Femoral Approach for Total Hip Arthroplasty (THA) in High Dislocated Hips, Comparison of Two Surgical Techniques
by Stefan Cristea*, M. Gavrila, Fl. Groseanu
Department of Orthopaedic, UMF Carol Davilla, Emergency Hospital” St Pantelimon”, Bucuresti Romania
*Corresponding author: Stefan Cristea, Department of Orthopaedic, UMF Carol Davilla, Emergency Hospital” St Pantelimon”, Bucuresti, Romania
Received Date: 12 May 2025
Accepted Date: 19 May 2025
Published Date: 21 May 2025
Citation: Cristea S, Gavrila M, Groseanu F (2025) Femoral Approach for Total Hip Arthroplasty (THA) in High Dislocated Hips, Comparison of Two Surgical Techniques. J Surg 10: 11325 https://doi.org/10.29011/2575-9760.011325
Abstract
Introduction: We present only the difficult cases of THA in high dislocated hips. All present DDH classifications described the relations between the femoral head and acetabulum. In our experience the abnormalities of the femoral metaphysis and diaphysis play a major role in the treatment of DDH. Femoral canal is frequently distorted in severe cases of DDH. Starting from this idea, we have developed an original classification of femoral defects.
Materials and Methods: We have operated on 122 hips with DDH. First 61 cases were operated using a cemented femoral stem with trochanterotomy, femoral shortening osteotomy and trochanteroplasty Kerboull-Postel. The other 61 hips were operated with an uncemented femoral stem with femoral subtrochanteric triple osteotomy - shortening, correction of valgus and rotation.
Results: Our goal is to compare the preliminary results of two surgical techniques. The non-union of the greater trochanter in 5 cases (9%) has led us to adopt the technique of triple femoral osteotomy, using a non-cemented femoral component functioning as a centromedullary nail. The lengthening obtained varied from 3,5 to 8 cm, and we did not record any case of palsy, neither total nor partial, of the sciatic nerve. No septic complications or nonunion of femoral osteotomy occurred. We didn’t have any dislocations for all the cases in both series.
Discussion: For the preoperative planning we used the Ranawat criteria. Uncemented stems have the same function as a proximal locked nail. We appreciated the place of metaphyseal-diaphyseal osteotomy after reaming of the femoral canal to correct the rotation, shortening and valgus deviation up to 10 degrees. We increased the stability of the osteotomy using tension band wiring, but sometimes it is not necessary. We had one delayed union of the femoral osteotomy who necessitated percutaneous bone marrow injection, at 4 month, and union was obtained at 6 months postoperative. The type III cases, according to our classification or Eftekhar D, presented at the operation time with a limb length discrepancy between 2 and 8 cm. This discrepancy is due to the hip instability. The lengthening of those cases was easier compared to cases Eftekhar A and B with stable hips.
Conclusion: The femoral dysplastic vice is present in DDH. According to our opinion, in the dysplastic femur, there are two problems: the shaft channel, which is very narrow, and the vice of shaft torsion. The preoperative planning is mandatory. The femoral torsion with a severe helitorsion angle is a good indication for femoral triple osteotomy. The prosthetic replacement in cases of hips with congenital dysplasia is difficult in the high, unstable dislocations, but surgery offers the satisfaction of achieving a stable and mobile hip as well as an equal length of the limbs in patients of an average age of 42 years. The triple femoral osteotomy and uncemented femoral prostheses seem to be attractive, femoral complications have not yet been noticed.
