Gunshot Injuries Resulting in Arthroplasty: A Literature Review and Case Report Resulting in a Megaprosthesis
by Jonghoo Sung1*, Margarita-Chrissi Litinas1, Jakub Jagiello2, Justin Alexander2, Tom Tolley3, Peter Smitham1,2
1Adelaide Medical School, University of Adelaide, 136 North Terrace, Adelaide SA 5000, Adelaide, Australia
2Department of Orthopaedics and Trauma, Royal Adelaide Hospital, Port Rd, Adelaide SA 5000, Adelaide, Australia
3Ballistic Headquarters, 12 Moorcroft Court, Burnside SA 5066, Australia
*Corresponding author: Jonghoo Sung, Adelaide Medical School, North Terrace, Adelaide 5000, Australia
Received Date: 16 June 2024
Accepted Date: 21 June 2024
Published Date: 24 June 2024
Citation: Sung J, Litinas M, Jagiello J, Alexander J, Tolley T, et al (2024) Gunshot Injuries Resulting in Arthroplasty: A Literature Review and Case Report Resulting in a Megaprosthetsis. Ann Case Report. 9: 1855. https://doi.org/10.29011/2574-7754.101855
Abstract
Background: Gunshot injuries (GSIs) are high-energy traumas that result in extensive damage to soft tissues and bones. There exists limited evidence and consensus regarding the optimal duration for maintaining antibiotic spacers before the insertion of definitive arthroplasty. We present a case of severe GSI treated with staged megaprosthesis insertion and conducted a systematic review to determine the timing of arthroplasty in these complex cases.
Methods: Our systematic review targeted English-language papers published after1980, focusing on arthroplasty-treated intraarticular gunshot injuries in patients aged 18 and above from Database searches including PubMed, Medline, Embase, CINAHL, and Scopus. Criteria included staged or single arthroplasty with documented follow-up. A ballistics expert provided additional experimental details regarding the exact distance, gun and shot used.
Results: Systematic search identified 15 relevant articles with 35 cases reported resulting in arthroplasty following a gunshot injury. Thirty cases reported timing of surgery. The median time to definitive arthroplasty was 7 months, (mean 13.8 months, range 12 days to 64 months). Ten cases involved gunshot injuries to the shoulder. In our case, deformation of the pellets implied the shot was lead and spray pattern allowed the distance to be calculated.
Conclusion: In conclusion, our systematic review highlights the limited evidence and lack of consensus regarding the optimal timing of arthroplasty for complex, intraarticular GSIs. We found a median time to definitive arthroplasty of 7 months, indicating a wide variation in practice. Our presented case of a shoulder injury underscores the importance of interdisciplinary collaboration and detailed forensic analysis in understanding the mechanism of injury.
Keywords: Gunshot injury; Megaprosthesis; Total shoulder replacement; Trauma; Orthopaedic Surgery.
Introduction
Gunshot injuries (GSIs) are a rarity in Australia, with an incidence rate of 1.8 per 100,000 reported in recent literature [1]. The high kinetic energy of bullets and explosive gun particles may result in significant haemorrhage, lead intoxication, organ damage, and death [2,3]. GSIs of the extremities have significant orthopaedic implications due to soft tissue and neurovascular damage, open comminuted fracture, and posttraumatic arthritis [4]. While open reduction and internal fixation (ORIF) and intramedullary (IM) nails have shown efficacy in the management of GSIs [1], there exist cases where these treatment modalities prove impractical due to the complexity of the injury and involvement of the joint. Herein, we present the case of an 81-year-old male who suffered a complex GSI to the proximal humerus, accompanied by multiple retained bullet shrapnel fragments. The extent of soft tissue injury, compromised bone stock, and the inherent risk of infection rendered ORIF and IM nails unsuitable options. Consequently, the patient underwent a series of debridement followed by the insertion of an antibiotic-coated humeral nail, complemented by antibioticinfused cement, ultimately culminating in a reverse proximal humerus replacement. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). This study was approved by Human Research Ethics Committee of Central Adelaide Local Health Network (Reference Number: 18407). Written and verbal consent was obtained from the patient.
Case Description
An 81-year-old Caucasian male with a medical history significant for atrial fibrillation, ischemic heart disease, cerebrovascular disease, and Type 2 Diabetes Mellitus was transported to the Royal Adelaide Hospital Emergency Department (ED) following closerange gunshot injury to his right shoulder and thigh. On arrival, he presented with hypotension and tachycardia, necessitating the activation of a Level 1 Trauma call and initiation of a massive transfusion protocol.
Orthopaedic and vascular surgeons conducted an initial assessment of the patient, which revealed a large entry wound in the right shoulder without any discernible exit wound. A further entry wound was observed on the proximal anterior thigh, and a larger exit wound was identified on the posterolateral aspect. Physical examination indicated compromised axillary nerve function, affecting both motor and sensory functions. However, the remaining neurovascular status of the affected upper and lower limbs remained intact.
