Hidden Risks in Liposuction: The Role of Abdominal Wall Ultrasound in Preventing Visceral Perforation
by Jesua Emmanuel Avilez1,2*, Cesar Edwinn Martínez3, Daniel Rodolfo Noriega1, Jonathan Mauricio Quisilema1, Ruben Reyes2, Pamela Irais Pineda1
1Plastic Surgery Service, University Hospital Miguel Enriquez, Havana, Cuba
2NipTuck Clinic, Mexico City, Mexico
3Plastic Surgery Medical Unit, Ibagué, Colombia
*Corresponding author: Jesua Emmanuel Avilez, NipTuck Clinic, Mexico City, Mexico
Received Date: 09 September 2025
Accepted Date: 15 September 2025
Published Date: 17 September 2025
Citation: Avilez JE, Martínez CE, Noriega DR, Quisilema JM, Reyes R, et al. (2025) Hidden Risks in Liposuction: the Role of Abdominal Wall Ultrasound in Preventing Visceral Perforation J Surg 10: 11443 https://doi.org/10.29011/2575-9760.011443
Abstract
Background: Liposuction is a widely performed aesthetic procedure. While generally safe, visceral perforation remains a rare but life-threatening complication, often caused by undiagnosed abdominal wall defects missed in standard preoperative evaluations.
Objective: This study evaluates the effectiveness of preoperative abdominal wall ultrasound as a screening tool for detecting hidden defects in liposuction candidates, aiming to reduce the risk of visceral perforation.
Methods: A retrospective observational study was conducted on 189 patients who underwent body contouring surgery between July 2021 and January 2025 at a single institution. All underwent preoperative ultrasound to detect umbilical hernias, diastasis recti, and inguinal hernias. Risk factors such as smoking, previous pregnancies, and prior liposuction were analyzed.
Results: 18 patients (9.5%) had abdominal wall defects, with umbilical hernia (55.5%) being the most frequent, followed by diastasis recti (16.7%) and inguinal hernias (11.1%). Smoking (61.1%), previous pregnancies (38.9%), and prior liposuction (44.4%) were significant risk factors. Preoperative ultrasound identified 88.9% of defects, allowing surgical modifications and reducing potential complications.
Conclusion: Preoperative ultrasound is a valuable tool for liposuction candidates, especially those with risk factors such as prior surgery or pregnancies. Systematic ultrasound screening enhances patient safety by detecting undiagnosed defects that could lead to severe intraoperative complications. Incorporating ultrasound into standard preoperative protocols is recommended to improve surgical outcomes.
Keywords: Abdominal Wall Defects; Body Contouring; Liposuction; Preoperative Ultrasound; Surgical Safety; Visceral Perforation
Introduction
Background and Justification
Liposuction is one of the most commonly performed aesthetic surgery procedures worldwide due to its effectiveness in body contouring. However, despite its relatively high safety profile, it remains a procedure with associated risks, among which visceral perforation is one of the most severe and potentially fatal complications. This injury, which can occur in hollow organs such as the small intestine or colon, or solid viscera like the liver and spleen, often goes unnoticed during the procedure and manifests later as peritonitis, sepsis, and multiple organ failure [1]. One of the main contributing factors to this complication is the presence of hidden defects in the abdominal wall, which may not be detected in standard preoperative clinical evaluation. These defects include undiagnosed abdominal hernias, areas of fascial weakness, and diastasis recti-conditions that do not cause obvious symptoms and can therefore be overlooked even by experienced surgeons [2]. Patients with risk factors such as previous pregnancies, smoking, or a history of abdominal surgery are particularly susceptible to these abdominal wall defects, increasing the risk of visceral perforation during liposuction [3]. Despite these risks, preoperative evaluation in most cases relies exclusively on physical examination and medical history-tools that may be insufficient to identify structural defects when no clinical manifestations are present [4].
