Fully Embedded IUD: Hysteroscopic Management Using X-ray
by Caroline S Kwon1*, Lily S Bender2, Lauren D Schiff3
1Department of Minimally Invasive Gynecologic Surgery/University of North Carolina Hospitals/University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
2Department of Obstetrics and Gynecology/University of North Carolina Hospitals/University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
3Department of Minimally Invasive Gynecologic Surgery/University of North Carolina Hospitals/University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
*Corresponding author: Caroline S Kwon, Department of Minimally Invasive Gynecologic Surgery/University of North Carolina Hospitals/University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Received Date: 14 September 2024
Accepted Date: 18 September 2024
Published Date: 20 September 2024
Citation: Kwon CS, Bender LS, Schiff LD (2024) Fully Embedded IUD: Hysteroscopic Management Using X-ray. Ann Case Report. 9: 1979. https://doi.org/10.29011/2574-7754.101979
Abstract
IUDs are highly effective long-acting reversible contraceptives, valued for their efficacy, ease of use, and suitability for postpartum placement. However, malpositioning can occur. In severe cases, an IUD may become fully embedded in the uterine wall, presenting a unique challenge that often necessitates removal in the operating room. Real-time intraoperative X-ray can be an invaluable tool for confirming the IUD’s exact location and ensuring accurate dissection planes. This presentation will highlight key surgical steps and important takeaways through a case study.
Keywords: Malpositioned IUD; Hysteroscopy; Imaging; Surgical Approach.
Introduction
IUDs are highly effective long-acting reversible contraceptives, valued for their efficacy, ease of use, and suitability for postpartum placement. However, malpositioning can occur, with some studies reporting rates of up to 10.4% [1].
Malpositioning can present in various ways: the IUD frame may rotate on its axis or shift transversely, with the arms unfolded or extended in different positions. Non-fundal IUDs are commonly located in the lower uterine segment or cervix, often identified through ultrasonography.
In cases of displacement, the arms of an IUD might become embedded in the uterine wall or even perforate it, potentially
embedding in the bowel or other intraperitoneal structures [2]. Symptoms of malposition can include changes in bleeding patterns and pain, though the severity of symptoms varies, and not all patients may be aware of the malposition. If an IUD is confirmed to be embedded in the uterine wall, it may often be removed in the office by grasping the strings with a clamp and applying gentle traction. If removal is difficult with moderate traction or if the strings are not visible, hysteroscopic removal is the next step, which may be performed in the office or the operating room, depending on the complexity. In complex cases where IUD location is uncertain, intraoperative imaging may be required.
We report a case that demonstrates the use of intra-operative radiographic imaging to guide the dissection and removal of a fully embedded IUD. We also discuss the key surgical steps involved in addressing an embedded IUD.
Case Presentation
A 37-year-old G0 patient presented for hysteroscopic removal of a fully embedded Mirena IUD. She had previously undergone a robotic myomectomy while the IUD was in place and a uterine manipulator was used. Three months post-operatively, she reported electric-type uterine pain. Upon examination, the IUD strings were not visible at the cervix, leading to a hysteroscopic investigation. This revealed the strings protruding into the cavity from the posterior uterine wall. Attempts to remove the IUD hysteroscopically by pulling on the strings were unsuccessful, resulting in detachment of the strings and leaving the cavity appearing normal.
The patient then sought consultation for a re-attempt at surgical removal. Prior to the procedure, a CT pelvis was performed to assess the distance of the IUD from the serosa and the uterine cavity to determine the appropriate surgical approach. The CT scan, chosen over MRI based on the radiologist’s recommendation, confirmed the presence of the IUD within the uterus but reported it as normally placed in the cavity, despite direct visualization suggesting otherwise. The patient was subsequently consented for both hysteroscopic and potentially robotic retrieval of the embedded IUD.
We began the procedure with a hysteroscopic approach. The hysteroscope was inserted through the cervix and guided into the uterine cavity. Upon inspection, the Mirena IUD was not visible.
Next, we introduced the MyoSure Reach device into the cavity. Using the device’s tip, we palpated the posterior uterine wall where the IUD strings were seen prior to detachment. To precisely locate the IUD, portable X-ray imaging was performed with the MyoSure device in place to serve as a reference point.
We then systematically excised endometrial tissue at the radiographic site of the IUD, taking multiple X-ray images throughout the dissection to confirm the accurate location of the IUD in reference to the MyoSure instrument and to ensure precise dissection planes. Once a portion of the IUD was exposed, we carefully resected the surrounding tissue to liberate a significant part of the device. Hysteroscopic forceps were used to completely remove the IUD. It was found to be lying parallel to the uterine wall, requiring a larger area of exposure to achieve adequate traction for removal. Notably, we injected vasopressin into the myometrium with a hysteroscopic needle to decrease blood loss during dissection (Figures 1-5).
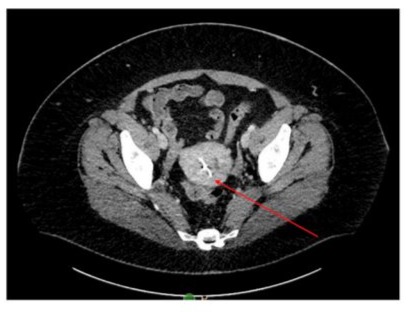
Figure 1: CT imaging showing the IUD within the uterine cavity (indicated by the red arrow).
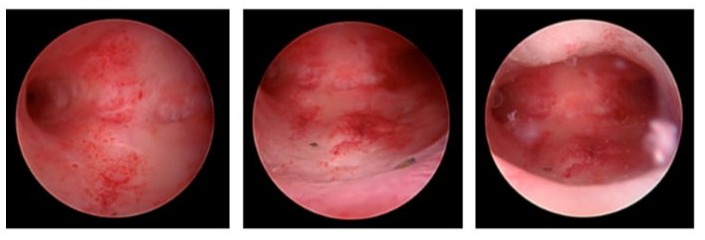
Figure 2: Hysteroscopic global survey showing inability to visualize the Mirena IUD.