Plain film radiographs (Figures 1a and 1b) and computed tomography (CT) scans revealed a heavily comminuted fracture of the proximal humerus, resulting in the loss of articular integrity and the presence of multiple retained bullet fragments. Additionally, there was a minimally displaced, comminuted fracture of the acromion, with an intact glenoid process. No osseous injuries were identified in the lower limb. The patient received broadspectrum antibiotics (intravenous cefazolin and metronidazole). Subsequently, he was taken to the operating room for thorough cleaning, debridement of devitalized muscle and soft tissue, and intraoperative exploration. Intraoperatively, it was observed that there was very minimal remaining deltoid, teres major, and pectoralis major muscle tissue, with complete disruption of all rotator cuff muscles. Furthermore, a significant loss of tissue at the quadrangular space was evident, and no identifiable axillary nerve could be located. The wound was contaminated with clothing material, wad and loose easily accessible pellets were removed.
After achieving physiological stability, a temporary humeral spacer was fashioned using a humeral nail coated with PALACOS® cement and inserted into the distal diaphysis. Subsequently, the initial spacer was replaced with a new one infused with vancomycin cement, featuring a 36mm humeral head created from an acetabular liner (Figure 2). Although shoulder mobility with a broad-arm sling was permitted, it remained limited due to persistent pain. At the four-month mark, the patient began experiencing pain and irritation anteriorly in the right shoulder. A nerve conduction study (NCS) confirmed the absence of axillary and suprascapular nerve function. Radiographs revealed anteroinferior dislocation of the spacer, prompting the need for surgical intervention. Surgical options were discussed with the patient, leading to the insertion of a megaprosthesis with a Stanmore Dailey-Walker Constrained Reverse prosthesis using a deltopectoral approach seven months after the initial injury (Figure 3a and 3b). Although the use of a Constant Thickness Anatomic head was contemplated, it was not implemented due to the risk of head subluxation, which could pressurise the anterior skin and increase the risk of wound breakdown. Additionally, a potential radial nerve to axillary nerve transfer was considered and discussed with Plastic and Reconstruction Surgeons. However, it was ultimately not pursued due to the high risk of graft failure, given the distal avulsion of the deltoid muscle with no strong attachment, even if attached to the prosthesis as a sleeve. The surgical outcome was deemed successful, and shoulder rehabilitation commenced on the second post-operative day. At the nine-month follow-up, the patient exhibited satisfactory wound healing and demonstrated active mobility, with measurements of 20° abduction and 50° flexion. Radiographs revealed a well-positioned implant, with evidence of bony ingrowth (Figure 4a and 4b). Notably, the patient reported no pain and expressed overall satisfaction with the functional outcome.
Gunshot injury analysis
In order to ascertain specific details regarding the firearms and ammunition involved, as well as the distance of the shot, the expertise of a ballistics specialist (TT) was enlisted. Examination of the images in this case suggests that the 12-gauge shotgun ammunition likely belonged to American Size 7, 7½, or 8, as indicated in Table 1. Radiographic analysis of the retained pellets within the body confirms their composition as lead. This determination is substantiated by the irregular morphology of the pellets, characteristic of lead deformation upon impact on human tissues with varying densities. In contrast, materials such as steel or bismuth would not exhibit such deformation under similar impact conditions.
The determination of the ballistic impact distance necessitates approximation due to the unavailability of precise information regarding the specific barrel length and choke employed during the incident. The fixed length of the shotgun barrel plays a pivotal role in dictating the dispersion pattern of pellets upon exiting the muzzle. Shotgun barrels conventionally range from 18 to 34 inches in length. Additionally, the muzzle configuration of the shotgun may incorporate or be equipped with an integrated choking system. The utilisation of an adjustable choke further influences the degree of pellet spread over distance, a parameter contingent upon the user’s intended purpose, as depicted in Figure 5. A controlled test shoot was conducted using a double-barrel side-byside (cylinder choke) 28” shotgun, representing a typical shotgun configuration. Size 7, 7½, and size 8 shot were discharged at paper approximations mimicking the victim’s shoulder at distances of 2m, 5m, 8m, and 10m. The clinical image and radiographs were utilised to best replicate the dimensions of the victim’s shoulder. Size 8 shotgun ammunition emerged as the closest match to the provided images. The 2m trial was excluded due to its minimal deviation, displaying less than a 5cm maximum spread from the intended aim point.