Abdominal Wall Ultrasound as a Preventive Method
Abdominal wall ultrasound has become a key tool in the preoperative evaluation of liposuction candidates, allowing for the detection of abdominal wall defects that are not evident in traditional clinical examinations [5]. Its ability to visualize incipient hernias, areas of fascial thinning, and zones of muscular fragility represents a significant advancement in preventing surgical complications. Previous studies have shown that liposuction can exacerbate preexisting abdominal wall defects or lead to unintended injuries in patients with a history of abdominal surgery [6]. In these cases, preoperative ultrasound not only helps identify high-risk patients but also allows for adjustments in surgical planning, either by modifying the liposuction technique or contraindicating it in highrisk cases [7]. Additionally, evidence suggests that the systematic use of ultrasound in preoperative evaluation could significantly reduce the risk of visceral perforation, particularly in patients with a history of prior abdominal surgery, multiple pregnancies, or smoking [7].
Objective of the Study
The objective of this study is to evaluate the effectiveness of abdominal wall ultrasound as a preoperative screening method in liposuction patients to prevent visceral perforations. Clinical characteristics, the reason for consultation versus the actual surgery performed, and the presence of abdominal wall defects detected by ultrasound will be analyzed. Additionally, the correlation with predisposing factors such as previous pregnancies, smoking, and prior abdominal surgeries will be examined. Furthermore, the relationship between the presence of abdominal wall defects and the risk of visceral perforation in patients who have previously undergone liposuction will be assessed.
Methods
Study Design
This is a retrospective observational study, analyzing patients who underwent body contouring plastic surgery, primarily liposuction, between July 2021 and January 2025 in a single institution. The presence of abdominal wall defects was assessed using preoperative ultrasound, and its correlation with predisposing factors and the risk of visceral perforation was evaluated.
Study Population
A total of 189 patients who requested liposuction or body contouring procedures were included, regardless of their postevaluation diagnosis. All patients underwent a preoperative evaluation protocol, which included abdominal wall ultrasound. Among these, 18 patients (9.5%) were diagnosed with abdominal wall defects, with umbilical hernia being the most frequent finding, followed by diastasis recti and inguinal hernias.
Inclusion and Exclusion Criteria
Inclusion Criteria
- Patients requesting body contouring surgery (liposuction, abdominoplasty, mini-abdominoplasty, etc.).
- Patients who underwent preoperative abdominal wall ultrasound evaluation.
Exclusion Criteria
- Patients with BMI >30.
- Patients over 50 years old or under 18 years old.
Preoperative Ultrasound Evaluation
A Chison ECHO-2 ultrasound machine with a 10 MHz linear transducer was used. The parameters for detecting abdominal wall defects included:
- Diastasis recti: A rectus muscle separation of greater than 2.5 cm.
- Umbilical hernia: Detectable defects of any size identified via ultrasound.
- Inguinal hernias: Identified regardless of whether they were direct or indirect, and irrespective of defect size.
The evaluation protocol consisted of four key anatomical points
- from the xiphoid process to the umbilicus for diastasis recti detection and epigastric hernia.
- to identify umbilical defects.
- (semilunar line) to assess lateral hernias (Spiegel hernias).
- to detect inguinal hernias.
Findings were documented with ultrasound images and stored in each patient’s clinical record.
Data Analysis
The data analysis aimed to determine
- The proportion of patients with abdominal wall defects within the total sample.
- The relationship between preoperative ultrasound detection and the prevention of severe intraoperative complications, including visceral perforation.
- The correlation between a history of prior liposuction and abdominal wall defects.
- The impact of ultrasound findings on surgical decisionmaking, assessing false negatives in hernia detection.
False negatives were identified in two patients, necessitating three consecutive evaluations due to discrepancies between clinical examination and initial ultrasound findings. In both cases, the presence of a defect was later confirmed by a radiologist. This emphasizes that ultrasound is operator-dependent, highlighting the need for a standardized preoperative protocol for body contouring surgery.
Results
Study Population Overview
The demographic and clinical characteristics of patients diagnosed with abdominal wall defects, including age, BMI, and relevant clinical history.
