Giant Cell Tumor of Tendon Sheath: Literature Review, Case Report and Management at the Juarez Hospital of Mexico
by Obed Grajeda*
*Corresponding author: Obed Grajeda, Department of Plastic Surgery, Mexico City General Hospital, Mexico City, Mexico
Received Date: 09 September 2025
Accepted Date: 15 September 2025
Published Date: 17 September 2025
Citation: Grajeda O (2025). Giant Cell Tumor of Tendon Sheath: Literature Review, Case Report and Management at the Juarez Hospital of Mexico. Ann Case Report. 10: 2413. https://doi.org/10.29011/2574-7754.102413
Abstract
Although most tumors of the hand can be diagnosed clinically with a high degree of accuracy, not infrequently the histologic diagnosis may be considerable different than anticipated. Surprised recently by several kind of hands tumor we were stimulated to review our experience at Juarez Hospital of Mexico, a third level hospital in Mexico City. The importance of this case is to highlight the plastic surgeon's experience in hand surgery for the proper management and dissection of tumors of this type to respect healthy anatomy and avoid injury to neurovascular structures that can even lead to amputations. The experience of the hospital's hand surgeons has proven over years that tissue preservation is of vital importance to recover proper function of the affected hand and prevent recurrences. The use of magnifying glasses during the approach helps prevent injuries during surgery. As well as an adequate imaging service that has experience in imaging this type of tumor and distinguishes between the anatomical structures involved for an adequate surgical approach.
Keywords: Hand surgery; Gigant; Cell; Tumor; Tendon; Sheath.
Introduction
Proper teatment depends upon accurate diagnosis. The numerous tissues contained in the small volume of the hand makes the exact tissue of origins of a lesion difficult to ascertain without biopsy [1].
The tumor pathology of my thoracic limb is diverse in location, form, origin, clinical presentation, progression, and treatment. The presence of benign as well as malignant tumor lesions is of clinical importance due to the differences in treatment modalities and, therefore, the functional prognosis of the hand. At the onset of symptoms, the common symptoms of lesions in the upper middle arm are usually treated by other medical professionals before a hand specialist, where the clinical presentation changes. Appropriate pre- and post-treatment can influence the prognosis as well as the patient's aesthetics. Benign lesions in the hand far outnumber malignancies, and this form significantly underestimates malignant pathology [2].
Gigant cell tumor of tendon sheath (GCTTS) is a common lesion of the digits, it is the second most common tumor of the hand after ganglia. Age of presentation is between 30 and 50 years, with a clear female predilection. Typical location is the volar aspect of the and with a propensity for involvement of the radial three digits and the distal interphalangeal joints [3].
Gigant cell tumor of the tendon sheath has had many names including pigmented villonodular tenosynovitis, xanthoma fibrous, xanthosarcoma, fibroma of the tendon and localized nodular synovitis. Traumatic, neoplasic, inflammatory and metabolic causes have been proposed as causes but it is best considered idiopathic. There is no report of becoming malignant. It is characterized histologically by a diverse cell population, including round stromal cells, multinucleated giant cells, and lipid-laden foam cells with deposits of hemosiderin [4].
Morphologically has also been classified into a localized nodular type seen more commonly in the hand and a diffuse type usually seen in larger joints which is multicentric or has satellite lesion without encapsulation. Although uncommon, interosseous invasion of Gigant cell tumors is another morphological factor associated with recurrence. Bony invasion is suspected when radiographs demostrate a multilocular bone defect and coarse sclerotic trabeculae.
Usually the clinical starts as slow-growing, firm with no history of trauma and no associated numbness or tingling painless nodule, however they may affect by proximity with digital nerves or mechanically interfere with hand function [5].
They are less mobile and do not transilluminates unlike ganglions. The affected hand was dominant in two third of the cases [6].
Marginal excision is the treatment of choice; recurrence after marginal excision ranges from 5 to 50%, probably related to the presence of satellite lesion or incomplete excision [7].