The subsequent three images (Figure 6) depict America size 8 shotgun ammunition fired from distances of 5m, 8m, and 10m towards the target. The 5m impact was deemed too proximal, revealing a 10cm maximum spread that inadequately represented the impact on the shoulder. Radiographic images, however, exhibited an approximate 17cm spread into the victim’s shoulder, acknowledging that the pattern would likely extend beyond the body. The impact range was estimated to be between 8m and 10m, as observed in the test firings. The 8m test illustrated a 15cm maximum spread with size 8 shot, while the 10m shot exhibited an 18cm maximum spread, signifying the most plausible distance from the shooter to the victim.
Methods
Search strategy and selection criteria
A systematic review was conducted in alignment with the PRISMA reporting guideline. The inclusion criteria included papers published in the English language after the year 1980, with patients older than 18 years who had sustained a gunshot injury including single or multiple bullet shrapnels, to any joints that was treated with either a staged or single arthroplasty, with documented follow-up of management and function after the injury. Exclusion criteria included patients with a gunshot treated with open reduction and internal fixation or arthrodesis, or patients that did not have documented management, followup or complication. The intervention was surgical management, specifically arthroplasty. PubMed, Medline, Embase, CINAHL and Scopus databases were searched up until 28 April 2023. There were no other filters or restrictions applied. Search terms included (gun OR shot*) AND (replac* OR total OR arthro* OR recon*). The searches were augmented by screening the bibliographies of included studies, targeted searches of Google Scholar, searches for grey literature, and consultation with experts in the field including orthopaedic surgeons and ballistic experts.
Data extraction
Following the removal of duplicate items, the studies were reviewed for eligibility for inclusion. This was completed using a web-based software program (Covidence). Studies were initially screened by the title and abstracts and then further screened by full text review. Data extraction was performed by two independent investigators (ML and JS). Any discrepancies were discussed and resolved with the senior investigator (PS).
Results
Systematic search identified 15 relevant articles with 35 cases reported. Details of the 35 cases are summarised in Table 2. The average age of the patients was 34.3 years (range 18-70). There were 24 male patients and one female patient. The gender was not specifieid for 10 cases. The injuries exhibited diverse joint involvement, with 15 cases affecting the hips, two affecting the knees, 10 involving the shoulders, and eight affecting the elbows. The affected side varied, with 11 cases on the right, 12 on the left, and 10 cases where the side was not specified. The average time to arthroplasty from gunshot injury was 13.8 months.
Various types of arthroplasty procedures were performed, including
Total Hip Arthroplasty (n=13), Total Knee Arthroplasty (n=2), Hip Hemiarthroplasty (n=2), Reverse Shoulder Arthroplasty (n=1), Anatomic Total Shoulder Arthroplasty (n=1), Resurface Shoulder Hemiarthroplasty (n=1), Global Shoulder Endoprosthesis (n=1), Bi-modular Shoulder Endoprosthesis (n=1), Shoulder Hemiarthroplasty (n=5), Interposition Elbow Arthroplasty with Masquelet Technique (n=1), and Semi-constrained Total Elbow Prosthesis (n=7). The average follow-up duration, excluding cases with unspecified follow-up periods, was 49.6 months. Complications were observed in 10 cases, with two cases exhibiting poor functional outcomes, and four cases lacking specific complication details. Additionally, complications such as septic loosening (n=1), aseptic loosening (n=3), infection leading to the removal of the implant with a late (24-year) attempt at arthrodesis (n=1), and implant removal due to pain and dysfunction with an attempted arthrodesis using a vascularized fibular graft (n=1) were identified.
Four instances of gunshot injuries (two hips, two knees) were managed through staged arthroplasty with a temporary spacer insertion, mirroring our approach. The average time to arthroplasty was 13.8 months, and the average duration of spacer insertion was 5.3 months in these staged cases. Remarkably, these cases exhibited a complication-free course, with an average time to follow up of 31 months.
Discussion
This case report outlines the utilisation of staged proximal humeral replacement as a treatment approach for patients who have sustained a shotgun injury to the proximal humerus, while providing a review of literature on this rare condition. In Australia, gunshot injuries (GSIs) represent an infrequent form of traumatic injury, with an estimated incidence of 1.8 cases per 100,000 individuals [2]. Gunshot injuries represent high-energy traumas that often lead to significant soft tissue and bony injuries, along with the potential for lead toxicity [3], and severe contamination, with an infection rate of up to 15.7% [4-6]. To mitigate the risks of infection and pain while aiming for the optimal restoration of function, it is imperative to engage specialist care.
Bullet wounds should be categorised as contaminated wounds, carrying a significant risk of infection [7]. Contrary to popular belief, bullet fragments are not ‘sterile’ [8] due to the heat generated during firing. In fact, there are documented cases of deliberately contaminated bullets being used in warfare to induce anthrax infections [9]. Bullets can instigate infection through the introduction of foreign materials and by creating a temporary cavity capable of drawing infective particles from either end of the wound track [8], potentially leading to sepsis [10]. Furthermore, shotgun injuries often result in the retention of numerous pellets and wadding, generating high-velocity wounds that escalate the risk of infection [11-13]. Zsoldos and colleagues published a case series featuring four patients who sustained humeral shotgun injuries and underwent hemiarthroplasty of the shoulder, with three cases ultimately developing acute prosthetic joint infections (PJI) [14].