Characteristics of Patients with Abdominal Wall Defects:
- Total patients analyzed: 189
- Patients with abdominal wall defects: 18 (9.5%)
- Average age: 36.5 years
- Average BMI: 26.14
- Patients with a history of smoking: 61.1%
- Patients with previous pregnancy: 38.9%
- Patients with previous liposuction: 44.4%
• Age range: 25 - 50 years
Abdominal Wall Defects Detected
The distribution of abdominal wall defects is shown in (Figure 1), where umbilical hernia was the most frequent finding (55.5%), followed by diastasis recti and inguinal hernias.
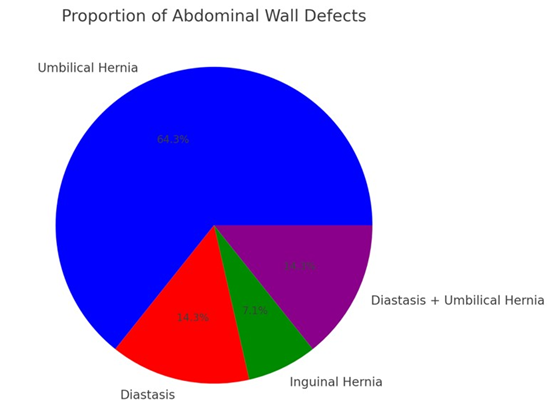
Figure 1: Proportion of Abdominal Wall Defects
- Umbilical hernia: 10 cases (55.5%)
- Diastasis recti: 3 cases (16.7%)
- Inguinal hernia: 2 cases (11.1%)
- Diastasis + umbilical hernia: 3 cases (16.7%)
Risk Factors Associated with Abdominal Wall Defects
The relationship between abdominal wall defects and risk factors is illustrated in (Figure 2), showing that smoking was the most common factor among patients with defects (61.1%).
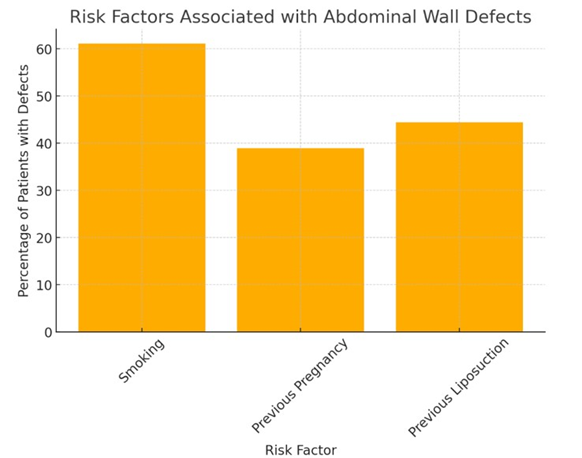
Figure 2: Risk Factors Associated with Abdominal Wall Defects.
Additionally, (Table 1) compares the frequency of defects in patients with and without previous liposuction, demonstrating a higher prevalence of umbilical hernia and diastasis recti in patients with a history of liposuction.
Abdominal Wall Defect | Patients with Previous Liposuction | Patients without Previous Liposuction |
Umbilical Hernia | 4 | 9 |
Diastasis Recti | 3 | 2 |
Inguinal Hernia | 1 | 1 |
Diastasis + Umbilical Hernia | 1 | 2 |
Table 1: Relationship Between Previous Liposuction and Abdominal Wall Defects.
Impact of Ultrasound in the Prevention of Complications
Preoperative ultrasound successfully detected abdominal wall defects in 18 out of 189 patients, allowing for their correction before surgery. However, two false negatives were identified, highlighting the importance of operator experience and the need for repeat evaluations in suspected cases.Without the use of ultrasound, these defects could have gone unnoticed, increasing the risk of visceral perforation during liposuction.
