Frontal Sinus Osteoma with Orbital Infection: A Case Report and Systematic Review of Cases
by Shek HT1, Nikie HY Sun1, SY Ho1, Stephanie NS Wong2*
1Department of Otorhinolaryngology, Queen Mary Hospital, Pok Fu Lam, Hong Kong SAR.
2Department of Surgery, Division of Otorhinolaryngology, The University of Hong Kong, Pok Fu Lam, Hong Kong SAR.
*Corresponding Author: Stephanie NS Wong, Department of Surgery, Division of Otorhinolaryngology, The University of Hong Kong, 3/F, Block T, Queen Mary Hospital, 102 Pok Fu Lam Road, Hong Kong.
Keywords: Frontal Sinus Osteoma; Osteoma; Sinonasal Tumour; Orbital Cellulitis; Orbital Abscess; Orbital Infection; Palpebral Abscess.
Received Date: 01 June 2025
Accepted Date: 05 June 2025
Published Date: 09 June 2025
Citation: Shek HT, Nikie HYS, Ho SY, Wong SNS (2025). Frontal Sinus Osteoma with Orbital Infection: A Case Report and Systematic Review of Cases. 10: 2314. https://doi.org/10.29011/2574-7754.102314
Abstract
Background: Frontal sinus osteomas can uncommonly invade the orbit and can be complicated with orbital infection. This article reports on a case of frontal sinus osteoma with orbital abscess and is the first systematic review of such cases. Methods: A detailed electronic search was performed on PubMed, EMBASE, and CINAHL Plus. The inclusion criteria were: adult (> 18 years old), frontal sinus involvement of osteomas, orbital cellulitis complicating osteomas. Results: A 67-year-old gentleman, with known left choroidal nevus and bilateral mild nuclear sclerotic cataract, was admitted for right eye swelling and blurring of vision for 2 days. On examination of the right eye, complete mechanical ptosis was noted. Visual acuity dropped from 0.7 to 0.025. Intraocular pressure was raised to 31 mmHg. Red desaturation was noted. Extraocular movement was limited by chemosis. A radiological diagnosis of frontal sinus osteoma with subperiosteal abscess (SPA) was made, and emergency frontal osteoma excision with combined approach and drainage of right orbital SPA were performed subsequently. Upon follow up, there was mild residual upper lid swelling, and no visual symptoms were noted. Three publications describing 3 patients met inclusion criteria and were included for systematic review. In cases with orbital infection, open or combined approaches are recommended in cases of lamina papyracea and orbital roof involvement. Conclusion: Subtotal resection of frontal osteomas with skull base involvement with open or combined approach should be considered in the setting of acute infection to avoid intracranial spread of infection.
Introduction
Paranasal sinus osteomas are benign osteogenic lesions in paranasal sinuses. They are the most common benign tumours of the nose and paranasal sinuses, and the frontal sinus is the most common location.[1] They are seen in 0.43% of plain sinus radiographs and 3% of sinus computed tomography (CT) scans[2]. They can happen at all ages, but are most commonly diagnosed at the third and fourth decades of life[3]. There is a slight male preponderance of paranasal sinus osteomas. This is attributed to a greater exposure to trauma and the larger size of their sinuses in males.[4] The aetiology of osteomas is still controversial. Despite the known association of multiple osteomas with Gardner syndrome [5], the exact cause of osteomas is still unknown.
Frontal sinus osteomas are usually asymptomatic and are discovered incidentally on radiographs. Tumours that are large or obstructive in nature can produce symptoms, such as chronic headache, chronic rhinosinusitis, mucocele, cosmetic deformity, cerebrospinal fluid (CSF) leak, and meningitis.[6] Frontal sinus osteomas are diagnosed radiologically. Typically, they present as hyperdense osseous lesions in the frontal sinus on CT scan and low-intensity changes on T2-weighted image on magnetic resonance imaging (MRI).[7]
Surgical approaches for frontal sinus osteomas include endoscopic and open approaches. Transnasal endoscopic surgery alone was the most common surgical approach adopted, followed by open osteoplastic flaps.[6,8] A grading system was devised by Chiu et al. to provide guidelines for surgical removal of frontal sinus osteomas.[9]
Frontal sinus osteomas can uncommonly invade the orbit and result in orbital infections. This article reports on a case of frontal sinus osteoma with orbital cellulitis and is the first systematic review of such cases. Patient demographics, tumour characteristics, surgical approach adopted, post-operative complications, and subsequent improvements in cases of frontal sinus osteomas with orbital infections would be discussed.
