Giant Bezoar in Patient with Trichophagia: Case Report
by Frank Jose Irigoyen Martinez1*, Pedro Guillermo Zuñiga Lopez1, Griselda Catty Luna Ramirez2, Rumy Abel Quispe Quipe1, Carlos Alberto Neira Ortega1, Jesus Miguel Humpiri Paredes1
1Department of General Surgery, ESSALUD III Juliaca, Peru
2Department of General Surgery, Digestive Surgery, ESSALUD III Juliaca, Peru
*Corresponding author: Frank Jose Irigoyen Martinez, Department of General Surgery, ESSALUD III Juliaca, Peru
Received Date: 24 April 2025
Accepted Date: 22 July 2025
Published Date: 25 July 2025
Citation: Martinez FJI, Lopez PGZ, Ramirez GCL, Quipe RBQ, Ortega CAN (2025) Giant Bezoar in Patient with Trichophagia: Case Report. J Surg 10: 11318 https://doi.org/10.29011/2575-9760.011318
Abstract
We present the case of a 17-year-old female patient, initials Q.C.A.F., with a history of untreated trichophagia and previous gastric pathology diagnosed as chronic gastritis, who presented with chronic abdominal pain and gastric mass. The patient had no prior imaging evaluations. Computed Tomography (CT) scan revealed a giant bezoar. The patient underwent emergency surgery, including removal of the bezoar and vertical gastrectomy. Despite the complexity and extent of the surgery, the postoperative course was uneventful. The patient received progressive enteral nutrition and followed the Enhanced Recovery After Surgery (ERAS) protocol. At 6 months of follow-up, the patient had regained her weight and normal gastric function. This case highlights the importance of considering the diagnosis of bezoar in patients with chronic abdominal pain and gastric mass, especially in those with a history of untreated psychiatric and gastric conditions.
Keywords: Bezoar; ERAS protocol; Surgical management; Trichophagia
Bezoar Description
A stomach bezoar is a mass of foreign material, often composed of hair or fiber, that is ingested and accumulates in the stomach, failing to pass through the intestines [1-4]. It is also defined as a compact mass of partially digested or undigested material that cannot exit the stomach [5].
Types of Stomach Bezoars
- Hair bezoar or trichobezoar: It is the most common type and is formed when hair is ingested, which accumulates in the stomach and is not digested.
- Fiber bezoar or phytobezoar: Formed when large amounts of fiber are ingested, which then accumulate in the stomach without being digested.
- Symptoms of stomach bezoar
- Chronic abdominal pain
- Abdominal mass
- Nausea and vomiting
- Weight loss
- Difficulty digesting food
Treatment of Stomach Bezoar
Treatment of stomach bezoar depends on the type and size of the bezoar, as well as the presence of complications. It may include:
- Medical treatment: For small bezoars, medication may be used to attempt to dissolve the bezoar.
- Surgery: For large bezoars or those causing intestinal obstruction, surgical management may be necessary to remove the bezoar.
Case Presentation
A 17-year-old female patient presented with chronic abdominal pain that had worsened over the past 4 days. The pain was described as a feeling of discomfort and heaviness in the upper abdominal region, without radiation to other areas. The patient has a history of psychiatric pathology related to trichophagia (hair ingestion) since the age of 8, which has not been adequately treated [6-10].
Diagnosis
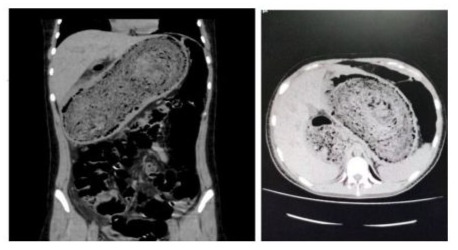
The patient underwent an abdominal Computed Tomography (CT) scan, which revealed a large, well-defined mass in the stomach, with an approximate diameter of 30 cm. The mass had a homogeneous density and showed no signs of necrosis or ulceration. The sagittal CT scan revealed dilation of the gastric chamber by a foreign body compatible with a bezoar [11,12]. Based on the CT scan results, it was decided to defer performing an endoscopy and proceed directly with surgical management.
Treatment
The patient underwent emergency surgery for the removal of the bezoar. The procedure was performed under general anesthesia and consisted of a median supraumbilical laparotomy. During the surgical management, an intestinal perforation was discovered in the greater curvature of the stomach, with the presence of localized peritonitis [13-15]. Due to the extensive damage, necrotic edges, and chronic inflammation of the gastric wall, it was decided to perform a vertical gastrectomy, removing 60% of the gastric cavity. The surgical procedure was completed without complications. The patient tolerated the surgery well and was transferred to intermediate care for necessary recovery and postsurgical management [16].
