Glomus Tumors of the Hand: Treatment and Outcomes at Fundacion Santa Fe De Bogota: Case Series
by Tatiana Almario-Aristizabal1,2, Jesús David Perea1, Paula Barragan P1, Fabiana L. Caicedo1, Jorge I. Quintero1-3*, Hand and Microsurgery Research Group
1Department of Orthopedics and Traumatology, Hand and Microsurgery Division, Hospital Universitario Fundación Santa Fe de Bogotá, Bogota, Colombia
2Universidad de los Andes, School of Medicine, Bogota, Colombia
3Universidad del Rosario, Bogota, Colombia
*Corresponding author: Jorge I. Quintero, Fundación Santa Fe de Bogotá, Calle 119 # 7-80 3rd Floor, Bogotá 110111, Colombia
Received Date: 15 January 2025
Accepted Date: 20 January 2025
Published Date: 22 January 2025
Citation: Almario-Aristizabal T, Perea JD, Barragan PP, Caicedo FL, Quintero JI, et al. (2025) Glomus Tumors of the Hand: Treatment and Outcomes at Fundacion Santa Fe De Bogota: Case Series. J Surg 10: 11234 https://doi.org/10.29011/2575-9760.011234
Abstract
Glomus tumors are rare, benign tumors that predominantly affect the hand, with a high incidence at the fingertips, particularly under the nail bed. These tumors are characterized by intense localized pain, often exacerbated by cold exposure, and can lead to significant discomfort and functional impairment. First described by Wood in 1812, glomus tumors arise from the glomus body, a neuromyovascular structure thought to regulate temperature and blood flow in the skin. This retrospective cohort study includes 14 patients diagnosed with glomus tumors between 2010 and 2020 in our teaching hospital. The patients, ranging from 20 to 72 years of age, primarily presented pain in the fingers, with the middle and thumb fingers being the most commonly affected. Nine cases were confirmed histopathological as glomus tumors. Diagnostic imaging, including MRI and ultrasound, was performed in several cases, with MRI offering the highest sensitivity. Surgical resection was the primary treatment. Follow-up revealed that while most patients had no recurrence, two reported nail deformities and occasional cold sensitivity. The study emphasizes the importance of clinical suspicion and detailed examination, particularly for pain and cold sensitivity, in diagnosing glomus tumors. MRI plays a crucial role in diagnosis and surgical planning; clinical evaluation remains keystone. Complete excision of the tumor is key to preventing recurrence, though patients should be counseled about the potential for nail deformities following surgery.
Keywords: Glomus tumors; Hand; Fingers; Resection
Introduction
Wood first described glomus tumors in 1812 as painful subcutaneous nodules characterized by intermittent intense pain, temperature sensitivity, and firm consistency. He proposed excision as the cure. The term “glomus” is derived from Latin, meaning a ball or sphere. In 1920, Masson conducted the first pathological study of glomus tumors, identifying their neuromyovascular origin. [1] These tumors consist of an efferent arteriole, an anastomosed vessel, a primary collecting vein, an intraglomerular reticulum, and a capsular portion. The lesion arises from the glomus body, which regulates skin temperature and circulation. Glomus tumors are rare hand tumors, typically located at the fingertips, and are associated with specific symptoms such as pressure pain and severe cold-induced pain. Diagnosis is often clinical, but imaging techniques like Magnetic Resonance Imaging (MRI) and Doppler ultrasound are used also, these tumors can be associated with vascular malformations detectable through these methods. This study aims to describe clinical diagnosis, additional tests, treatments, recurrence rates, and associated lesions after resection, culminating in histopathological studies.
Materials and Methods
This is a retrospective cohort study. We included patients surgically treated by the Hand and Microsurgery Group at Fundación Santa Fe de Bogotá between 2010 and 2020. Cases of glomus tumors in the hand were identified through pathology reports.