Epidemiology
Giant-cell tumour is more common in female in a ratio of 3:2 among the ages of 30 and 50 yeas. GTCTS Is a benign lesion that usually presents in adults and doesn´t affect childrens usually. it mostly occurs in the hands, mainly in the radial fingers, frequently close to the distal interphalangeal joint. Although they can also affect the extensor aspect, tumors prefer the flexor aspect of the hand. Can be lateral or circumferential. Other sites may be affected with less frequency such as the hip, ankle, knee and foot [8].
Diagnosis
The clinical examination of the hand is the keystone of the diagnosis of GCTTS, however may be misdiagnosed or left without definitive diagnosis until intraoperative findings are available. There is no defined radiographic appearance. Ultrasonography shows a solid, homogeneous, hypoechoic tumor generally in relation to the flexor tendons of the fingers with increased vascularity on Doppler mode. Magnetic resonance imaging revels decreased signal intensity on T1- and T2 weighted images. Magnetic resonance imaging is the most definitive imaging study, however it is generally not obtained due to the ubiquity and cost-effectiveness of radiography and ultrasound (Figure 1). GCTTS differs from fibrolipoma of tendon sheath in the non-uniform signal, tumors with uniform signal are more likely to be GCTTS, secund fibrolipoma tumors are strip-like or irregular, while GCTTS are predominantly flaky/granular or separated (Figure 2) [9].
Clinical suspicion of neurovascular budle involvement should arise when the patient experiences pain during the approach. The variability of a preoperative diagnosis of GCTTS between studies indicate a discrepancy in diagnostic techniques. GCTTS found in 5th digit have to be diferentiated from granulomatous lesions, necrobiotic granulomas. The necrobiotic granulomas tumour usually arises in a setting of hyperlipemia and fibroma of the tendon sheath. A histological scoring must be used to differentiate from fibroma of the tendon sheath due to histological similarity [10].
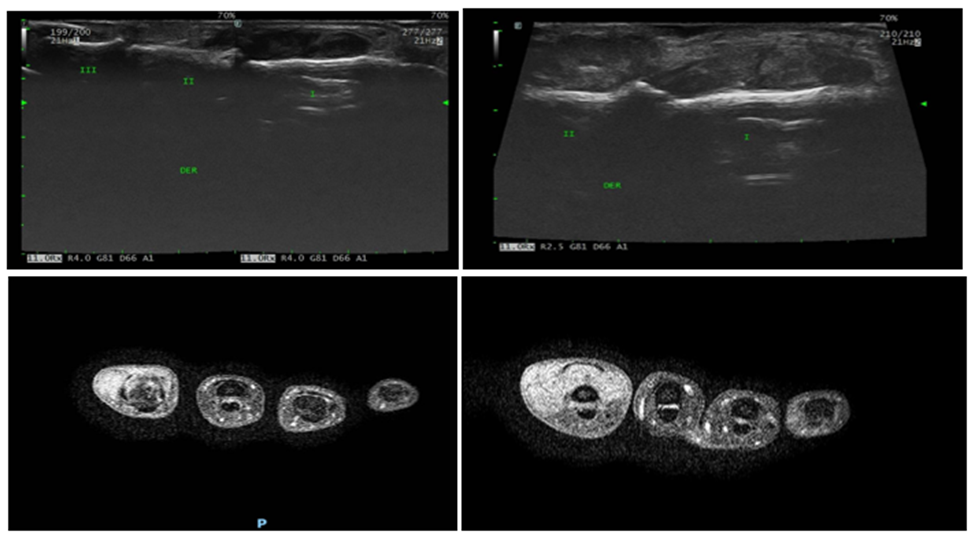
Figure 1: Ultrasound of giant cell tumor of the tendon sheath.

Figure 2: MRI of Affected Hand.
