Giant Primary Abdominal Wall Hernia: Case Report of the Surgical Treatment with a Review of the Literature
by Johanna CF Willburger 1*, Giacomo L Angelastri 2
1 Department of General Surgery, GZO Wetzikon, Wetzikon, Zurich, Switzerland
2 Department of General Surgery, Luganese Clinica Moncucco, Lugano, Ticino, Switzerland
*Corresponding author: Willburger JCF, Department of General Surgery, GZO Wetzikon, Wetzikon, Zurich, Switzerland
Received Date: 20 November 2023
Accepted Date: 25 November 2023
Published Date: 28 November 2023
Citation: Willburger JCF, Angelastri GL (2023) Giant Primary Abdominal Wall Hernia: Case Report of the Surgical Treatment with a Review of the Literature. Ann Case Report 8: 1526. https://doi.org/10.29011/2574-7754.101526
Abstract
Introduction: Primary abdominal wall hernias can occur in different locations and sizes. The hernia gaps can originate either due to embryonic weaknesses or the yielding of connective tissue due to excessive intra-abdominal pressures. Surgical treatment should be discussed in the event of an emergency situation, disturbing symptoms, or prevention of complications. Case Presentation: In this case report we present a delay treatment of a giant primary ventral abdominal wall hernia, which is rarely seen in Switzerland, due to a normally earlier desired treatment of the patient. Despite delay, treatment could be performed according to the most up-to-date hernia recommendations which are discussed, including a brief review of the literature. Conclusion: A key factor in the successful treatment of large hernias is good communication and clear explanations of the procedure with the patient and his or her relatives. In addition, cooperation between the disciplines involved is crucial for the sometime prolonged follow-up. For an improvement of the evidence in hernia surgery, further case and series reports are essential to be able to offer the best possible care, individualized to our patients.
Keywords: Abdominal-Wall Hernia; Transversus-AbdominisRelease; Poly-4-Hydroxybutyrate Mesh
Abbreviations: ASIS: Anterior Superior Iliac Spin; TAR: Transversus-Abdominis-Release
Introduction
Primary abdominal wall hernia is a worldwide common disease, with an estimated occurrence of 20% in adults [1]. A primary (non-incisional) hernia mostly occurs in the naturally weak points of the abdominal wall. In addition to the inguinal area, this mainly affects the umbilical and epigastric region. There is an indication for treatment in case of incarceration (emergency) or discomfort of the patient. High intra-abdominal pressure (e.g. obesity, chronic cough, chronic obstructive pulmonary disease, vomiting, ascites, pregnancy) can significantly increase the risk of development as well as the size of the hernia sac. Smoking and alcoholism are additional risk factors that should be addressed and minimized, if possible, before treatment is desired [2].
Case Presentation
A 58-year-old male patient presented to our clinic in October 2022 with a huge primary umbilical/ventral hernia (EHS classification M3W3). He reported having the hernia for at least 7-8 years, with rapid increase in size over the past 6 months. Despite the enormous size of the hernia, he had no symptoms until 2 months before presenting in our clinic. The patient also had type 2 diabetes mellitus on medication (metformin 1000mg 3/d; Ozempic 0.75mg 1/week), hypertension, moderate obstructive sleep apnea/ hypopnea syndrome, bronchial asthma, atrial fibrillation (on Eliquis 5mg 1-0-1) and grade III obesity with a BMI of 47.7kg/m2. He had no prior abdominal surgery.
Clinically, we found a huge ventral abdominal wall hernia with the hernia sac starting above the umbilicus (Figure 1).

Figure 1: Pre-Operative clinical finding of the giant ventral abdominal wall hernia. Left in supine position, right standing patient.
The hernia sac overlapped the inguinal/genital region. Preoperative CT scan (24th of October 2022) revealed an abdominal wall hernia with a defect of the abdominal wall measuring 5.5 x 6 cm. The hernial sac included the transverse colon and parts of the small intestine without signs of incarceration. We estimated a loss of domain of 30% bowel outside the abdominal cavity. In addition, there was a small inguinal hernia on the left side. No other relevant pathologic findings. Sections from the CT scan are shown in Figures 2 to 4 to illustrate the size of the hernia (Figure 2-4).