Notably, the average time from gunshot injury to arthroplasty observed in our review was 13.8 months. This temporal delay in intervention, averaging nearly a year, appears to align with a prudent consideration for soft tissue healing. It is conceivable that this interval allows for the resolution of acute inflammatory responses, facilitates adequate wound healing, and mitigates the risk of infection. The intricacies of managing gunshot injuries, particularly in the periarticular regions, necessitate a careful balance between the urgency for surgical intervention and the imperative for optimal tissue healing.
Every possible measure should be taken to mitigate the risk of infection associated with gunshot injuries (GSIs) and to prevent the development of gunshot sepsis. The use of intravenous antibiotics or antibiotic-laden bone cement as prophylaxis against infection following aseptic or primary arthroplasty has been extensively documented in the literature and has demonstrated clinical efficacy [15-17]. In cases where PJI is already established, the staged arthroplasty approach, involving debridement, placement of an antibiotic spacer, and subsequent arthroplasty, is a well-established treatment modality [18-20]. These antibiotic spacers can be left in place for a period ranging from six weeks to several months [20, 21]. This extended duration allows for the achievement of high tissue antibiotic concentrations at the infection site, promotes adequate recovery of the inflamed and congested tissues around the infected joint, and facilitates the restoration of physiological function [22]. However, the utilisation of staged arthroplasty in cases of gunshot injuries, characterised by gross contamination and a heightened risk of infection, has not been extensively described in the existing literature.
In our case, the staged approach proved instrumental in restoring normal physiology, successfully managing the initial haemorrhagic shock, and mitigating the subsequent acute kidney injury. Given the minimal remaining bone stock and compromised soft tissue, staging allowed for the acute local trauma to heal, creating an optimised environment for subsequent arthroplasty. Furthermore, considering the severity of the soft tissue insult, patient age and comorbidities and the concern regarding PJI due to the initial involvement of pellets, clothing and wad within the shoulder joint, our reconstruction was strategically staged. The initial focus centered on meticulous irrigation and debridement, precise removal of intraarticular bullet fragments, and the local delivery of high-dose antibiotics.
Third body damage and wear from macroscopic and microscopic bullet fragments must be closely monitored and followed up. Third body wear can occur when hard particles such as bone cement particles, bone fragments or other particulate materials become trapped between the articulating surfaces of an implant causing damage to the joint surfaces and accelerating implant wear [23]. The unique nature of gunshot injuries introduces a distinctive set of challenges, in which the characteristics of ballistic fragments may contribute to accelerated wear and damage of the implant components. Close attention to the macroscopic and microscopic aspects of these fragments is essential for comprehensively evaluating treatment outcomes and ensuring the long-term durability of the implant. Upon conducting a thorough literature review, we identified 35 cases where complex fractures from a GSI have been treated with an arthroplasty (Table 2) [14,24-37]. However, we believe that this represents the first documented case of a staged total reverse shoulder replacement following a closerange shotgun injury. Notably, Herry and colleagues detailed two cases involving severe knee gunshot injuries that were initially managed with debridement and the insertion of antibiotic-laden cement spacers, which remained in place for an average of six months. Subsequently, knee megaprostheses were implanted, resulting in a return to nearly full functional capacity with limited flexion [29]. Additionally, Bell et al and Ujvari et al each reported a case involving a severe gunshot injury that resulted in comminuted femoral head and neck fractures, along with a retained intraarticular bullet fragment [25,30]. An antibiotic spacer was left in situ for an average of five months before a total hip replacement was performed. The patient achieved a return to normal activities and remained free of signs of infection at the two-year follow-up.
The analysis of gunshot injuries goes beyond the immediate case, providing insights applicable to diverse scenarios. The observed spray pattern in test shooting (Figure 6) radiographic imaging serves as a valuable tool for estimating gunshot distances universally. This approach can enhance forensic investigations, contributing to a more precise assessment of shooting distances. Understanding these patterns is crucial for clinical decisionmaking, as proximity during gunshot injuries concentrates energy, resulting in deeper, severe local soft tissue damage, while longerrange injuries cause wider, more superficial damage. Close-range wounds typically display flame burns and singeing of hair, whereas distant or far-range wounds may include components other than the lubricant, resulting in the formation of a grease collar [38]. It is important to consider the characteristics of the firearm used to help determine the energy of the injury, prognosis, and treatment of gunshot wounds.
