normally considered symptomatic of an injury, such as that resulting from shaken baby syndrome (SBS) or abusive head trauma (AHT). However, SDH can occur in a number of circumstances involving mild head trauma without any evidence of a mechanical impact [1].
Infantile acute subdural hematoma (IASDH) was defined in 1984 as apparently being caused by minor head trauma without loss of consciousness or any association with a primary brain injury [2]. The present case is a valuable illustration of the fact that IASDH can occur if the dural border cell layer is disrupted even in the absence of an external impact to the head. The present study is the first to report the novel, neuroimaging findings of this hitherto undocumented condition, which has been termed holohemispheric subdural hematoma.
Case Presentation
The patient was a female infant who was born after an uncomplicated delivery. Her medical history was unremarkable. At the age of 3 months, while she was being breast-fed by her mother, she experienced an episode of vomiting. On the morning of the following day, she vomited again and was brought to a nearby pediatric clinic, where a medication for vomiting was prescribed. During the night of the same day, however, she suddenly began crying. While holding the patient in her arms, the mother noticed clonic seizures in the right arm followed by generalized convulsions. The patient had no history of head trauma, and the episode was recorded on video.
The patient was taken to the emergency room of a nearby hospital, where head computed tomography (CT) revealed a prominent, acute subdural hematoma (SDH) in the parasagittal region and a thin, film-like SDH inside the inner table of the skull (Figure 1).
The infant was admitted for further observation and underwent magnetic resonance imaging (MRI) on hospital day 2, which visualized the thin, film-like, high-intensity SDH surrounding the entire cerebral convexity on the right side. In addition, benign enlargement of the subarachnoid space (BESS) and sylvian fissure (LSF) was noted (Figure 2). No mass effect or cerebral parenchymal abnormalities were observed. An ophthalmological examination revealed a right-sided, retinal hemorrhage (Figure 3). Although no neurological abnormality or external signs of trauma were noted, the infant was admitted for observation and treated with anticonvulsant medication. On hospital day 2, the vomiting and irritability subsided, and her subsequent clinical course was uneventful. At the age of 2 years, tests confirmed that she had achieved the normal, developmental milestones.
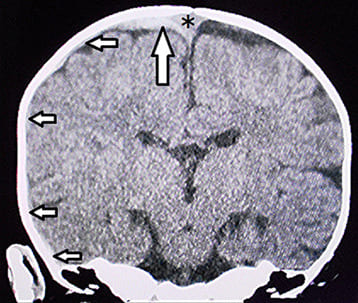
Figure 1: Coronal view on computed tomography on presentation. A prominent acute subdural hematoma can be seen in the parasagittal region of the right side (large arrow). Thin, film-like subdural hematomas can be seen within the inner table of the skull (small arrows). The asterisk indicates the superior sagittal sinus.
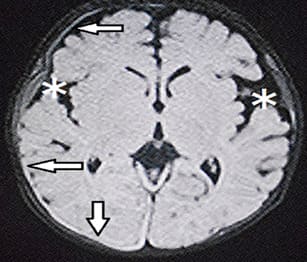
Figure 2: Magnetic resonance imaging on the day after admission. Left: Fluid-attenuated inversion recovery (axial image) showing the subdural hematoma (SDH) with a thin, film-like appearance on the right side (arrows) surrounding the entire cerebral hemisphere (i.e, the holohemispheric SDH). Note the bilaterally enlarged sylvian fissure (asterisks).
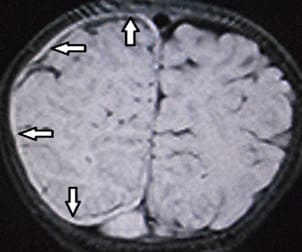
Center: T1-weighted coronal image showing the subdural hematoma (SDH) with a thin, film-like appearance on the right side (arrows) surrounding the entire cerebral hemisphere (i.e, the holohemispheric SDH)
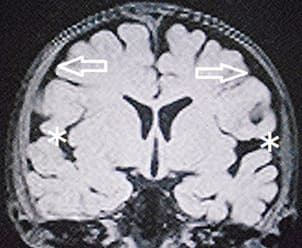
Right: T1-weighted coronal image showing benign enlargement of the subarachnoid space (arrows) and sylvian fissure (asterisks)

Figure 3: Fundoscopic examination showing retinal hemorrhages on the right side. Note that most of the hemorrhages follow the pattern of the blood vessels. (No hemorrhage was observed on the left side.)
Discussion
The infant in the present case experienced rapid, neurological recovery following episodes of vomiting and seizure. Her favourable clinical course indicated mild IASDH [2-4]. Furthermore, the BESS and LSF seen on CT and MRI indicated intracranial, structural vulnerabilities predisposing the patient to IASDH development [4-6]. Based on the bio physiological characteristics of infants, IASDH was originally defined in 1984 as acute, infantile subdural hematoma apparently caused by minor head trauma without loss of consciousness or any association with a primary brain injury [2]. Cases of IASDH have been reported in Japan since the 1960’s [7]. However, because most of these cases were published in Japanese-language journals and accusations that the diagnosis was an attempt to conceal child abuse were frequently raised, the concept of IASDH has not been widely accepted in the English-speaking world [8]. Nonetheless, recent Japanese reports have demonstrated that patients with IASDH can be distinguished from those with SBS/AHT through multidisciplinary assessment, including an evaluation by child abuse pediatricians and pediatric neurosurgeons [3,4,9-12].
Furthermore, the absence of a primary brain injury in IASDH indicates a fundamental difference from SBS/AHT. The findings of nation-wide, multicentre, retrospective studies in Japan (2022) are particularly valuable in that they provide reliable corroboration of this finding [9,13,14].