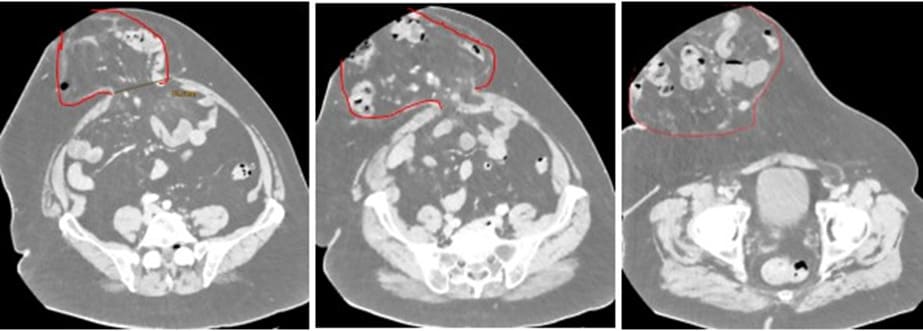
Figure 2: CT-Scan 24.10.22 axial scan left to right - cranial to caudal; red lines illustrating the hernia sac.
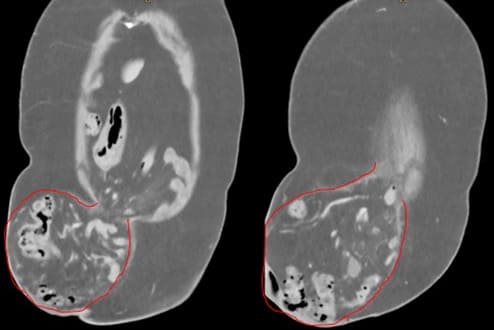
Figure 3: CT-Scan 24.10.22 coronary scan – dorsal to ventral; red lines illustrating the hernia sac.

Figure 4: CT-Scan 24.10.22 sagittal scan; red lines illustrating the hernia sac.
Because of the bizarre findings, we planned early surgical management of the hernia to avoid incarceration or strangulation of the overlapping bowel as well as vascular injury of the small bowel mesentery. For this purpose, we omitted preoperative Botox infiltration, which would have meant delaying the operation another 4-6 weeks. Therefore, we discussed the that in case of significant fascial tension and/or intraoperatively high estimated risk of postoperative abdominal compartment syndrome, a transversusabdominis-release (TAR) would be performed. The patient was informed in detail about the procedure, possible adjustments during surgery, peri- and postoperative complications, especially pulmonary complications, an abdominal compartment and the risk of infection or seroma in the setting of mesh implantation. The patient was also informed about postoperative wound treatment by vacuum dressing, as well as secondary wound closure with corresponding time expenditure.
The patient was in the supine position and under general anesthesia. Disinfection of the abdomen followed by standardized sterile draping. The patient received an i.v. antibiotic injection of Kefzol 3g (1st generation Cephalosporine) preoperatively and repeated Kefzol 1g after 2 and 6 hours. After the routine “team time-out,” a median laparotomy was performed. Especially in the umbilical region there were severe adhesions, which made the separation of the hernia sac from the subcutaneous fat difficult and time-consuming. We entered on the fascia, which was well exposed beyond the hernia-rim. The space in the abdomen was clearly limited, therefore it was evident that a TAR would be necessary to avoid a compartment syndrome by having a tension free closure of the two rectus sheaths in the end. In addition, the decision was quickly made to perform a total omentectomy. The intestines were carefully reduced, the mesentery of the small bowel was totally dislocated. The entire ascending colon, transverse colon and about half of the small intestine were fused to the mesentery within the hernia. Debridement and complete adhesiolysis was performed. Provisional closure of the peritoneum was done to continue with the next step in the sublay-layer. Incision of the left posterior rectus sheath relatively cranially and entering retro-muscular space. This plane was dissected free, bone-to-bone (xiphoid to pubic tuberosity) under precise hemostasis. The same procedure was done on the right side. At this moment it was totally impossible to close the two rectus sheaths. Therefore, the TAR was performed: We started cranially and on the left side. Incision of the posterior rectus sheath about 1 cm away from the margo lateralis under preservation of the small perforating vessels. Visualization of the transverse muscles, which were gradually loaded on a Rommel and cut with electrocautery, from the costal arches downward to beneath the anterior superior iliac spin (ASIS). A decision must be made whether the inguinal hernia treatment on the left side should be performed at the same time: We refrained from doing so because even the largest available Phasix mesh (50 x 50 cm) would have been too short to cover both hernias properly. Since the patient was asymptomatic in this respect, we decided against the additional procedure. Same procedure was done on the right side. Now the intestines were reduced without problems and the rectus sheaths was sutured together without tension. The skin surrounding the hernia sac was removed due to its poor condition (Figure 5) and a radical panniculectomy up to the fascia was performed.