Results
Fourteen patients were diagnosed with glomus tumors via biopsy. Of these, 5 were male and 9 were female, with ages ranging from 20 to 72 years. The most common locations were the fingers, with 5 cases in the long finger, 4 in the thumb, and 2 cases each in the index and ring fingers. No cases were observed in the little finger; one lesion was in the thenar region. Nine of the 14 patients had a clinical diagnosis of glomus tumor confirmed by histopathological evaluation Table 1.The primary symptom was pain, reported by 13 out of 14 patients. Of those 14 patients, one presented a painless mass in the middle finger, with pathology resembling a glomus tumor. Three patients reported cold sensitivity, and Hildreth’s test was documented in one patient. [2] The time from symptom onset to consultation ranged from 5 months to 5 years. No patients had prior surgeries on the affected digit. And the final follow up was up to 5.4 years in our cohort. The most frequent lesion sites were the nail bed (4 cases), subungual region (4 cases), and nail matrix (2 cases). Imaging was obtained for 8 patients. Radiographs (5 cases) were normal in all. MRI was performed in 5 patients, showing findings consistent with a glomus tumor in 2 cases, inconclusive in 2, and unavailable in 1. Ultrasound was performed in 2 patients, with findings consistent with glomus tumors.
|
Cases |
N=14 |
|
Age |
20-72 |
|
Gender |
|
|
- Male |
5 (36%) |
|
- Female |
9 (64%) |
|
Primary diagnosis |
|
|
- Glomus tumor |
9 (64%) |
|
- Thenar mass |
1 (7.1%) |
|
- Soft tissue mass |
2 (14%) |
|
- Right thumb nailbed mass |
1 (7.1%) |
|
Afected Hand |
|
|
- Right |
7 (50%) |
|
- Left |
7 (50%) |
|
Finger |
|
|
- Thumb |
4 (29%) |
|
- Index |
2 (14%) |
|
- Long |
5 (36%) |
|
- Ring |
2(14%) |
|
- Thenar area |
1 (7.1%) |
|
Cold sensation (Pain) |
3 (21.4%) |
|
Pain |
|
|
Yes |
13 (92%) |
|
No |
1 (8%) |
|
Images |
|
|
Yes |
8 (57%) |
|
No |
6 (43) |
|
X-ray simple proyection |
|
|
yes |
7 (50%) |
|
No |
7 (50%) |
|
Ultrasound /Doppler |
|
|
yes |
2 (14%) |
|
No |
12 (86%) |
|
MRI |
|
|
Yes |
5 (35%) |
|
No |
9 (65%) |
|
Pathology |
|
|
Glomus tumor |
13 (93%) |
|
Glomus tumor like |
1 (7.1%) |
|
Recurrency |
1 (7.1%) |
|
Nail Deformity |
2 (15%) |
|
Complication |
None |
Table 1: Demographics, diagnosis, affected hand and finger, recurrency.
Nine patients underwent surgery for a suspected glomus tumor, 2 with a preoperative diagnosis of soft tissue mass, and others with benign tumor, subcutaneous mass, or mucous cyst diagnoses. For the 13 patients with digital lesions, a similar procedure was performed in 8 cases: local anesthesia, tourniquet application, nail plate removal, tumor resection, nail bed repair, and nail plate reinsertion. Thirteen histopathological samples confirmed glomus tumors; one was reported as a lesion resembling a glomus tumor. Twelve of the 14 patients completed follow-up without recurrence.
Two patients reported nail abnormalities, one reported occasional cold-induced pain and slight nail deformity. Two patients did not respond at the end of the study. Ten of the 12 patients reported no residual symptoms. No complications were observed.
Illustrative Case
An illustrative case details the surgical technique. A 40-year-old woman reported thumb pain exacerbated by cold. Thumb X-ray ap and lateral view were normal (Figure 1), and an ultrasound revealed a subungual mass measuring 6.8 x 2.6 x 4 mm (Figure 2). Doppler examination showed increased vascularization (Figure 3). Surgery involved nail plate elevation (Figure 4), proximal incision of the nail bed, tumor exposure and resection (Figure 5), The nail bed was reconstructed, and the nail plate repositioned (Figure 6).

Figure 1: Thumb X-ray. 1a: AP view, 1b: Lateral view.