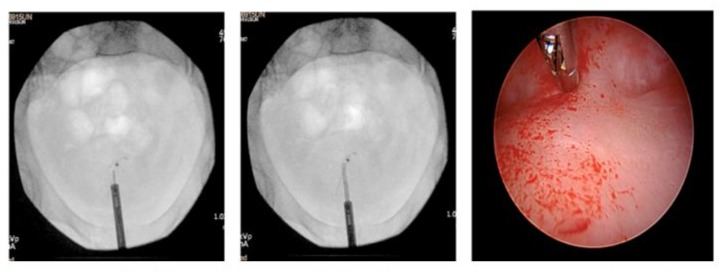
Figure 3: X-ray imaging guiding the initial dissection point of the MyoSure device along the posterior wall of the uterine cavity.
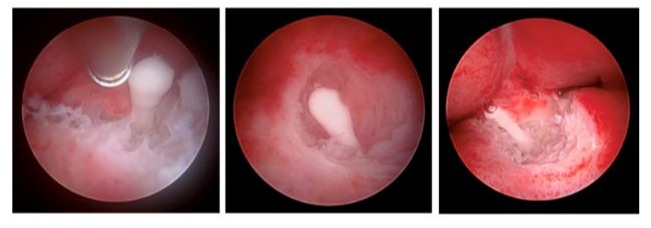 Figure 4: Hysteroscopic resection of the embedded IUD using the MyoSure device, following confirmation of its location with X-ray.
Figure 4: Hysteroscopic resection of the embedded IUD using the MyoSure device, following confirmation of its location with X-ray.
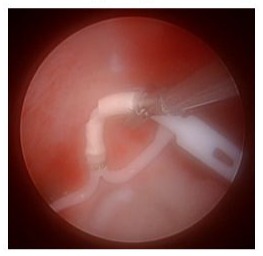
Figure 5: The entire Mirena IUD (without strings) following hysteroscopic endometrial dissection.
Discussion
Utilizing real-time intraoperative X-ray can facilitate a minimally invasive approach to the removal of a fully embedded IUD, particularly when the IUD strings are no longer visible. This case presentation highlights that preoperative imaging alone may not always provide sufficient information to determine the IUD location or the optimal surgical approach. Consequently, patients should be informed about the potential need for additional procedures, such as hysteroscopy or laparoscopy, for effective removal of a malpositioned IUD. If imaging had revealed that the IUD was subserosal or transmural with a significant distance from the endometrium, a laparoscopic or robotic approach would have been more appropriate for its removal.
It is crucial to perform endometrial dissection with caution, as excessive tissue removal can increase the risk of complications such as intrauterine scarring increasing risk for bleeding abnormalities, infertility, or ectopic pregnancy, uterine perforation, pregnancy complications (ie. placenta accreta spectrum), bleeding, and infection [3-5].
After the removal of a malpositioned IUD, it can be replaced immediately at the patient’s discretion [6]. However, in cases involving significant endomyometrial resection, it may be advisable to wait up to 2-3 menstrual cycles to allow for tissue regeneration [7]. A history of IUD malposition or expulsion is not a contraindication for subsequent IUD insertion [8]. The recurrence rate of malposition remains unknown and represents a potential area for future research.
Conclusion
In summary, three key surgical takeaways are essential when removing a fully embedded IUD:
- Preoperative Imaging Limitations: Preoperative imaging alone may not always provide sufficient information to determine the optimal surgical approach.
- Cautious Endometrial Dissection: Endometrial dissection should be performed with caution to minimize the risk of complications.
- Timing of IUD Replacement: Replacement of the
IUD can be done immediately at the patient’s discretion unless significant endomyometrial resection has occurred, in which case waiting may be advisable.
These takeaways emphasize the importance of a careful surgical approach and the use of real-time intraoperative X-ray to confirm the IUD’s precise location and ensure accurate dissection planes, contributing to a more successful IUD removal.
Conflict of Interest: There are no conflicts of interest.
References
- Kavanagh TA, Fletcher SA, & Shah MK. (2020). Intrauterine device expulsion and malposition: A comprehensive review of the literature. Contraception, 101: 244-251.
- Schiff, L. (2013). Intrauterine device transmigration into sigmoid bowel in early pregnancy: A case report. SLS Case Reports.
- Hurskainen R, Tei, L, & Duffy JMN. (2017). Risks and benefits of endometrial resection for abnormal uterine bleeding. International Journal of Gynecology & Obstetrics, 139: 63-69.
- Vervoort AJ, & Mol, BWJ. (2014). Complications of hysteroscopic surgery: What to expect and how to manage. Best Practice & Research Clinical Obstetrics & Gynaecology, 28:437-453.
- Schorge JO, & Williams T. M. (2012). Complications of hysteroscopic surgery: Uterine perforation and infection. Obstetrics & Gynecology, 120: 560-567.
- Baird DT, & Vostral SR. (2018). Immediate replacement of malpositioned intrauterine devices: Clinical guidelines and patient outcomes. Contraception, 97: 273-279.
- Goldstein SR, & Clark TL. (2017). Management of endometrial and myometrial damage: Recommendations for post-resection recovery and tissue regeneration. Journal of Minimally Invasive Gynecology, 24:763-768.
- American College of Obstetricians and Gynecologists. (2021). Long-acting reversible contraception: Implants and intrauterine devices. Committee Opinion No. 774. Obstetrics & Gynecology, 137: e128-e140.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.