Surgery is the first line of tratment, care must be taken to preserve tissue not affected by the tumor, It is frequently possible to remove the tumor en bloc due to the usual presence of a pseudocapsule, Hand surgeon should actively look for satellite lesions, and if present, these lesions and any suspected connection with the tumor must be removed. Instead of opening the entire site, satelite lesion can be removed using teasing technique, which utilizes gentle, slow dissection. Curettage to remove the cortical shell is recommended if bone degradation has been identify. Flexor and extensor tendons must be repaired if invaded by tumor. Therefore, a balance must be maintained between salvaging tissue and adequately removing tumour margins to prevent recurrences.
Increased recurrence has been associated with a distal joint location of the tumour and direct involvement of the tumour with the extensor or flexor tendon or joint capsule. This is likely due to the increased technical difficulty of excising tumours [11].
Risk factors for recurrence
Complete surgical excision remains the gold standard treatment for GCTSS. Beside incomplete excision and joint envolvment there is no consensus on the effect and contribution identified risk factor for recurrence. Adequate surgical exposure and meticululous dissection provided by magnification loupes are required to lower recurrence rates. Adjuvant therapies such as phenol treatment, radiation therapy and more recently monoclonal antibody therapy have been described to lower recurrence rates but more studies are needed to issue specific recommendations for their uses [12].
Case Report
We present the case of a 41-year-old female patient with a history of systemic arterial hypertension treated with amlodipine and losartan once a day. She began approximately a year ago with a growing, initially as a painless mass on the index finger of the right hand. The slow-growing tumor continued to increase in size and was accompanied by pain at the fingertip, as well as paresthesia during hand activity, limitation of range of motion and sensation of blocking or clicking. She comes to our office and after the medical examination (Figure 3), we request an ultrasound and an MRI to assess the involvement of the neurovascular unit of the finger prior to the surgical approach.
Patient underwent surgery with an S-shaped dorsal access approach above de middle phalanx and extending proximally to the proximal interphalangeal joint. With careful dissection it was observed that the lesion involved ulnar digital nerve, while sparing the extensor tendon complex (Figure 4).
After releasing the edges of the lesion, while avoiding vascular and nerve structure the tumor mass was sectioned horizontally so it could be removed completely (Figure 5). Subsequently, the specimen was sent for histopathological examination, which confirmed the diagnosis of GCTTS.
It is worth noting that in this patient the tumor displaced the neurovascular structures and even surrounded them, so the plastic surgeon's expertise in hand surgery is the main point to highlight for the patient's adequate outcome.

Figure 3: GCTTS.
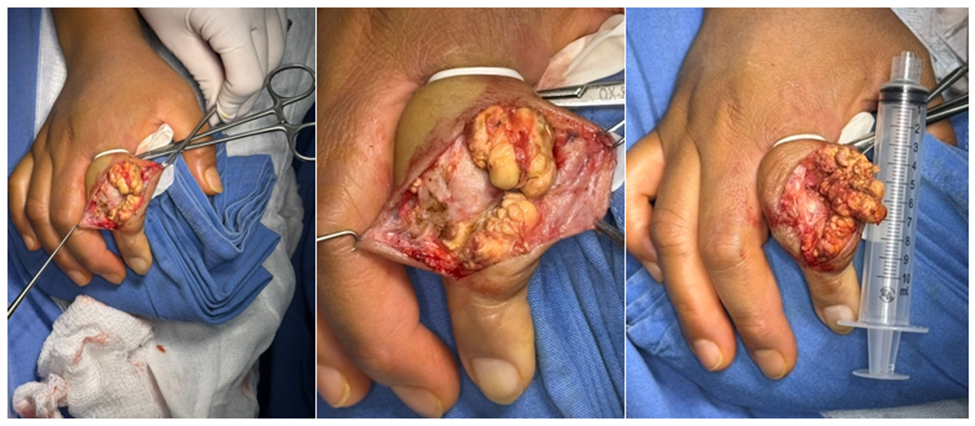
Figure 4: Intraoperative images of giant cell.

Figure 5: After complete dissection.