While publications in the literature have been guiding clinicians in the management of shotgun injury to the shoulder, the treatment of complex GSI to the shoulder has not been well established with staged arthroplasty. Severe soft tissue damage and bone loss, haemodynamic instability and numerous retained bullet shrapnel made staged arthroplasty of the shoulder appropriate. Further data and study of similar cases with successful treatment to staged arthroplasty is necessary to validate the staged approach to minimise the risk of infection.
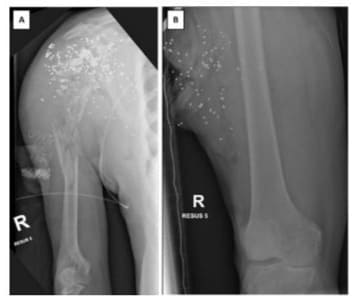
Figure 1: Plain film X-rays obtained upon admission, depicting the right shoulder and right thigh. The images reveal the presence of numerous metallic bullet fragments scattered throughout the soft tissues of the right shoulder and right thigh. Additionally, the X-rays show that the right humeral head and proximal humeral shaft are completely shattered, resulting in the loss of articular integrity. No bony injury is observed in the right femur.

Figure 2: Plain film X-rays depicting the new proximal humeral spacer featuring a 36mm humeral head secured in place with two non-locking screws.

Figure 3: Plain film X-rays displaying the Stanmore DaileyWalker Constrained Reverse total shoulder arthroplasty.
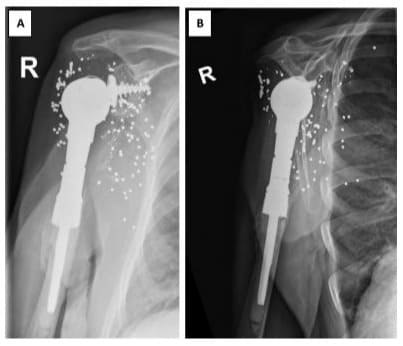
Figure 4: Plain film X-Rays of prosthesis at the nine-month follow up.
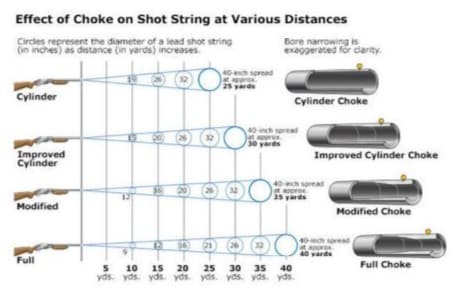
Figure 5: Choke impact on shot string dispersion at varied distances.

Figure 6: Photographs capturing the impact of size 8 shotgun ammunition at controlled distances: 5m, 8m, and 10m. These images provide insight into the shot pattern and aid in determining the likely distance between the shooter and the victim. Note the varying spreads and their implications on the simulated shoulder target.
|
American Size |
Pellet Diameter mm |
Pellet Weight (grains) |
Lead Pellets Per Oz. |
|
11 |
1.57 |
.35 |
1250 |
|
1.68 |
.42 |
1040 |
|
|
10 |
1.78 |
.52 |
848 |
|
9 1/2 |
1.91 |
.63 |
688 |
|
9 |
2.03 |
.75 |
568 |
|
8 1/2 |
2.21 |
.97 |
472 |
|
8 |
2.31 |
1.29 |
399 |
|
7 1/2 |
2.41 |
1.46 |
338 |
|
7 |
2.59 |
1.62 |
291 |
|
6 |
2.79 |
1.99 |
218 |
|
5 |
3.05 |
2.57 |
168 |
|
4 |
3.25 |
3.12 |
132 |
|
3 |
3.43 |
3.65 |
106 |
|
2 |
3.81 |
4.38 |
86 |
|
1 |
4.09 |
5.47 |
71 |
Table 1: Lead shotgun pellets in American sizing system.