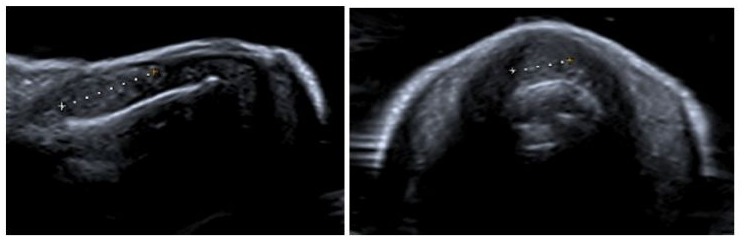
Figure 2: Ultrasound. 2a. Sagital, 2b. Coronal.
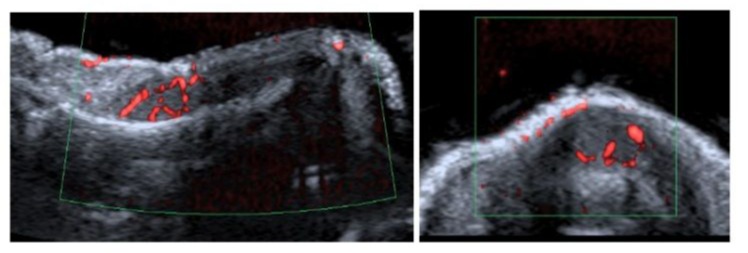
Figure 3: Doppler examination. 2a. Sagital, 2b. Coronal.

Figure 4: nail plate elevation.
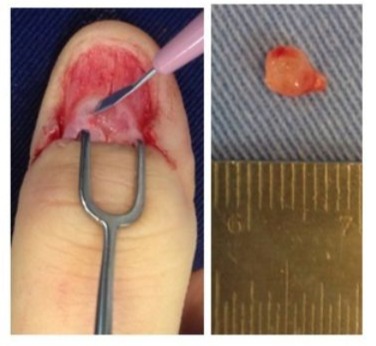
Figure 5: Proximal incision of the nail bed, tumor exposure. 5a. Nail bed incision, 5b. tumor.

Figure 6: Nail bed reconstruction. 6a. Suture with absorbable suture, 6a. Nail plate replenishment.
Discussion
We present a retrospective cohort of glomus tumors of the hand, operated at Fundacion Santa Fe de Bogota. This type of tumor was predominantly found in women, as demonstrated in various case reports, and the average age of presentation ranged between 20 and 72 years. Glomus tumors typically manifest as solitary lesions, most commonly in the subungual region and nail bed. In our case series, the primary location was the nail bed, which is the area with the highest concentration of glomus bodies [1]. Pain was the cardinal symptom and was present in 100% of patients with histologically confirmed glomus tumors. [3,4] According to Chou [5] glomus tumor has the classic triad Love Test, Hildreth test and cold sensitivity test without the need of MRI or Ultrasound and with this symptoms the pathological examination can be 76% glomus tumor. The average consultation time ranged between 6 months and 1 year. When compared to the consultation time reported in the literature, the average time between symptom onset, consultation, and correct diagnosis varies between 4 and 10 years. [6] Although the clinical suspicion of a glomus tumor is key, 8 out of 14 patients underwent some form of imaging x-ray, MRI, or ultrasound to confirm or guide the diagnosis [7,8].
Radiographs in all cases were reported as normal, consistent with prior reviews establishing that radiography is not relevant for diagnosis but is useful for assessing differential diagnoses such as gouty arthritis or foreign bodies (7 patients in this study). [9] There are atypical cases where the glomus tumor may be intraosseous, in which case simple radiography becomes more relevant. MRI was positive in all 5 patients examined, described as a low signal intensity lesion on T1-weighted images and high signal intensity on T2-weighted images. Case series report MRI with a sensitivity of 90% and a specificity of 50% for diagnosing glomus tumors, making it important for lesion characterization and confirmation. However, we recommend that clinical evaluation be prioritized for the accurate diagnosis of this type of tumor [10]. Surgical excision is the treatment for glomus tumor, according to Huang [11] is the curative treatment, usually recurrence is secondary to incomplete excision. Nail deformity is also secondary to a suboptimal excision of the glomus tumor, that is the reason that in all our cases, we performed a transungueal incision removing the nail plate, accessing the nail bed including the proximal nail fold and full excision of the tumor was performed. The same nail plate was used the maintain the nail bed shape. In our cohort no recurrency was observed and Huang cohort about 22 patients none had recurrency and satisfaction was good in 19 of the 23 patients.