Methods
Search strategy
One independent reviewer (HT Shek) performed a detailed electronic search on PubMed, EMBASE, and CINAHL Plus for studies published between January 1970 and August 2024 without language restriction, and the findings were reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA). Key words and MeSH (Medical Subjective Headings) terms pertaining to the condition (i.e. osteoma, frontal osteoma, frontal sinus osteoma) were cross-referenced with terms pertinent to orbital infection (i.e. orbital cellulitis, orbital abscess, subperiosteal abscess, orbital infection, palpebral abscess) in relevant combinations. The full-text versions of all studies that the reviewers considered relevant were obtained. References of studies of potential relevance and relevant reviews were manually screened to identify any applicable study that was not previously identified. Case series and case reports were included for discussion.
Selection criteria
Case series and case reports on osteomas involving the frontal sinus with orbital infection were included. The inclusion criteria were: adult (> 18 years old), frontal sinus involvement of osteomas, orbital infection complicating osteomas. Conference abstracts and letters to editors were excluded if studies were not published as full reports. Non-English articles were included if they met the selection criteria with a translated English abstract. Any uncertainty was resolved by consensus with a second reviewer (Nikie HY Sun).
Data extraction
Data was extracted by one investigator (HT Shek). A system was developed to ensure accuracy by having each abstracted reference to be reviewed by another investigator (Nikie HY Sun). Any disagreement was solved by discussion and consensus. Information was gathered using data abstraction forms. Items extracted included title, first author, year of publication, patient demographics, tumour characteristics, surgical approach adopted, post-operative complications, and subsequent improvements, as mentioned above.
Results
Case Presentation
A 67-year-old gentleman was admitted for right eye swelling and blurring of vision for 2 days. On examination of the right eye, palpebral edema was noted. Visual acuity dropped from 0.7 to 0.025. Pupils were normal, both equal in size, accommodating and reactive to light, with no relative afferent pupillary defect. Extraocular movement (EOM) was limited by chemosis in all four directions. The right eye also failed the test plate in Ishihara test, with red desaturation noted. Intraocular pressure (IOP) was raised to 31 mmHg.
CT showed an osseous lesion occupying the right frontal sinus with extension into the superior aspect of the right orbit and erosion of the right orbital roof. A rim enhancing collection was also noted along the right superior medial orbital roof, which was consistent with subperiosteal abscess (SPA). A radiological diagnosis of frontal sinus osteoma with SPA was made (Figure 1). In view of the rapid drop in visual acuity, red desaturation, raised IOP, increasing proptosis and lid tightness, orbital compartment syndrome was suspected. Urgent right lateral canthotomy was performed by ophthalmologists. There was only slight improvement of symptoms after canthotomy.
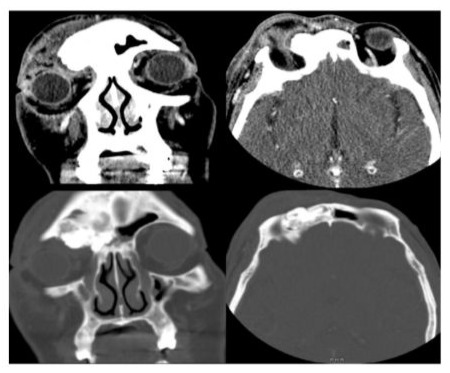
Figure 1: Axial and coronal CT scans showing frontal sinus osteoma with SPA
Emergency functional endoscopic sinus surgery with open resection of the orbital part of the osteoma, frontal sinusotomy, and drainage of right orbital SPA were performed by otorhinolaryngologists subsequently. An infrabrow incision was made and the above-and-below technique was adopted (Figure 2). 4 mL pus was drained, and the majority of the frontal sinus osteoma was removed. Part of the osteoma was intentionally left behind to avoid intracranial extension of the dissection and possible intracranial spread of the infection. Mometasone drug eluting stent and an endotracheal tube were placed over the frontal sinus drainage pathway. The operation was uneventful and there was no CSF leak intraoperatively.