|
Author |
Year |
Case |
Age |
Sex |
Side |
Joint affected |
Type of firearm |
Time from injury to arthroplasty (months) |
Type of arthroplasty / Surgery |
Staged approach |
Duration of spacer insertion (months) |
Time to final follow up (months) |
Compli cations |
|
Ujvari et al |
2023 |
1 |
42 |
M |
R |
Hip |
Not stated |
6 |
Total hip arthroplasty |
Y |
6 |
36 |
N |
|
Herry et al [29] |
2015 |
2 |
58 |
M |
R |
Knee |
Low energy gunshot |
15 |
Total knee arthroplasty |
Y |
8 |
60 |
N |
|
3 |
62 |
M |
L |
Knee |
Not stated |
9 |
Total knee arthroplasty |
Y |
3 |
24 |
N |
||
|
Bell et al [30] |
2022 |
4 |
39 |
M |
L |
Hip |
Not stated |
3 |
Total hip arthroplasty |
Y |
4 |
24 |
N |
|
Zandi et al [24] |
2023 |
5 |
35 |
M |
R |
Hip |
Not stated |
12 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
|
Pazarci et al [26] |
2019 |
6 |
43 |
Not stated |
R |
Hip |
Not stated |
8 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
|
7 |
44 |
Not stated |
R |
Hip |
Not stated |
6 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
||
|
8 |
23 |
M |
R |
Hip |
Not stated |
5 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
||
|
9 |
29 |
Not stated |
R |
Hip |
Not stated |
4 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
|
10 |
18 |
Not stated |
L |
Hip |
Not stated |
3 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
||
|
11 |
18 |
Not stated |
L |
Hip |
Not stated |
5 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
||
|
12 |
45 |
Not stated |
L |
Hip |
Not stated |
3 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
||
|
13 |
24 |
Not stated |
L |
Hip |
Not stated |
6 |
Total hip arthroplasty |
N |
N/A |
24 |
N |
||
|
14 |
23 |
M |
L |
Hip |
Not stated |
5 |
Total hip arthroplasty |
N |
N/A |
24 |
Poor functional outcome |
||
|
15 |
32 |
Not stated |
L |
Hip |
Not stated |
4 |
Total hip arthroplasty |
N |
N/A |
24 |
Poor functional outcome |
||
|
Martin et al [27] |
2022 |
16 |
70 |
F |
L |
Hip |
Not stated |
Not stated |
Bipolar hip hemiarthroplasty |
N |
N/A |
18 |
N |
|
Ho et al [28] |
2011 |
17 |
62 |
M |
R |
Hip |
Not stated |
0.39 (12 days) |
Bipolar hip hemiarthroplasty |
N |
N/A |
12 |
N |
|
Dosari et al [31] |
2017 |
18 |
51 |
M |
L |
Shoulder |
Machine gun |
64 |
Reverse shoulder arthroplasty |
N |
N/A |
12 |
Not stated |
|
Amstutz et al [32] |
1981 |
19 |
31 |
M |
L |
Shoulder |
Shotgun |
Not stated |
Anatomic total shoulder arthroplasty |
N |
N/A |
23 |
Not stated |
|
Amri et al [33] |
2019 |
20 |
26 |
M |
L |
Shoulder |
Not stated |
11 |
Resurface shoulder hemiarthroplasty |
N |
N/A |
60 |
N |
|
Haspl et al [34] |
1999 |
21 |
44 |
Not stated |
Not stated |
Shoulder |
Not stated |
36 |
Global endoprosthesis |
N |
N/A |
36-48 (not specified) |
N |
|
22 |
27 |
Not stated |
R |
Shoulder |
Not stated |
20 |
Bi-modular endoprosthesis |
N |
N/A |
36-48 (not specified) |
N |
||
|
Palmer et al [35] |
1986 |
23 |
36 |
M |
R |
Shoulder |
Shotgun |
1 |
Hemiarthroplasty |
N |
N/A |
Not stated |
N |
|
Carroll et al [36] |
2020 |
24 |
32 |
M |
L |
Elbow |
Not stated |
4 |
Interposition arthroplasty with Masquelet technique |
N |
2 |
42 |
N |
|
Demiralp et al [37] |
2007 |
25 |
21 |
M |
Not stated |
Elbow |
Not stated |
32 |
Semi-constrained total elbow prosthesis |
N |
N/A |
122 |
Septic loosening |
|
26 |
23 |
M |
Not stated |
Elbow |
Not stated |
30 |
Semi-constrained total elbow prosthesis |
N |
N/A |
142 |
Aseptic loosening |
||
|
27 |
22 |
M |
Not stated |
Elbow |
Not stated |
16 |
Semi-constrained total elbow prosthesis |
N |
N/A |
107 |
Aseptic loosening |
||
|
28 |
24 |
M |
Not stated |
Elbow |
Not stated |
39 |
Semi-constrained total elbow prosthesis |
N |
N/A |
120 |
N |
||
|
29 |
25 |
M |
Not stated |
Elbow |
Not stated |
14 |
Semi-constrained total elbow prosthesis |
N |
N/A |
115 |
Aseptic loosening |
||
|
30 |
28 |
M |
Not stated |
Elbow |
Not stated |
38 |
Semi-constrained total elbow prosthesis |
N |
N/A |
114 |
N |
||
|
31 |
23 |
M |
Not stated |
Elbow |
Not stated |
14 |
Semi-constrained total elbow prosthesis |
N |
N/A |
94 |
N |
||
|
Zsoldos et al [14] |
2013 |
32 |
22 |
M |
L |
Shoulder |
Shotgun |
1 |
Hemiarthroplasty |
N |
N/A |
Not stated |
Infection, removal of implant, late (24y) attempt at arthrodesis |
|
33 |
36 |
M |
Not stated |
Shoulder |
Shotgun |
Not stated |
Hemiarthroplasty |
N |
N/A |
Not stated |
Infection, removal of implant |
||
|
34 |
21 |
M |
Not stated |
Shoulder |
Hunting rifle |
Not stated |
Hemiarthroplasty |
N |
N/A |
Not stated |
Implant removed for pain + dysfunction, attempted arthrodesis with vascularised fibular graft |
||
|
35 |
42 |
M |
Not stated |
Shoulder |
Shotgun |
Not stated |
Hemiarthroplasty |
N |
N/A |
Not stated |
Infection, removal of implant |
||
|
M: Male, F: Female, N: Nil, N/A: Not applicable |
|||||||||||||
Table 2: Summary of cases of gunshot injury treated with arthroplasty.