Discussion
Interpretation of Results
Preoperative ultrasound allowed for the identification of abdominal wall defects in 9.5% of the evaluated patients, effectively preventing potential intraoperative complications. The most frequent defect observed was umbilical hernia (55.5%), followed by diastasis recti and inguinal hernias. These findings align with previous studies suggesting that undiagnosed abdominal wall defects may contribute to increased surgical risks [2]. A significant correlation was observed between risk factors and the presence of abdominal wall defects, with smoking (61.1%) being the most prevalent, followed by previous pregnancies (38.9%) and a history of prior liposuction (44.4%). These findings suggest that tobacco use and previous surgical interventions may weaken the integrity of the abdominal wall, increasing the likelihood of developing defects that could compromise surgical safety. Notably, 44.4% of patients with defects had undergone previous liposuction, reinforcing the hypothesis that preexisting abdominal wall defects may go undiagnosed and could be exacerbated by prior surgical procedures. This highlights the importance of incorporating preoperative ultrasound as a routine screening tool, particularly for patients with prior liposuction or a history of abdominal surgeries.
Comparison with the Literature
Previous studies have documented visceral perforation as one of the most severe complications of liposuction, with fatal outcomes in some cases [1]. Traditional preoperative assessments-based solely on clinical history and physical examination-have been shown to be insufficient in detecting hidden abdominal wall defects [4]. Our study aligns with these findings, reinforcing the role of ultrasound as a complementary diagnostic tool to enhance patient safety [5]. Emphasized the increasing role of diagnostic ultrasound in aesthetic surgery, particularly in detecting subtle anatomical variations that may impact surgical planning. Our findings further support this approach, demonstrating that systematic ultrasound screening can prevent complications by identifying high-risk patients preoperatively [8].
Study Limitations
While the results provide valuable insights, certain limitations must be acknowledged:
- Operator dependence: Ultrasound is an operator-dependent imaging modality, and variability in skill levels may affect diagnostic accuracy. In two cases, false negatives were identified, requiring further evaluation by a radiologist.
- Single-center study: The study was conducted at a single institution, which may limit the generalizability of the findings to other patient populations.
- Lack of a control group: A comparison group of patients who did not undergo ultrasound screening could have strengthened the analysis of its impact on reducing complications. Clinical Relevance and Recommendations
Given the findings of this study, we recommend
- Systematic integration of preoperative abdominal wall ultrasound into the standard assessment protocol for body contouring surgery.
- Targeted screening for high-risk patients, particularly those with a history of prior liposuction, pregnancy, or smoking.
- Specialized training for plastic surgeons in the use and interpretation of ultrasound imaging to improve diagnostic accuracy.
- Further multicenter studies to confirm the efficacy of ultrasound screening in preventing surgical complications.
By adopting these recommendations, the safety of liposuction and other body contouring procedures can be significantly enhanced, reducing the likelihood of severe intraoperative and postoperative complications.
References
- Barros LFL, Teixeira VF, Reis JAP, Ferraz RA, Araújo DC, et al. (2014) Complications in liposuction: Systematic review. brazilian Journal of Plastic Surgery 38.
- Stevens WG, Spring MA, Stoker DA (2010) Liposuction complications: Systematic review of case studies. Aesthetic Surgery Journal 2010.
- Reish RG, Seify H (2015) Perforation of viscera, a dramatic complication of liposuction: Review of literature. Plastic and Reconstructive Surgery 135: 743-750.
- González-García A, Ríos-Luna A (2018) Perforación intestinal tras liposucción: Revisión de casos. Cirugía Española 2018.
- Swanson E (2018) The expanding role of diagnostic ultrasound in plastic surgery. PRS Global Open 2018.
- Talmor M, Hoffman LA, Lieberman M (1997) Intestinal perforation after suction lipoplasty: a case report and review of the literature. Annals of Plastic Surgery 38: 169-172.
- Sozer SO, Agullo FJ, Palladino H (2000) Intestinal perforation after suction lipoplasty: A rare but potentially lethal complication. Annals of Plastic Surgery.
- Thieme M (2020) Ultrasound evaluation of abdominal wall defects in aesthetic surgery patients. Journal of Aesthetic Surgery 2020.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.