Keywords: Classification; Congenital Hip Dysplasia (CDH); Developmental Dysplasia of the Hip (DDH); Treatment; Total Hip Arthroplasty (THA); Ultrasound
Introduction
Total Hip Arthroplasty (THA) is one of the most successful orthopedic procedures performed today for patients with pain due to a variety of conditions. A wide range of congenital and/or developmental hip disorders, such as neonatal instability, acetabular or femoral dysplasia, hip subluxation, and hip dislocation, are collectively referred to as developmental Dysplasia Of The Hip (DDH). Klisic changes the name of Congenital Hip Dysplasia (CDH) to DDH, emphasizing the role of time in triggering the condition [1]. Hippocrates proposed 2400 years ago that children’s hip dislocations are curable if treatment is started very early. Early detection of hip dislocation and dysplasia in newborns by ultrasound results in more efficient, straightforward, patientbearable, and cost-effective therapy [2]. In newborns, the reduced hip concentrically is simple to obtain, and a normal hip architecture is achieved. The issue occurs with cases of hip dislocation, dysplasia, or late detection. Treatment gets more aggressive, less successful, more painful, and more costly the later it is started. THA is required to return the adult hip’s normal biomechanics, lower limb equality, and hip stability. the appropriate location of the rotational center, the adjustment of the femoral offset, and the center of hip rotation. Applying a prosthesis for congenital hip dysplasia in adults usually doesn’t provide any unique challenges; however, it can get quite challenging in cases of high, unstable dislocations. We present only the severe cases: type IV Crowe, type C Hartofilakidis, or Eftekhar stages C and D.
All DDH classifications describe the relations between the femoral head and acetabulum. We present a few of them.
Crowe’s classification of hip dysplasias:
- Type I includes partial dysplasia of less than 50%;
- Type II partial dysplasia of 50-75% and acetabular deficit;
- Type III - partial dysplasia of 75-100%, but with the posterior and anterior columns intact;
- Type IV dysplasia exceeding 100%, with an underdeveloped original acetabulum and a deficient roof [3].
The Hartofilakidis classification of developmental dysplasia of the hip,
- Type A (dysplasia) hips had a deficiency of the superior segment of the acetabulum and a shallow acetabulum because of osteophyte coverage of the medial wall;
- Type B (low dislocation) hips had a deficiency of the anterior and posterior segments of the acetabulum, a narrow opening or small acetabular diameter, and shallow acetabular depth;
- Type C (high dislocation) hips had segmental deficiency of the entire acetabular rim, a narrow opening, shallow depth, and excessive anteversion [4,5].
Eftekhar established a radiologic classification in 1978 based on the femoral head’s grade of dislocation. Four phases of hip dysplasia severity were distinguished, ranging from partial dislocation to dysplasia.
- Type A is characterized by a slightly elongated and dysplastic acetabulum,
- Type B by an intermediate acetabulum,
- Type C by a false and high-sited acetabulum,
- Type D by the lack of any contact between the femur and the iliac bone [6].
The Kerboul classification on dislocation hip. Type A: anterior dislocation where the femoral head is located in front of the original acetabulum. Type B: intermediate dislocation. The femoral head articulates with the ilium at the same anterioposterior level as the original acetabulm. Type C: posterior dislocation [7].
Our Classification for Femoral Dysplasia in Adult Hip
All present DDH classifications described the relations between the femoral head and acetabulum. The current classifications focus more on the cotyl and the ratio between it and the femur than they do on the femur itself. In our experience, the abnormalities of the femoral metaphysis and diaphysis play a major role in the treatment of DDH. The femoral canal is frequently distorted in severe cases of DDH. They also frequently have femoral dysplasia. Starting from this idea, we have developed an original classification of femoral defects. In femoral dysplasia, there are two problems: the shaft’s torsion vice and its extremely tiny shaft canal. The torsion vice of the diaphysis is very manifest, especially in the transverse plane, but also in the coronal plane. The medullary canal is elliptic; the large metaphyseal medullary diameter becomes perpendicular to the broad diameter of the shaft channel, which makes it difficult to pose the femoral prosthesis. The vice of torsion and the narrow diaphysis induce longitudinal fractures of the femur. This complication is frequent because even the special prostheses are not adapted to the extreme difficulty of these cases.
We present our classification for the femoral dysplasia Figure 1.