The histopathological report confirmed the diagnosis of a GCTTS with a multilobulated appearance and a rough surface. When sectioned, the tumor exhibited a smooth surface and an ochre-yellow color alternating with light yellow areas, with a rubbery to semi-firm consistency.
In serial sections, stained with Hematoxylin-Eosin, no residual tissue is identified, only an area of non-encapsulated neoplastic lesion with irregular, poorly defined edges, a homogeneous, hypercellular appearance and abundant hemosiderin. At higher magnification, 3 cell populations are identified, which consist of multinucleated osteoclast-like giant cells, immersed in a stroma with abundant epithelioid-appearing cells (Figure 6) and a single nucleus that resembles that of the previously mentioned giant cells, in addition to hemosiderophages and foamy macrophages (Figure 7).
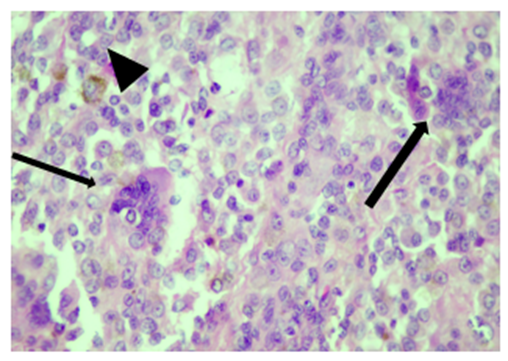
Figure 6: Presence of multinucleated osteoclast-like giant cells (arrows) and a stroma with abundant mononuclear cells with hemosiderophages (arrowhead).

Figure 7: Foamy macrophages. Note the clear cytoplasm indicative of phagocytosis of lipid material.
Discussion
Despite being a widely studied pathology, hand GCTTS treatment remains a challenge for the hand surgeon. The tumor may penetrate into joints bone cortices, can extend into tendon sheaths, and enclose neurovascular structures. Therefore, establishing the balance between complete and aggressive tumour removal along with preservation of vital tissues should be attempted. However, this can be technically challenging to attempt. Surgery should always be performed using magnifying loupes to distinguish between normal tissue and tumor mass to avoid injuries to adjacent healthy structures.
Follow-up was conducted through an outpatient clinic, with satisfactory results in terms of function and aesthetics. The patient remained tumor-free at the 1-year follow-up. We believe that the tissue preservation technique should be considered the standard of care.
This work represents a first step toward publishing a larger case series with longer follow-up and achieving a generalized treatment approach to restore function and prevent amputations and tumor recurrences [13].
Systematic studies have reported a recurrence rate of around 45%. The main factors associated with this recurrence are type II or diffuse lesions, location primarily in the interphalangeal joint of the first finger and the distal interphalangeal joint of the other fingers, as well as location in the flexor sheaths. What we consider to be one of the main factors is the involvement of neurovascular structures, which prevents adequate dissection of the entire tumor.
There is a tendency for the association with degenerative joint diseases due to the increase in histocytes, which makes complete dissection difficult and increases recurrence [14].
Criteria for more aggressive adjuvant approaches such as radiotherapy should be standardized to reduce the risk of recurrence without increasing the risk of neurovascular injury.
Conclussion
During the investigation the following points were identified: 1. Clinical examination and a detailed medical history can be decisive in having an accurate clinical suspicion, but imaging studies remain important, especially in abnormal clinical presentations with pain or atypical cases, in addition to allowing for the distinction between adjacent structures for planning and a more accurate therapeutic approach.
2. As described by Breton et all 2008, Giant cell tumors of the tendon sheath are semi-encapsulated, multilobulated lesions. They can displace other healthy structures, which can make surgical resection difficult, especially to preserve healthy tissue.
3. The use of magnification loupes is essential to reduce the risk of recurrence, as shown in multiple studies, where the main risk factor of recurrence is the presence of residual tumor. Magnification loupes allow for correct identification of tumor tissue and proper dissection and separation of healthy tissue.