Although anatomically there is no preformed space, a distinct, soft-tissue layer at the dura-arachnoid interface, termed dural border cell layer (DBCL) by Nabeshima et al., has been proved to be present [15]. The DBCL is composed of a loosely adherent conglomeration of cells having enlarged extracellular spaces and no extracellular collagen. A SDH in this environment results from the disruption this dural border cell layer by the collection of blood. Furthermore, in the superficial compartment of the DBCL, there is a well-developed dural venous plexus, which fills the venous sinuses. Because the DBCL is easily disrupted, a hemorrhage originating in the inner dural plexus may be chiefly responsible for the non-traumatic symptoms of this condition.
In the present patient, the parasagittal venous plexus, which communicates with the superior sagittal sinus, was the likely source of the bleeding, as suggested by the conspicuous hemorrhages seen on CT [1]. The parasagittal hemorrhage continued peripherally in a tapering fashion, forming the characteristic, thin, film-like hematoma surrounding the entire hemisphere (i.e, the holohemispheric subdural hematoma) on the right side (Figure 2). This hemorrhagic lesion may directly affect the DBDL due to the latter is fragility. Thus, the age-specific vascularity of the dura together with intracranial, structural vulnerabilities secondary to CCD, including the BESS and LSF, are considered to be the etiological factors in the spontaneous development of IASDH.
Finally, a fundoscopic examination in the present case found right-sided retinal hemorrhages (RH), most of which occurred along the blood vessels. The pattern of the RH in this patient suggested that a vessel-related mechanism, such as intracranial hypertension and/or venous congestion, may have been involved rather than an eye injury caused by a direct, traumatic impact to the head or face (Figure 3).
Conclusion
The present case is invaluable because it demonstrates that IASDH can occur in the absence of an external impact to the head. The diagnostic criteria for SBS/AHT, particularly in terms of their application to very young infants, need to be reviewed, considering that the presence of CCD, including BESS and LSF, may cause IASDH even without trauma. Particularly relevant here is the thin, film-like, holohemispheric appearance on neuroimaging studies characterizing IASDH localized in the disrupted dural border cell layer. The present study proposes the term, holohemispheric subdual hematoma, to describe this phenomenon.
Author’s contribution: Nobuhiko Aoki (corresponding author with no co-authors) conceived the study and conducted a search of the literature.
Availability of data and materials: This article does not include any data or material that can be provided.
Declarations, ethics approval, and consent to participate: This study was approved by the ethics committee of Bethlehem Garden Hospital and Tokyo Metropolitan Tama Medical Center. No funding was obtained for this study. The parents/legal guardians provided consent to publish the details of the case described in this report.
Consent to publish: The author consents to the publication of identifiable details, which can include photographs, case history, and other details.
Conflicts of interest: None
References
- Mack J, Squier W, Eastman JT (2009) Anatomy and development of the meninges: implications for subdural collections and CSF circulation. Pediatr Radiol 391:200-210.
- Aoki N, Masuzawa H (1984) Infantile acute subdural hematoma. Clinical analysis of 26 cases. J Neurosurg 61: 273-280.
- Aoki N (2023): Clinical and neuroimaging characteristics in mild-type infantile acute subdural hematoma. Report of four cases. Childs Nerv Syst 40:189-195.
- Aoki N (2024) Infantile acute subdural hematoma. Clinical and neuroimaging analysis of 15 cases focusing on intracranial structural vulnerabilities. Journal of Surgery.
- Aoki N (2024) Infantile acute subdural hematohygroma: A clinical and neuroimaging analysis of 18 casesAmerican Journal of Pediatrics. 10:26-33.
- Aoki N (2024). Asymptomatic infantile acute subdural hematoma with benign enlargement of the subarachnoid space and large sylvian fissure. Mega J Case Rep. 7:2001-2006.
- Aoki N (2011) Infantile acute subdural hematoma: Caused by abuse or mild head trauma? Nervous System in Children 36:326-330.
- Rekate HL (1985) Subdural hematomas in infants. (Letter) J Neurosurg 61: 316-317.
- Akutsu N, Nonaka M, Narisawa A, Kato M, Harada A, et al (2022) Infantile subdural hematoma in Japan: a multicenter, retrospective study by the J-HITs (Japanese head injury of infants and toddlers study) group. PLoS ONE. 25: e0264396.
- Aoki N (2020) Infantile acute subdural hematoma with retinal hemorrhage caused by minor occipital impact witnessed by an ICU nurse: a case report. Pediatr Neurol Neurosci. 4: 47-50.
- Shimoji K, Suehiro E, Matsuno A, Araki T (2022) Abusive head trauma in Japan. Childs Nerv Syst 38:2387-2393.
- Aoki N (2020) "Infantile" acute subdural hematoma: a clinical entity different from abusive head trauma. J Pediatr Neurol Neurosci. 4:151-53.
- Narisawa A, Nonaka M, Akutsu N, Kato M, Harada A, et al (2022) Unexplained mechanism of subdural hematoma with convulsion suggests nonaccidental head trauma: a multicenter, retrospective study by the Japanese Head injury of Infants and Toddlersstudy (J-HITs) group.PLoS ONE. 17:e0277103.
- Kato M, Nonaka M, Narisawa A, Harada A, Park YS (2023) Correlations of intracranial pathology and cause of head injury with retinal hemorrhage in infants and toddlers: A multicenter, retrospective study by the J-HITs (Japanese Head injury of Infants and Toddlers study) group PLoS One. 18:e0283297.
- Nabeshima S, Reese TS, Landis DM, Brightman MW (1975) Junctions in the meninges and marginal glia. J Comp Neurol 164:127-169.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.