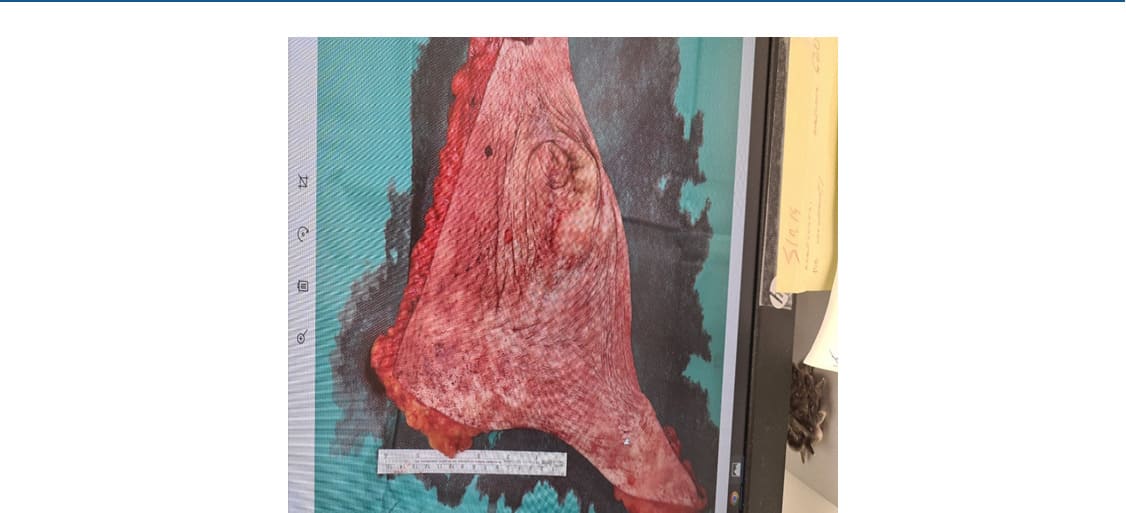
Figure 5: intraoperatively removed skin-flap of poor conditioned skin once covering the hernia-sac.
The closure of the posterior rectus sheath was performed with PDS Loop 2-0 running suture. We trimmed and adjusted the Phasix mesh (43 x 40cm). The fixation of the mesh is done with Prolene 2-0 caudally (ASIS and Lig. Coopery) and laterally. Additional fixation with Vicryl 2-0 in single knot technique and Histoacryl-glue. We inserted in total 4 redon drains on the mesh. After flushing the situs with Ringer-Solution the ventral rectus sheath was closed tension-free by a PDS 1-0 Loop followed by a partial skin closure and installation if a vacuum dressing (-120mmHg).
Postoperatively, the patient was transferred to our intensive care unit for the first night. Thromboprophylaxis was started 6 hours after completion of surgery. A final antibiotic treatment with Kefzol 1g was given 4 hours postoperatively. Two drains were removed on day 3 and the last two on day 4 after surgery. The patient was pain-controlled with a peridural catheter. The preoperatively paused oral anticoagulation was reestablished on day 6. He was discharged home in good condition on day 8. Frequent follow-up was performed in our wound outpatient clinic. The vacuum dressing was successfully removed on 6th of December 2022. Further treatment was with betadine and moist compress. Secondary wound healing was continued with successful results until the end of January 2023 (compare Figure 6).