Thanks to the pathological anatomy service of the Juarez Hospital in Mexico. Dr. José Rafael Peñavera Hernández, Dr. Luis Fernando Ramos Martínez PGY 3 Dr. Alejandro Osvaldo Hernández PGY1.
Conflict of interest
The research team declares that it has no conflicts of interest.
All personal identifying information of patients has been removed.
We consider our strengths to be a tertiary-level hospital that is a national reference. The availability of a plastic surgeon trained in hand surgery.
Among our weaknesses, we currently do not have complete absorbable monofilament suture material to carry out the proper management according to the guides.
After the excisional biopsy is taken, the nursing staff receives the sample in a sterile glass container with formalin and sends it to the pathology department for analysis. Non-anatomical waste is then stored in a red polyethylene bag, and sharp objects in a rigid polypropylene container. They are then stored in a metal container labeled "Biologically Infectious Hazardous Waste" for no more than 7 days and then disposed of for final disposal. Treated and unrecognizable biologically infectious hazardous waste is disposed of as non-hazardous once treated with physical or chemical methods by facilities authorized by SEMARNAT.
References
- Bogumill GP, Sullivan DJ, Baker GI. (1975). Tumors of the Hand. Clinical Orthopaedics and Related Research, 108: 214-222.
- Bretón GMÁ, Hernández CD. (2008). Lipoma gigante de primer espacio de mano. Diagnóstico diferencial con liposarcoma. Rev Hosp Jua Mex. 75: 230-234.
- Mavrogenis AF, Panagopoulos GN, Angelini A, Lesenský J, Vottis C, et al. (2017). Tumors of the hand. European Journal of Orthopaedic Surgery & Traumatology: Orthopedie Traumatologie, 27: 747-762.
- Lanzinger WD, Bindra R. (2013). Giant Cell Tumor of the Tendon Sheath. The Journal of Hand Surgery, 38: 154-157.
- Tambe S, Bhobe M, Jerajani H. (2015). Giant cell tumor of the tendon sheath mimicking a plexiform neurofibroma. Indian Dermatology Online Journal, 6: 201.
- Adams EL, Yoder EM, Kasdan ML. (2012). Giant cell tumor of the tendon sheath: experience with 65 cases. Eplasty. 12: e50.
- Glowacki KA, Weiss AP. (1995). Giant cell tumors of tendon sheath. Hand Clin. 11: 245-253.
- Khurana A, Singh JP, Preeti LZ, Young S, Shah A. (2023). Demystifying Giant Cell Tumours of Tendon Sheath (GCTTS): A Case Series of 18 Cases with Review of Literature. Indian Journal of Orthopaedics, 57: 1858-1873.
- Ge Y, Guo G, You Y, Li Y, Xuan Y, et al. (2019). Magnetic resonance imaging features of fibromas and giant cell tumors of the tendon sheath: differential diagnosis. European Radiology, 29: 3441-3449.
- Darwish FM, Haddad WH. (2008). Giant cell tumour of tendon sheath: experience with 52 cases. Singapore Med J. 49: 879-82.
- Williams J, Hodari A, Janevski P, Siddiqui A. (2010). Recurrence of giant cell tumors in the hand: A prospective study. The Journal of Hand Surgery. 35: 451-456.
- Ozben H, Coskun T. (2019). Giant cell tumor of tendon sheath in the hand: analysis of risk factors for recurrence in 50 cases. BMC Musculoskeletal Disorders, 20.
- Codesal A, Maldonado JA, Benavente P. (2016). Tumor de células gigantes de la vaina tendinosa de la mano. Estudio de la epidemiología, eficacia de las pruebas de imagen en su diagnóstico y análisis de la recidiva. Revista Iberoamericana de Cirugía de La Mano, 44: 8-12.
- Kolisetty PV, Ali SS, Ahmad I, Sudhy IK, Prakash O. (2024). Giant Cell Tumor of the Tendon Sheath of the Hand: Analysis of Factors Impacting Recurrence. Indian Journal of Plastic Surgery, 57: 123-128.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.