In the 14 patients with postoperative follow-up averaging 5.4 years, complete symptoms resolution was observed. Only one patient reported recurrence, presenting with nail deformity and occasional cold sensitivity [12]. These findings align with literature reports of low recurrence and few complications. Recurrence is primarily due to incomplete resection or undetected multiple glomus tumors during the initial evaluation, a situation that can be minimized with the use of MRI. Finally malignant glomus tumors or glomangiosarcomas are rare entity and we should be aware of the risk of metastasis, malignant glomus usually are around the hand and soft tissue bigger than 2 cm, local treatment should include local resection [13].
Conclusion
Glomus tumors of the hand, though rare, present with characteristic symptoms, primarily intense pain and cold sensitivity, which should raise clinical suspicion for early diagnosis. The findings from this study reinforce the importance of a thorough clinical examination, including careful assessment of the nail bed and sensitivity to temperature changes, for identifying these tumors. While imaging techniques such as MRI and ultrasound can confirm the diagnosis and guiding surgical planning, clinical evaluation remains the keystone of diagnosis. Surgical resection, when performed carefully offers excellent outcomes with minimal recurrence, although nail deformities may occur as a postoperative sequela, particularly given the tumor’s common location under the nail. The results of this study highlight that, with complete excision and appropriate follow-up, patients can achieve significant symptom relief and return to normal hand function. Finally, the low recurrence rate and favorable long-term prognosis further underscore the effectiveness of early detection and timely intervention in managing glomus tumors of the hand.
Aknowledgement
The authors wants to thank Constanza L. Moreno-Serrano for the illustrative case images
References
- Carlstedt T, Lugnegard H (1983) Glomus tumor in the hand: A clinical and morphological study. Acta Orthop 54: 296-302.
- Giele H (2000) Hildreth’s test is a reliable clinical sign for the diagnosis of glomus tumours. J Hand Surg Am 27: 157-158.
- Tomak Y, Akcay I, Dabak N, Eroglu L (2003) Subungual Glomus Tumours Of The Hand : Diagnosis And Treatment Of 14 Cases. Scand J Plast Reconstr Surg Hand Surg 37: 121-124.
- Nazerani S, Motamedi MHK, Keramati MR (2010) Diagnosis and management of glomus tumors of the hand. Tech Hand Up Extrem Surg 4: 8-13.
- Chou T, Pan SC, Shieh SJ, Lee JW (2016) Glomus Tumor Twentyyear Experience and Literature Review. Ann Plast Surg 76: 35-40.
- Gandhi J, Yang SS, Hurd J (2010) The Anatomic Location of Digital Glomus Tumor Recurrences. J Hand Surg Am 35: 986-989.
- Mundada P, Becker M, Lenoir V, Stefanelli S, Rougemont AL, et al. (2019) High resolution MRI of nail tumors and tumor-like conditions. Eur J Radiol 2019: 93-105.
- Almeida CÁ De, Nakamura R, Leverone A, Marchiori E (2024) High - frequency ultrasonography for subungual glomus tumor evaluation - imaging findings. Skeletal Radiol 53: 891-898
- Bhaskaranand K, Navadgi BC (2002) Glomus tumour of the hand. J Hand Surg Am 27 : 229-231.
- Al-Qattan M, Al-Namla A, Al-Thunayan A, AF E-S (2005) Magnetic Resonance Imaging In The Diagnosis Of Glomus Tumours Of The Hand. JHS Br Eur 30: 535-540.
- Huang H, Tsai M, Hong K, Chang S, Wang C, et al. (2015) Outcome of Microscopic Excision of a Subungual Glomus. Dermatologic Surg 41: 487-492.
- Lin Y-C, Hsiao PF, Wu Y-H, Scher RK (2010) Recurrent Digital Glomus Tumor: Analysis of 75 Cases. Dermatologic Surg 36: 1396-400.
- Woodward JF, Jones NF (2016) Malignant glomus tumors of the hand. Hand 11: 287-289.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.