Figure 2: Above-and-below technique with infrabrow incision
On postoperative day 3, optic nerve function was much improved. IOP was normal, EOM was full, and proptosis improved. Upon follow up, there was only mild residual upper lid swelling. Best corrected visual acuity of the right eye was 0.7 after 9 months, and no other visual symptoms were noted.
Systematic Review
Of 57 unique articles from the literature, three publications describing 3 patients were included in this review. The selection process follows the PRISMA reporting guidelines as summarised in (Figure 3) [11-13]

Figure 3: Selection flowchart
Including our reported patient, our series consisted of a total of 4 patients as detailed in (Table 1). Ages ranged from 42 to 67 years old (mean age: 53.5). 2 patients (patients 2 and 3) had frontal sinus osteomas extending to the ethmoid sinus; 2 patients (patients 3 and 4) had osteomas extending into the ipsilateral orbit. The surgical approaches adopted were either open (patients 2 and 3) or combined (open and endoscopic) (patients 1 and 4). There was one case of intraoperative CSF leak (patient 3) reported. This patient (patient 3) had an osteoma with intracranial extension. All 4 patients had uneventful recovery and resolution of symptoms.
|
Study (author/year) |
Age (year) |
Extension |
Surgical approach |
Complete removal? |
CSF leak |
|
|
1 |
Dispenza C et al., 2004 |
42 |
Part of contralateral frontal sinus |
Combined (frontal sinus trephination + endoscopic) |
No |
|
|
2 |
Sahin A et al., 2007 |
65 |
Ipsilateral ethmoid sinus |
Open |
Yes |
No |
|
3 |
Nguyen S et al., 2019 |
42 |
Ipsilateral orbital roof, contralateral frontal sinus, ethmoid sinus |
Open (osteoblastic flap) |
Yes |
Yes |
|
4 |
Our case report |
67 |
Ipsilateral orbit |
Combined (frontal sinus trephination + endoscopic) |
No |
No |
Table 1: Cases identified in the systematic review of published cases.
Discussion
Orbital infection is an uncommon complication of frontal sinus osteoma. It typically presents with erythema and edema of the eyelids, vision loss, fever, headache, proptosis, chemosis, and diplopia.[10] Generally, asymptomatic osteomas do not require treatment. Surgical treatment is recommended when the tumour occupies more than 50% of the frontal sinus.[14] However, when frontal sinus osteomas are complicated with orbital infection, treatment is essential.
There are three main surgical approaches for frontal sinus osteomas: open, endoscopic, and combined approaches. Open approaches, including Lynch frontoethmoidectomy, frontal sinus trephination, and osteoplastic flap, were classically preferred for laterally based osteomas. However, open approaches were associated with potential for poor cosmetic outcome due to the large incision, risk of osteoplastic flap fracture, and postoperative forehead deformity.[15] Endoscopic approaches have gained increasing popularity as an alternative to open approaches since the 1990s.[16] They can be classified into Draf IIA (removal of all ethmoidal cells obstructing frontal sinus drainage with resection of floor of frontal sinus between the lamina papyracea and the middle turbinate), Draf IIB (resection of the floor of frontal sinus from lamina papyracea and the nasal septum), and Draf III (resection of the frontal sinus floor on both sides, superior part of adjacent nasal septum and inferior area of interfrontal septum).[17] Combined (open and endoscopic) approach can also be adopted to achieve complete removal of osteoma with minimal morbidity. Combined approach can also ensure adequate resection of laterally based osteomas and ensure a precise frontal sinus drainage pathway endonasally.
