Funguria. Nitroxoline an Option for the Treatment of Fluconazole Resistant Fungal Species, for Example Trichosporon spp.
by Herbert Hof*
MVZ Labor Limbach u. Kollegen, Im Breitspiel 16, 69126 Heidelberg, Germany
*Corresponding author: Herbert Hof, MVZ Labor Limbach u. Kollegen, Im Breitspiel 16, 69126 Heidelberg, Germany.
Received Date: 06 September 2025
Accepted Date: 16 September 2025
Published Date: 19 September 2025
Citation: Hof H (2025) Funguria. Nitroxoline an Option for the Treatment of Fluconazole Resistant Fungal Species, for Example Trichosporon spp. Infect Dis Diag Treat 9: 278. https://doi.org/10.29011/2577-1515.100278
Keywords: Candida albicans; Candida glabrata; Trichosporon asahii; Fluconazole; Nitroxoline
Introduction
Bacteria are the most common causes of urinary tract infections; among them uropathogenic strains of Escherichia coli are the most frequent ones. Fungi are also found in microbiologic cultures of urines and indeed not seldomly. Generally, yeasts especially ascomycetic ones predominate; moulds are only occasionally detected. Risk factors for funguria are vesicular catheters, obstruction, hospitalisation, particularly in intensive care units, diabetes, old age and prior treatment with antibiotics [1-3]. Unfortunately, only few antimycotics achieve sufficient concentrations in the urinary tract. Hence, therapy of funguria is sometimes difficult. This holds especially true for infections with fungi moderately or even resistant to certain antimycotics, such as the basidiomycetic Trichosporon spp., in particular Trichosporonasahii.
The role of nitroxoline, in fact an antibiotic, for the treatment of funguria is largely underestimated, although this drug is generally active against most yeasts [4].
Laboratory results
Urine specimens send to the laboratory Limbach, Heidelberg/ Germany in 2023 were cultured according to the recommendations of the AWMF guideline [5]. The differentiation was done by MALDI-TOF (Bruker, Bremen/Germany).
The majority of fungal isolates from urine were found in specimens from hospitalized patients afflicted obviously with certain risk factors (table 1). The species Candida albicans was isolated most frequently followed by Candida glabrata. Other species were definitely less common (table 1). Candida auris was not detected in this survey. Trichosporon asahii, a basidiomycetic yeast, was found in 3 hospitalized patients.
|
species |
hospitals |
medical practices |
dialysis centers |
|
total |
2 060 100% |
443 100% |
133 100% |
|
C. albicans |
1 243 60% |
226 51% |
60 45% |
|
C. glabrata |
398 19% |
101 23% |
19 14% |
|
C. tropicalis |
144 7% |
17 4% |
12 13% |
|
C. krusei |
110 5% |
36 8% |
18 14% |
|
C. parapsilosis |
63 3% |
21 5% |
8 6% |
|
C. lusitaniae |
16 1% |
4 1% |
5 4% |
|
C. dubliniensis |
16 1% |
8 2% |
1 1% |
|
Saccharomyces |
42 20% |
15 4% |
9 7% |
|
annotation: among the various yeasts also 3 isolates of Trichosporon asahii were detected namely in hospitalized patients. |
|||
Table 1: Yeasts isolated from urinary cultures in 2023 submitted by different senders (Laboratory Limbach Heidelberg).
T. asahii is susceptible in vitro to nitroxoline, since in an agar diffusion test the diameter of the inhibition zone was > 17mm (figure 1).
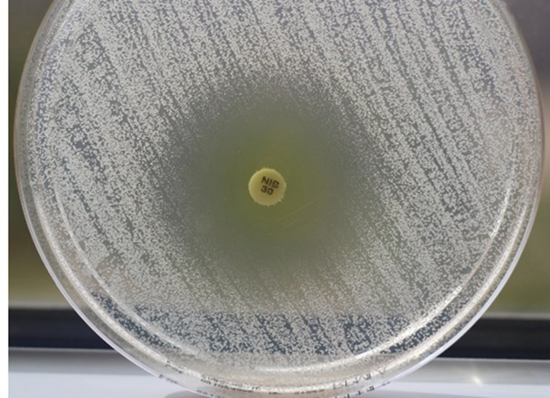
Figure 1: In vitro activity of nitroxoline against Trichosporon asahii (agar diffusion test).
Discussion
Yeasts were found often in urine specimens especially from hospitalized patients (table 1). By far the most prevalent yeast species in this series was C. albicans, amongst various other species (table 1). Principally, still other species such as C. auris also can be present [8]. The yeast T. asahii as well as other species can be isolated occasionally in urine [Table 1; 4, 6-16]. Obviously, patients with chronic kidney diseases are particularly susceptible for those fungi [17]. Elderly people [6,13,15] as well as diabetic persons [7,9,13] are also at risk. One has to keep particularly in mind nosocomial cases [17].