Conclusion
Close range shotgun injury to the shoulder is an uncommon pathology resulting in severe soft tissue and bony comminution. Staged reconstruction with an antibiotic spacer and conversion to reverse total shoulder replacement with a megaprosthesis is a viable treatment approach for severe shotgun GSIs resulting in numerous retained bullet shrapnel and comminuted proximal humeral fracture with significant bone loss, that is not amenable to open reduction and internal fixation, to reduce the risk of periprosthetic joint infection.
Conflict of interest: None declared
Data Availability Statement: For queries regarding datasets generated during and/or analysed during the current study, please contact the corresponding author.
Disclosure Statement: None declared
References
- Taş H, Mesci A, Erylmaz M, Zeybak N, Peker Y (2011) The affecting factors on the complication ratio in abdominal gunshot wounds. Ulus Travma Acil Cerrahi Derg, 17: 450-4.
- Negin, J., Bell J, Ivanic L, Alpers P, Nassar N (2021) Gun violence in Australia, 2002-2016: a cohort study. Med J Aust, 215: 414-420.
- Linden, M.A., Manton WI, Stewart RM, Thal ER, Feit H (1982) Lead poisoning from retained bullets. Pathogenesis, diagnosis, and management. Ann Surg, 195: 305-13.
- Baumfel D, Brito AS, Torres MS, Prado KL, Andrade MA, et al (2020) Firearm-Related Fractures: Epidemiology and Infection Rate. Rev Bras Ortop (Sao Paulo), 55:625-628.
- Clasper, J.C, Hill PF, and Watkins PE (2003) Contamination of ballistic fractures: an in vitro model. Injury, 33:157-60.
- Nguyen, M.P., Savakus JC, Donnell JAO, Prayson NF, Reich MS, et al (2017) Infection Rates and Treatment of Low-Velocity Extremity Gunshot Injuries. J Orthop Trauma, 31: 326-329.
- Özden, R., Davut S, Dogramaci Y, Kalaci A, Duman IG, et al (2020) Treatment of secondary hip arthritis from shell fragment and gunshot injury in the Syrian civil war. J Orthop Surg Res, 15: 464.
- Thoresby, F.P. and Darlow HM (1967) The mechanisms of primary infection of bullet wounds. Br J Surg, 1967. 54: 359-61.
- La Garde L.A (1903) Poisoned Wounds By The Implements Of Warfare. Journal of the American Medical Association, 1903. XL: 1062-1069.
- Nechaev, E.A. and Revskoĭ Ak (1993) [Gunshot wound sepsis]. Khirurgiia (Mosk), 1993: 27-32.
- Deitch, E.A. and W.R. Grimes, (1984) Experience with 112 shotgun wounds of the extremities. J Trauma, 24: 600-3.
- Shelton, W.L., Krause P, Fox R, Lowe M, Delatin L, et al (2023) Risk of Infection Following Gunshot Wound Fractures to the Foot and Ankle: A Multicenter Retrospective Study. J Foot Ankle Surg, 62: 50-54.
- Stefanopoulos, P.K., Pinalids DE, Hadjigeogiou GF, Filippakis KN (2017) Wound ballistics 101: the mechanisms of soft tissue wounding by bullets. Eur J Trauma Emerg Surg, 43: 579-586.
- Zsoldos C.M, Basamania CJ, and Bal GK, (2013) Shoulder fusion after a self-inflicted gunshot wound: an injury pattern and treatment option. Bone Joint J, 95-b: 820-4.
- Gandhi R, Backstein D, and Zywiel MG (2018) Antibiotic-laden Bone Cement in Primary and Revision Hip and Knee Arthroplasty. J Am Acad Orthop Surg, 26: 727-734.
- Garvin, K.L. and Konigsberg BS, (2019) Infection following total knee arthroplasty: prevention and management. Instr Course Lect, 61: 4119.