Stage I - Mild torsion. The femoral canal is almost normal, and it could be associated with any type of Crowe, Kerboul, or Eftekhar stage A, B or C.
Stage II - Important torsion of the diaphysis and metaphysis. It could be associated with any type of Crowe, Kerboul, or Eftekhar C or D. It is a major indication for diaphyseal osteotomy or trochanterotomy during a THA.
Stage III - Severe torsion of the shaft, almost 900 to the condylar axis - a large medullary diameter of the metaphysis is perpendicular to the large diameter of the diaphysis canal. Excellent indication for triple femoral osteotomy.
Stage IV - Caricatural, a caricature of the proximal femur.
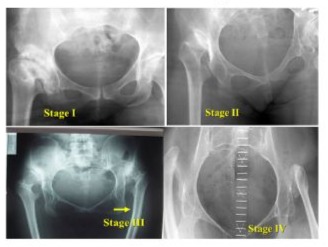
Figure 1: Femoral classification of DDH in adults.
During the THA, it is necessary to redo the hip architecture in severe dislocations. It is necessary to correct the center of rotation and the optimal femoral and cotyloid anteversion. It is necessary to establish an equality of length of the lower limbs. Correction of femoral offset reduces the risk of loss, decreases the forces applied to the cup, and decreases the wear of the polyethylene. So it is necessary to solve, for the hips in the high dislocations, two kinds of problems. On the one hand, there are cotyloid problems, and on the other hand, femoral problems.
Cotyloid Problems
The Ranawat criteria remain valid for the use of Ranawat’s rules for preoperative planning [8]. The Ranawat triangle - the horizontal line between the iliac ridges, the horizontal line between the ischiatic tuberosities, and the perpendicular to these lines, by 5 mm lateral of the Kohler and Shenton lines. On this perpendicular, the acetabular height (of the radiological “U”) is 1/5 of the height of the pelvis measured; the depth of the cotyl is equal to the height. The hypotenuse of the Ranawat triangle unites the ends of the cathetes, and the center of rotation is in the middle of the hypotenuse Figure 2.
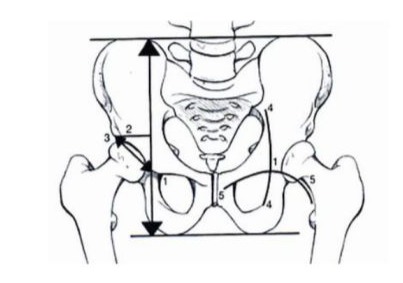
Figure 2: Ranawat’s rules for preoperative planning.
The Pierchon index for the correction of the femoral offset and the center of the hip rotation. For the dysplastic acetabulum, it is necessary to medialize and lower the center of rotation, and it is necessary to ensure good acetabular coverage [9].
Practical solutions are:
- Cotyloid reconstruction with a massive graft, structuralized and fixed by 2 screws, when more than 20% of the cup remains discovered superior or when small prostheses are difficult to put in. A Kerboull or Burch Schneider ring is often added to stabilize this cotyloid construction for cemented prostheses.
- medialization by cotyloidal controlled fracture - Hartofilakidis
- the use of a cotyl Espace / Megacups
- the placement on the neocotyl of the cup, not recommended.
Femoral problems
We find ourselves in two situations:
- Dysplastic hips already operated on by prior osteotomies (Schantz, Milch) or prior osteotomies and lengthening (Ilizarov, Palley) - it is necessary to reostotomize to redo the hip knee ankle axe (HKA). Osteotomies of shortening, derotation, and varization.
- surgical virgin hip in a high, unstable dislocation, with or without contact between the femur and the pelvis.
For this late situation - unstable hip, high dislocated, unoperated - we have 3 practical solutions:
- trochanteroplasty, trochanterotomy, proper great trochanter relocation and the use of a cemented or non-cemented prosthesis;
- femoral metaphyseal triple metaphyseal osteotomy of shortening, derotation, varization - the use of a noncimented prosthesis (Stage III of our classification);
- custom prosthesis - CAD CAM, which we don’t dispose of.