Chiu et al.[9] devised a grading system in 2005 to provide guidelines on surgical removal. The three variables in the grading system are the location of the base of attachment, relative size to the frontal recess, and location in relation to a virtual sagittal plane through the lamina papyracea. They suggested that smaller Grade I-II osteomas that are medially located can be removed by endoscopic approaches, while laterally located Grade I-II osteomas, and larger Grade III-IV osteomas that occupy the majority of the frontal sinus should be removed using an open approach with an osteoplastic flap.
A more recent study by Ledderose GJ et al.[18] in 2011 showed that Grade III and IV osteomas can be removed by Draf III endoscopic approach, but with certain limitations, such as surgeon’s experience, narrow antero-posterior diameter of the frontal sinus, endoscopic equipment, anatomic variation, rather than absolute lateral extension past the lamina papyracea. Gotlib T et al.[19] also demonstrated the feasibility of removing Grade III and IV osteomas endoscopically. They suggested that an auxiliary external approach may be required when the frontal ostium is narrow, when tumours are extensively attached to the orbital roof, and when tumours grow close to the mid-orbital point.
Watley DC et al.[15] found that the attachment of the tumour to the orbital roof or floor of the frontal sinus is the most significant predictor of an open surgical approach. For frontal sinus osteomas with orbital infection, involvement of the lamina papyracea and orbital roof is common due to osteoma extension into the orbit. Such extension makes the removal of osteomas through endoscopic approach difficult. In our systematic review, none of the patients were operated by endoscopic approach only. Open or combined approaches were adopted in all cases with orbital infection.
There are still controversies regarding the extent of bone removal along the skull base. Currently, no guidelines are available to guide the extent of frontal sinus osteoma removal along the skull base. Iatrogenic CSF leak is a major complication in surgical removal of frontal sinus osteoma. Dural transgressions during sinonasal procedures commonly occur at the level of the cribriform plate and ethmoidal roof.[20] In our systematic review, the patient with CSF leak had intracranial extension of osteoma. Extensive removal of frontal sinus osteomas with intracranial extension could result in CSF leak. In addition to CSF leak, intracranial spread of infection could also occur in the setting of acute infection. In the literature, the reason for recurrence of osteomas had been described as non-removal of the osteoma tissue completely. However, the risk of spread of infection intracranially has to be taken into account especially when dealing with cases with acute infections.[21] In our reported case, part of the frontal osteoma was intentionally left behind to avoid intracranial extension of the dissection and possible intracranial spread of the infection. In frontal sinus osteomas with complicated orbital infection, extensive dissection of osteoma with intracranial extension could expose the dura and spread the infection to the central nervous system directly. To prevent spread of infection, subtotal resection of osteoma with re-establishment of frontal sinus drainage pathway should be considered especially during acute infective episodes. Further surgery with repair of skull base defect can be considered at a later stage when infection subsides and in the event of recurrence.
Limitations
Our study has several limitations. First, the retrospective nature of the study makes direct patient comparisons difficult. Since the cases were extracted from different publications, the documentation of cases was not uniform. Second, there was limited information regarding the characteristics of the tumours. Some publications did not provide information on the dimensions of the tumour, and very limited CT scans and image descriptions were provided in the publications. This makes the assessment of the tumour grading difficult.
Conclusions
In conclusion, frontal sinus osteomas can uncommonly invade the orbit and result in orbital infection. This is the first systematic review of frontal sinus osteoma cases with orbital infection. Open or combined approaches are recommended in cases of lamina papyracea and orbital roof involvement. Subtotal resection of osteoma should be considered in the setting of acute infection to avoid intracranial spread of infection. There is also a need to derive a guideline to guide the extent of frontal sinus osteoma removal along the skull base.
Acknowledgements: The authors sincerely thank the patient reported in the case report and his family.
Disclosures
Declarations of interest: None.
Ethical approval and consent: This study was approved by the Institutional Review Board (UW 25-230). Written informed consent was obtained from the patient.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Smith ME, Calcaterra TC. (1989). Frontal sinus osteoma. Ann Otol Rhinol Laryngol. 98: 896-900.