Results
Despite the complexity and invasiveness of the surgery, the postoperative course was uneventful. The patient received progressively advanced enteral nutrition and was managed according to the Enhanced Recovery After Surgery (ERAS) protocol. At six months of follow-up, the patient had regained her weight and normal gastric function [17-20].
Appendices
Images (Tomografy)
Histopathological report corresponding to request No. 49477 from EsSalud Juliaca.
Slide code: 24Q-746.
1. Stomach - Partial Resection
• Gastric perforation associated with severe, diffuse chronic gastritis and peritonitis.
Macroscopic Description: A specimen labeled with the patient’s name, consisting of a partial gastrectomy, was received in formalin. The specimen measures 15 × 8 × 4 cm. The serosal surface is grayish and smooth. The superior margin measures 10 cm, and the inferior margin 9 cm. The specimen is opened along the greater curvature and displays a firm consistency. A perforation is identified in the gastric fundus, measuring 1.2 cm in diameter.
2. Received separately in formalin and labeled with the patient’s name is a gastric trichobezoar measuring 30 × 10 × 9 cm and weighing 3,565 grams. The specimen consists of a compact mass composed of hair and food debris.

References
- Iwamuro M, Okada H, Matsueda K (2015) Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc 7: 336-345.
- Keramidas D, Voyatzis N, Lazarides S (2018) Gastric bezoars: A review of the literature. J Clin Gastroenterol 52: 539-545.
- Lohse B, Kohler G, Schmitz B (2018) Trichobezoar - a rare cause of gastric outlet obstruction. J Med Case Rep 12: 123.
- Chisholm E, Richards D, Cunningham A (2019) Bezoars: A review of the literature and a case report. J Surg Case Rep 2019: rjz126.
- Kumar A, Chaudhary A, Gupta A (2020) Gastric bezoar: A rare cause of abdominal pain. J Clin Diagn Res 14: OE01-OE03.
- Andrus CH, Ponsky JL (1988) Bezoars: classification, pathophysiology, and treatment. Am J Gastroenterol 83: 476-478.
- Walker-Renard P (1994) Update on gastrointestinal bezoars. Gastroenterol Clin North Am 23: 935-946.
- Erzurumlu K, Malazgirt Z, Bektas A (2005) Gastrointestinal bezoars: a retrospective analysis of 34 cases. World J Gastroenterol 11: 18131817.
- Gayer G, Jonas T, Apter S (1999) Bezoars in the stomach and small bowel - CT appearance. Clin Radiol 54: 182-188.
- Chintamani, Tendon S, Singhal V (2003) Gastric bezoar: a rare cause of gastric outlet obstruction. J Postgrad Med 49: 267-268.
- Kadiyala M, Rajagopal C, Rao S (2004) Bezoars - a review of 15 cases. Indian J Surg 66: 269-273.
- Ladas SD, Triantafyllou K, Tzathas C (2010) Gastric bezoars treated endoscopically: a case series. World J Gastrointest Endosc 2: 179183.
- Kochar R, Banerjee S, Chakravarti A (2011) Gastric bezoar: a rare cause of abdominal pain in children. J Pediatr Gastroenterol Nutr 53: 432-435.
- Rodríguez G (2018) Bezoar gástrico gigante. Presentación de un caso. Rev Cubana Cir 57: 1-5.
- Gómez-Rosado J (2019) Bezoar gástrico, una aproximación al manejo. Rev Gastroenterol Mex 84: 155-162.
- Jiménez-Sáenz M (2017) Metalobezoar como causa de abdomen agudo. Presentación de un caso. Rev Esp Enferm Dig 109: 651-654.
- González-Huix F (2018) Tratamiento endoscópico de bezoares gástricos. Rev Gastroenterol Mex 83: 247-253.
- Castaño-Milla C (2019) Bezoar gástrico como causa de obstrucción intestinal. Rev Colomb Gastroenterol 34: 147-152.
- Fernández-Arquero M (2018) Bezoar gástrico en pacientes con trastornos alimentarios. Rev Psiquiatr Psicol Clin 23: 83-88.
- Díaz-Tasende J (2019) Diagnóstico y tratamiento de bezoares gástricos. Rev Gastroenterol Hepatol 34.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.