Not each funguria needs imperatively antimycotic treatment, since patients are often asymptomatic [18]. This holds especially true for the presence of Saccharomyces spp., which will indicate a mere colonization (table 1). Indeed, often an overtreatment can be observed [19,20]. On the other hand funguria in patients with severe underlying diseases, for example patients in an intensive care unit or with anomalies of the urinary tract or with medical devices in the urinary tract such as indwelling catheters, may require an antimycotic therapy, because otherwise the risk of a threatening fungemia may emerge. In cases of fungal urinary infections requiring antimycotic therapy usually fluconazole is applied according to expert opinions [4].
Nevertheless, the rising frequency of fluconazole-resistant C. albicans represents a growing obstacle for successful treatment [21]. In addition, there are species found in urines such as Candida glabrata, Candida krusei (Pichia kudriavzevii), Candida parapsilosis (table1) and Candida auris which tend to be a priori resistant to fluconazole [8,21-23] as well as to other antimycotics. Furthermore, absolutely fluconazole resistant strains of otherwise susceptible yeasts arise steadily [11]. T. asahii strains, are, in general, moderately susceptible to fluconazole [14,15] but resistant strains also exist [11]. Hence, it can be anticipated that the common fluconazole therapy will not be effective for certain urinary infetions. While voriconazole and posaconaole can be used for therapy of systemic infections with these yeasts [14,15], these drugs fail in case of a urinary infections, because these azoles are preferentially eliminated via the bile tract and only minimal amounts are excreted unmodified into the urinary tract (product information). T. asahii is, however, inherently susceptible to nitroxoline (figure 1) an antibiotic approved for the treatment of urinary tract infections at least in certain countries [24] and indicated even in infections with multidrug resistant E. coli [25]. Indeed, an effective therapy of T. asahii in urine is required occasionally, since T. asahii possesses indeed a lot of virulence factors so that funguria can finally cause fungemia [17]. Hence, for the treatment of funguria with fluconazole resistant or moderately susceptible yeasts – among them T. asahii - nitroxoline, an antibiotic achieving high urinary concentrations [4] represents a suitable alternative. By the way nitroxoline can be used even in case that a susceptibility testing is not feasible, since it is reliably effective against practically all medically relevant yeasts [4] even C. auris [8].
Furthermore, indwelling catheters can be colonized by yeast biofilms, where azoles including fluconazole are inactive [26], whereas nitroxoline is principally active against microorganisms in biofilms [27].
Summary
Yeasts are present in urine rather frequently; therapy is, however, not indicated in every case, since in most instances colonization remains asymptomatic. In case that an antimycotic therapy is stringent, usually flucanzole is used. But one has to foresee the presence of fluconazole resistant species; in addition, fluconazole is not active against pathogens in biofilms. Although funguria by fluconazole resistant T. asahii is rather rare this yeast species is difficult to treat with conventional antimycotics. Nitroxoline, which is eliminated principally via the urinary tract and effective against most yeasts even in biofilms, would be the drug of choice, if treatment is indicated, i.e. in case that risk factors for dissimination exist.
References
- Bukhary ZA (2008) Candiduria: A Review of clinical significance and management. Saudi J Kidney Dis Transplant 19:350-360.
- He Z, Su C, Bi Y, Cheng Y, Lei D, et al. (2021) Evaluation of a novel laboratory candiduria screening protocol in the Intensive Care Unit. Infect Drug Resist 14:489-496.
- Sobel JD, Fisher JF, Kauffman CA, Newman CA (2011) Candida urinary tract infections—epidemiology. Clin Infect Dis 52:S433–S436.
- Hof H (2017) Candidurie! Was nun? Zur Therapie von Harnwegsinfektionen durch Candida. Der Urologe 56: 172179.
- AWMF S3-Leitlinie Epidemiologie, Diagnostik, Therapie, Prävention und Management unkomplizierter, bakterieller, ambulant erworbener Harnwegsinfektionen bei Erwachsenen (HWI). Reg. no. 043-044 (2024).
- Acampora N, Frizza A, Brau F, Torelli R, Vella A, et al. (2019) A case of Trichosporon asahii urinary tract infection in a frail elderly patient. Infez Med 27: 93-96.
- Adhikari S, Saud B, Paudel G, Wagle S (2019) A rare case of recurrent urinary tract infection due to Trichosporon species in an immune-competent diabetic female patient. Arch Case Rep 3:26-28.