- Srivastav A.K, Nadkarni B, Srivastav S, Mittal V, Agarwal S (2009) Prophylactic use of antibiotic-loaded bone cement in primary total knee arthroplasty: Justified or not? Indian J Orthop, 43: 259-63.
- Bonanzinga T, Tanzi G, Iacono F, Ferrari MC, Marcacci M (2017) Periprosthetic knee infection: two stage revision surgery. Acta Biomed, 88: 114-119.
- Fowler T.J, Sayers A, and Whitehouse MA, (2019) Two-stage revision surgery for periprosthetic joint infection following total hip arthroplasty. Ann Transl Med, 7: S261.
- Franceschini M, Pedretti L, Cerbone V, Sandiford NA (2020) Two stage revision: indications, techniques and results. Annals of Joint, 2020. 7.
- Lindberg-Larsen M (2021) One-stage versus two-stage revision of the infected knee arthroplasty - a randomized multicenter clinical trial study protocol. BMC Musculoskelet Disord, 22: p. 175.
- Mazzucchelli, L., Rosso F, Marmotti A, Bonasia DE, Bruzzone M, et al (2015) The use of spacers (static and mobile) in infection knee arthroplasty. Curr Rev Musculoskelet Med, 8:373-82.
- Cowie, R.M., Pallem N, Briscoe A, jennings LM (2020) Third Body Wear of UHMWPE-on-PEEK-OPTIMA™. Materials (Basel), 13.
- Zandi, R., Talebi S, Ehsani A, Nodehi S (2023) Two-step sequential management for hip arthroplasty after hip joint gunshot injury: A case report. Clin Case Rep, 11: e7569.
- Ujvári B, Olah Z, Molnar S, Hancs T, VarhelyiL, et al (2023) Multi-stage management of a right hip gunshot injury; Case report. Trauma Case Rep, 47: 100881.
- Pazarci, O, Klinic S, Camuruc Y, Bulut O (2019) Total hip arthroplasty after hip joint gunshot injury. J Orthop Surg (Hong Kong), 27:2309499019873113.
- Martin M.P., 3rd, Cole MW, Patel AH, Sherman WF (2022) Gunshot Wound to the Hip Resulting in a Femoral Head and Acetabulum Fracture Treated With Open Reduction and Internal Fixation and Bipolar Hemiarthroplasty. Arthroplast Today, 16: 229-236.
- Ho C.J, Hung SH, Huang HT, Huang PJ, LIN SY, et al (2012) Successful treatment of a delayed presentation of a gunshot injury to the femoral neck in an elderly man: a case report. Eur J Orthop Surg Traumatol, 22:131-3.
- Herry Y., Boucher F, Neyret P, Ferry T, Lustig S (2016) Three-step sequential management for knee arthroplasty after severe ballistic injury: Two cases. Orthop Traumatol Surg Res, 102:131-4.
- Bell C, Skibicki HE, Post ZD, Ong AC, Ponzio DY (2022) Gunshot Wound Resulting in Femoral Neck Fracture Treated With Staged Total Hip Arthroplasty. Arthroplast Today, 14: 44-47.
- Dosari M, Hammed S, Mukhtar K, Elmhiregh A (2017) Reverse shoulder arthroplasty for deltoid-deficient shoulder following latissimus dorsi flap transfer. Case report. Int J Surg Case Rep, 39: 256-259.
- Amstutz H.C., Sew Hoy AL, and Clarke CI, (1981) UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res, 1981: 7-20.
- Amri K, Chefi MA, Znagui T, Rafrafi A, Saadi S, et al (2019) Resurfacing shoulder hemi arthroplasty in ballistic injuries. A case report. Int J Surg Case Rep, 65: 48-51.
- Haspl M, Pecina M, Orlic D, Cicak N (1999) Arthroplasty after war injuries to major joints. Mil Med, 164: 353-7.
- Palmer R.S. and Miller TA (1988) Anterior shoulder reconstruction with pectoralis minor muscle flap. Plast Reconstr Surg,81: 437-9.
- Carroll J.J, Henderson C, Watson J, Larsen K, Kobayashi Ky, et al (2020) Interposition Arthroplasty of the Elbow after Proximal Ulna Reconstruction with the Masquelet Technique: A Case Report. JBJS Case Connect, 10: e0084.
- Demiralp B, Komuruc M, Ozturk C, Tasatan E, Sehrilioglu A, et al (2008) Total elbow arthroplasty in patients who have elbow fractures caused by gunshot injuries: 8- to 12-year follow-up study. Arch Orthop Trauma Surg, 128: 17-24.
- Shrestha, R, Kanchan T, and Krishan K, Gunshot Wounds Forensic Pathology, in StatPearls. 2023, StatPearls Publishing.
- Hunter-ed. Shot String at Various Distances. [Cited 22 Feb 2024].
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.