- Earwaker J. (1993). Paranasal sinus osteomas: a review of 46 cases. Skeletal Radiol. 22: 417-423.
- Atallah N, Jay MM. (1981). Osteomas of the paranasal sinuses. J Laryngol Otol. 95: 291-304.
- Mansour AM, Salti H, Uwaydat S, Dakroub R, Bashshour Z. (1999). Ethmoid sinus osteoma presenting as epiphora and orbital cellulitis: case report and literature review. Surv Ophthalmol. 43: 413-426.
- Koh KJ, Park HN, Kim KA. (2016). Gardner syndrome associated with multiple osteomas, intestinal polyposis, and epidermoid cysts. Imaging Sci Dent. 46: 267-272.
- Watley DC, Mong ER, Rana NA, Illing EA, Chaaban MR. (2019). Surgical Approach to Frontal Sinus Osteoma: A Systematic Review. Am J Rhinol Allergy. 33: 462-469.
- Watanabe N, Tsurubuchi T, Amano T, Sugii N, Sakamoto N, et al. (2022). Frontal sinus giant osteoma with radiologically unusual component suggesting blood supply: A case report. Radiol Case Rep. 18: 567-571.
- Arslan HH, Tasli H, Cebeci S, Gerek M. (2017). The Management of the Paranasal Sinus Osteomas. J Craniofac Surg. 28: 741-745.
- Chiu AG, Schipor I, Cohen NA, Kennedy DW, Palmer JN. (2005). Surgical decisions in the management of frontal sinus osteomas. Am J Rhinol. 19: 191-197.
- Tsirouki T, Dastiridou AI, Ibanez Flores N, Cerpa JC, Moschos MM, et al. (2018). Orbital cellulitis. Surv Ophthalmol. 63: 534-553.
- Dispenza C, Martines F, Dispenza F, Caramanna C, Saraniti C. (2004). Frontal sinus osteoma complicated by palpebral abscess: case report. Acta Otorhinolaryngol Ital. 24: 357-360.
- Sahin A, Yildirim N, Cingi E, Atasoy MA. (2007). Frontoethmoid sinus osteoma as a cause of subperiosteal orbital abscess. Adv Ther. 24: 571-574.
- Nguyen S, Nadeau S. (2019). Giant Frontal Sinus Osteomas: Demographic, Clinical Presentation, and Management of 10 Cases. Am J Rhinol Allergy. 33: 36-43.
- Smith ME, Calcaterra T.C. (1989). Frontal sinus osteoma. Ann Otol Rhinol Laryngol. 98: 896-900.
- Watley DC, Mong ER, Rana NA, Illing EA, Chaaban MR. (2019). Surgical Approach to Frontal Sinus Osteoma: A Systematic Review. Am J Rhinol Allergy. 33: 462-469.
- Rokade A, Sama A. (2012). Update on management of frontal sinus osteomas. Curr Opin Otolaryngol Head Neck Surg. 20: 40-44.
- Draf W. (2005). Endonasal frontal sinus drainage type I–III according to Draf. In: Kountakis S, Senior B, Draf W, editors. The frontal sinus. New York: Springer. pp. 219-231.
- Ledderose GJ, Betz CS, Stelter K, Leunig A. (2011). Surgical management of osteomas of the frontal recess and sinus: extending the limits of the endoscopic approach. Eur Arch Otorhinolaryngol. 268: 525-532.
- Gotlib T, Held-Ziółkowska M, Niemczyk K. (2014). Frontal sinus and recess osteomas: an endonasal endoscopic approach. B-ENT. 10: 141-147.
- Vinciguerra A, Dohin I, Daloiso A, Boaria F, Marc M, et al. (2024). Iatrogenic Cerebrospinal Fluid Leak in Endoscopic Sinus Surgery: Topographical Map and Influence of Skull Base Asymmetry. J Pers Med. 14: 226.
- Turan S, Kaya E, Pınarbaşlı MO, Çaklı H. (2015). The Analysis of Patients Operated for Frontal Sinus Osteomas. Turk Arch Otorhinolaryngol. 53: 144-149.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.