- Fuchs F, Hof H, Hofmann S, Kurzai O, Meis JF, et al. (2021) Antifungal activity of nitroxoline against Candida auris isolates. Clin Microbiol Infect 27: 1697.e7-1697.e10.
- Iken M, Belkouch A, Bellarj B, Naoui H, Boumhil L, et al. (2015) A rare case of urinary tract infection due to Trichosporon asahii in a diabetic patient. Pan Afr Med J 20:127.
- Khan ID, Sahni AK, Basu A, Haleem S (2015) Trichosporon asahii urinary tract infection in immunocompetent patients. Med J Armed Forces India 71: 373-376.
- Li T, Huang Y, Chen X, Wang Z, Xu Y (2020) Urinary Tract Infections Caused by Fluconazole-resistant Trichosporon japonicum in 2 kidney transplant patients and analysis of their homology. Open Forum Infect Dis 7: ofaa365.
- Oliveira dos Santos C, Zijlstra JG, Porte RJ, Kampina GA, van Diepeningen AD, et al. (2016) Emerging pan-resistance in Trichosporon species: a case report. BMC Infect Dis 16:148.
- Subramanian A, Sheela Devi, Abraham G, Honnavar P (2021) Trichosporon asahii infection associated with glomerulonephritis in a diabetic patient. Med Mycol Case Rep 35:15-17.
- Treviño M, García-Riestra C, Areses P, Garcia X, Navarro D, et al. (2014) Emerging Trichosporon asahii in elderly patients: epidemiological and molecular analysis by the Diversi-Lab system. Eur J Clin Microbiol Infect Dis 33:1497-1503.
- Turan D, Barış A, Özakkaş F, Dinçer ŞD, Aksaray S (2021) Investigation of antifungal susceptibility of Trichosporon asahii isolated from urine samples. Med J Bakirkoy 17:130-134.
- Urs TA, Kadiyala V, Deepak S, Karthik MK (2018) Catheter associated urinary tract infections due to Trichosporon asahii. J Lab Physicians 10:464-470.
- Hassan H, Nair LA, Varsha NS, Jyothi R, Aravind R, et al. (2024) Trichosporon infection in chronic kidney disease patients from a tertiary care hospital – a case series or an outbreak? An unanswered question but a well-managed problem. GMS Infect Dis 12: Doc05.
- Kaufmann CA (2005) Candiduria. Clin Infect Dis 41: S371-376.
- Castellano-Sánchez L, Rosales-Castillo A, Marcos-Rodríguez R, Olvera-Porcel MC, Navarro-Marí JM, et al. (2025) Microbiological relevance of Candida in urine cultures. J Fungi 11:483.
- Jacobs DM, Dilworth TJ, Beyda ND, Casapao AM, Bowers DR (2017) Overtreatment of asymptomatic candiduria among hospitalized patients: a multi-institutional study. Antimicrob Agents Chemother 62: e01464-17.
- Akinosoglou K, Livieratos A, Asimos, K, Donders, F, Donders GGG (2024) Fluconazole-resistant vulvovaginal candidosis: an update on current management. Pharmaceutics 16:1555.
- Daneshnia F, de Almeida Júnior JN, Ilkit M, Lombardi L, Perry AM, et al. (2023) Worldwide emergence of fluconazoleresistant Candida parapsilosis: current framework and future research roadmap. Lancet Microbe 4: e470-e480.
- Ratner JC, Wilson J, Roberts K, Armitage C, Barton RC (2025) Increasing rate of non-Candida albicans yeasts and fluconazole resistance in yeast isolates from women with recurrent vulvovaginal candidiasis in Leeds, United Kingdom. Sex Transm Infect 101:21-26.
- Krajewski W, Łaszkiewicz J, Tomczak W, Nowak Ł, Chorbińska J, et al. (2024) Nitroxoline: treatment and prevention of urinary tract infections from the urologist’s perspective. Cent European J Urol 77:339-343.
- Hof H, Juretschke C (2019) Nitroxoline: an option for the treatment of urinary tract infection with multi-resistant uropathogenic bacteria. Infection 47:493-495.
- Mannan M, Nabeela S, Mishra R, Uppuluri P (2024) Host immune response against fungal biofilms. Curr Opin Microbiol 81:102520.
- Sobke A, Klinger M, Hermann B, Sachse S, Nietzsche S, et al. (2012) The urinary antibiotic 5-nitro-8-hydroxyquinoline (Nitroxoline) reduces the formation and induces the dispersal of Pseudomonas aeruginosa biofilms by chelation of iron and zinc. Antimicrob Agents Chemother 56:6021-6025.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.