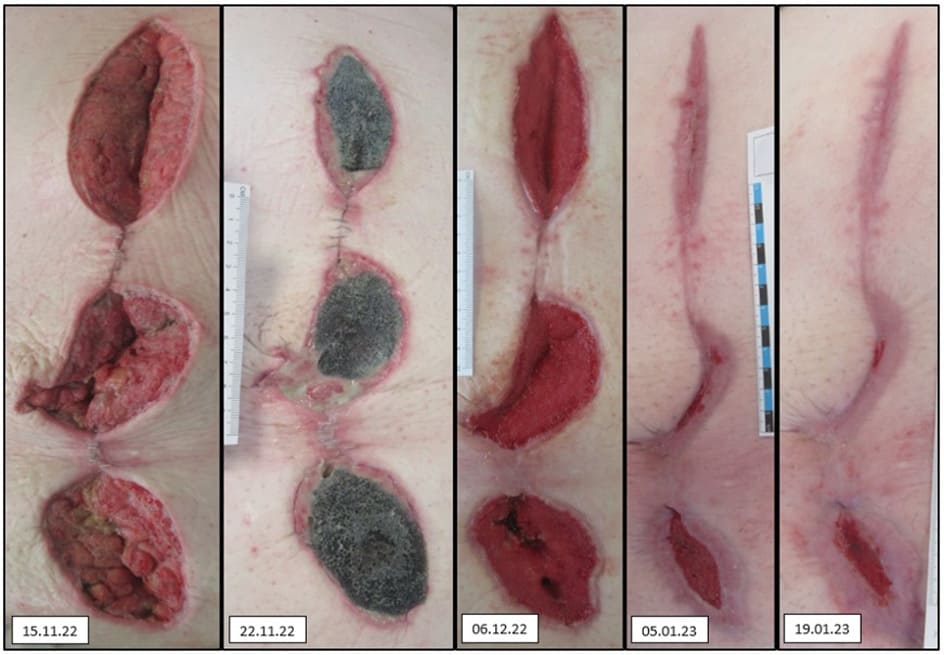
Figure 6: Demonstration of the wound-healing process after surgery.
Our patient was last seen in our hernia consultation in April 2023. He was very satisfied with the surgical result and did not wish any further follow-up visits at present, even though we recommended a yearly follow up to check for recurrence and control the inguinal hernia on the left side. Now there was no evidence of recurrence of the treated abdominal wall hernia with non-irritant and completely healed scars (Figure 7). The patient was asymptomatic and did not need any pain medication. Regarding the existing inguinal hernia on the left, he was still asymptomatic, so we continued to refrain from surgical treatment.

Figure 7: 04/2023 final photo-documentation of the completely closed scar
Discussion
Our patient already had some risk factors due to pre-existing conditions (diabetes, asthma, sleep apnea, obesity), which had to be considered when planning the surgery. An improvement of the situation was not feasible in the foreseeable future, which is why the patient was treated as quickly as possible to avoid possible complications (strangulation, incarceration). Therefore, despite the size of the finding and loss of domain, preoperative conditioning of the abdominal wall by Botox infiltration was not performed, as it would have been recommended in the literature [3].
In the preoperative CT scan, we saw a small inguinal hernia on the left side, which was intentionally not treated in asymptomatic patients as explained. We were aware that this region would be the weakest area of the abdominal wall after the meshing of the ventral abdominal hernia. Perioperatively, we measured the 50x50cm mesh as too small to adequately cover (and overlap) the inguinal region. If the hernia becomes symptomatic and enlarges, we would plan an open procedure such as the Lichtenstein (onlay) technique to avoid surgical complications due to postoperative scarring in the deeper (retromuscular) layers. The patient will be invited yearly in our hernia consultation to monitor the inguinal hernia and to ensure that no complications or new findings occur. There is no guideline recommendation of the management of such rare clinical cases of combined hernias and their surgical management. However, according to current international guidelines for groin hernia management, a watch-and-wait strategy can clearly be chosen for asymptomatic inguinal hernias in men [4]. Therefore, we consider our intraoperative decision in the presented case as justifiable and reasonable to be able to treat the present main problem of the patient without compromise. The patient was informed about the different options depending on the intraoperative situation in a detailed pre-treatment discussion.
The guidelines of the International Endohernia Society for the treatment of ventral abdominal wall hernias of 2014 already recommended the application of perioperative antibiotic therapy with an evidence level of 2b (Grade B), which was reconfirmed in the update of the guidelines in 2019 [5, 6]. This was adhered to in our case, so that 20 minutes before surgery and after 2 and 6 hours of surgery, as well as 4 hours postoperatively the weight-adapted antibiotic therapy with 3g Kefzol i.v. was performed.
To avoid wound infection and postoperative seroma, we decided to do a partial closure (as seen in Figure 6) with the application of a vacuum-assisted closure. In the recent literature, this procedure is recommended especially in large hernias [7], as well as obese patients as it was both presented in this case. We removed the vacuum dressing approx. 1 month after surgery (treatment duration from 04th of October till 6th of December 2022) to continue with the secondary wound healing for another 1.5 months till the healing was finished. There is no existing recommendation about the duration of wound management. Published studies used it either just a few days after surgery [7], or in the case of an onlay mesh until the mesh was completely covered with granulation [8]. We made our decision dependent on the clinical development of the wound, as the mesh was already covered by the fascia in a retro-muscular location. We believe that a strict recommendation in these rare cases might not always be constructive because of an individual healing-progress. However, more publications and shared experience concerning that subject could be helpful in decision making and preoperative communication with the patient.
To be able to perform a tension-free closure of the rectus sheath, a component separation was expected and after the intraoperative finding necessary. For planning a ventral hernia repair in that size, a pre-operative CT Scan it highly recommended to be able to estimate a strategy for a closure. Beside a minimizing of intraabdominal volume, which we did with the omentectomy the component separation is a useful and frequently performed procedure that helps diminishing the tension of the new abdominal wall [9, 10]. We have decided on component separation in terms of a TAR, as it is also frequently done and recommended in cases of large ventral hernias in the current literature. Compared to different types of component separations the TAR got slightly better results in respect of wound infection and other morbidities. Additionally, there are better results concerning the recurrence rate using a TAR in combination with a retro-muscular mesh positioning compared to other methods of techniques [11, 12].
In case of complex ventral hernia repair it is important to use a mesh material that avoids infection and seroma as good as possible. At the same time a low recurrence-rate should be aimed to avoid a re-operation, which is commonly much more complicated and invasive than the first treatment. Beside the clinical outcome, the economic facts should be included in the strategy as well [13]. In our case we decided to take a poly-4-hydroxybutyrate (P4HB) mesh (PhasixTM Mesh 50x50cm, Bard), which is recommended in complicated cases of large ventral hernias. The mesh is a longterm (approx. 2 years) resorbable biosynthetic mesh, which is more economical than biological meshes with a lower infection and seroma rate as shown in the literature [14]. Due to a scarring of the repaired tissue, the strength of the abdominal wall seems to take over the stability after the mesh is resorbed [15, 16] which is shown in follow-ups up to 60 months [17]. The stability of the mesh and the scarring on the tissue after mesh resorption in the presented case will be shown over time and can`t be said at this time.
Conclusion
Summing up the presented case, the key factors for the treatment of the patient and the successful result were the preoperative planning, the integration of the patient through detailed information, and the rapid treatment to avoid complications. In the case of large hernia treatment with a large wound area, prior discussion with the patient regarding a possible longer follow-up is essential for good compliance. We hope to be able to motivate our patients for a yearly follow-up for further post-operative control. In addition, interdisciplinary cooperation first in the operating room, then in our surgical ward, as well as the intensive care in our outpatient wound clinic must be emphasized. With still little literature related to standardized care, recommended mesh material, and procedures in exceptional cases, further case studies, meta-analyses, and randomized control trials would be desirable.
Acknowledgments: None
Ethical Considerations: All the procedures were performed in accordance with the ethical standards of the Declaration of Helsinki.
Conflicts of Interest: The authors declare no conflicts of interest.
References
- Gillies M, Anthony L, Al-Roubaie A, Rockliff A, Phong, J (2023) Trends in Incisional and Ventral Hernia Repair: A Population Analysis From 2001 to 2021. Cureus 15(3);1-10.
- Smith J, Parmely JD (2023) Ventral Hernia. Treasure Island (FL): StatPearls Publishing
- Whitehead-Clarke T, Windsor A (2021) The Use of Botulinum Toxin in Complex Hernia Surgery: Achieving a Sense of Closure. Front Surg 8:753889.
- The HerniaSurge Group (2018) International guidelines for groin hernia management. Hernia 22:1–165.
- Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, et al. (2014) International Endohernia Society (IEHS). Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc 28(1):2-29.
- Bittner R, Bain K, Bansal VK, Berrevoet F, Bingener-Casey J, et al. (2019) Update of Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS))-Part A. Surg Endosc 33: 3069-3139.
- López-Cano M, Armengol-Carrasco M (2013) Use of vacuum-assisted closure in open incisional hernia repair: a novel approach to prevent seroma formation. Hernia 17(1):129-31.
- Tamhankar AP, Ravi K, Everitt NJ (2009) Vacuum assisted closure therapy in the treatment of mesh infection after hernia repair. Surgeon 7:316-8.
- Franklin BR, Patel KM, Nahabedian MY, Baldassari LE, Cohen EI, et al. (2013) Predicting abdominal closure after component separation for complex ventral hernias: maximizing the use of preoperative computed tomography. Ann Plast Surg 71(3):261-5.
- Trakarnsagna A, Chinswangwatanakul V, Methasate A, Swangsri J, Phalanusitthepha C, et al. (2014) Giant inguinal hernia: Report of a case and reviews of surgical techniques. International Journal of Surgery Case Reports 5(11): 868-872.
- Novitsky YW, Fayezizadeh M, Majumder A, Neupane R, Elliott HL, et al. (2016) Outcomes of Posterior Component Separation with Transversus Abdominis Muscle Release and Synthetic Mesh Sublay Reinforcement. Annals of Surgery 264(2): 226–232.
- Chaves CER, Girón F, Conde D, Rodriguez L, Venegas D, et al. (2022) Transversus abdominis release (TAR) procedure: a retrospective analysis of an abdominal wall reconstruction group. Scientific reports 12(1):18325.
- Buell J, Flaris A, Raju S, Hauch A, Darden M, et al. (2021) Long-Term Outcomes in Complex Abdominal Wall Reconstruction Repaired with Absorbable Biologic Polymer Scaffold (Poly-4-Hydroxybutyrate). Annals of Surgery open 2: 1-7.
- Messa CA, Kozak G, Broach GB, Fischer JP (2019) When the Mesh Goes Away: An Analysis of Poly-4-Hydroxybutyrate Mesh for Complex Hernia Repair. Plastic and Reconstructive Surgery - Global Open 7(11): e2576.
- Deeken CR, Chen DC, Lopez-Cano M, Martin DP, Badhwar A (2023) Fully resorbable poly-4-hydroxybutyrate (P4HB) mesh for soft tissue repair and reconstruction: A scoping review; Frontiers in Surgery10:1-19.
- Trapani V, Bagni G, Piccoli M, Roli I, Di Patti F, et al. (2020) Analysis of resorbable mesh implants in short-term human muscular fascia cultures: a pilot study. Hernia 24: 1283-1291.
- Roth JS, Anthone GJ, Selzer DJ, Poulose BK, Pierce R, et al. (2022) Long-Term, Prospective, Multicenter Study of Poly-4-Hydroxybutyrate Mesh (Phasix Mesh) for Hernia Repair in Cohort at Risk for Complication: 60-Month Follow-Up. Journal of the American College of Surgeons 235(6):p 894-904.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.