Methods
We selected all patients who could undergo THA surgery, with high dislocated hips and invited them to take part in the trial after receiving approval from the hospital’s institutional review board (approval number 2 from 3.02.2004). We include all patients who will undergo THA surgery between March 3, 2004, and March 3, 2021. 122 THAs who met our inclusion criteria and signed informed consent forms were among the 82 patients (62 females and 20 males), 40 of whom were bilateral (32 females and 8 males). The research was conducted in accordance with the Declaration of Helsinki. This study was carried out at the Saint Pantelimon Emergency Clinical Hospital, Orthopedics Clinic, with the agreement of the Hospital’s Ethics Committee and respecting the principles set out in the Helsinki Declaration. We present only the difficult cases of THA in high dislocated hips: type IV Crowe, type C Hartofilakidis, Eftekhar C or D and also our classification of femoral dysplasia, stages II and III (Figure 3).
This study compare the preliminary results between two surgical techniques.
- On the one hand, the prostheses putted in these cases by trochanterotomy, femoral osteotomy of shortening, implementation of a cemented prosthesis and trochanteroplasty - 61 cases.
- On the other hand, triple femoral osteotomy under trochanterian shortening correction of a preexistent valgum and derotation, and use of a non-cemented femoral prosthesis with or without osteosynthesis - 61 cases.
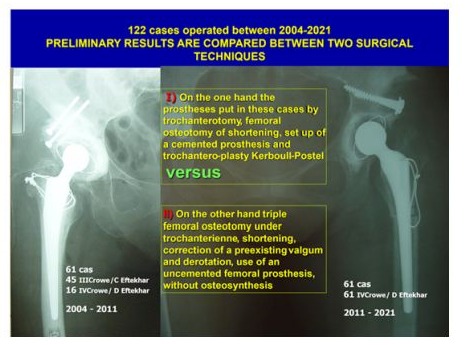
Figure 3: Compare study situation.
We operated on 61 hips between 2004 and 2011, including 16 type IV Crowe-D stage Eftekhar and 45 type III Crowe-C stage Eftekhar. Our classification placed 40 in stage 3 and 21 in stage 2.We evaluated clinically pre and postoperatively our patients according to the Merle d’Aubigné - Postel criteria (pain 0-6 points, mobility 0-6, gait 0-6 points).The preoperative inequality of the limbs varied from 3,5 to 5,5 cm and the postoperative shortening was at most 2 cm. The preoperative planning of the femoral osteotomy was adjusted recording to the desired lengthening. We have systematically performed a trochanteroplasty. In the severe high sited dysplasias we have at first carried out a subtrochanteric femoral osteotomy at the level of the upper projection of the original acetabulum. We detached from this proximal fragment the greater trochanter, and we modelled it concavely to attach it to the subtrochanteric femoral diaphysis.The duration of the operation varied from 180 to 330 minutes.The trochanteroplasty on the subtrochanteric cortical surface was not always easy, owing to the torsion vice. We applied the Kerboul - Postel technique. In 6 cases we detected the non-union of the greater trochanter, but it remains functional in two cases. The revision of trochanteroplasty was necessary in 4 other cases. In 1 case, the thread of the trochanteroplasty caused a bursitis and a subcutaneous necrosis, which was the starting point of an infection. This required, after a year, the septic revision with Kent prosthesis.The high rate of nonunion of the greater trochanter (19%) determined us after 2011 to adopt the second technique in those cases - the triple femoral osteotomy and uncemented prosthesis. We adopted the technique of triple femoral osteotomy under trochanterian shortening correction of a preexistent valgum and derotation and use of a non-cemented femoral prosthesis with or without osteosynthesis. We operated on 61 hips, type IV Crowe-stage D Eftekhar, stage III of our classification, between 2011 and 2021. In 1988, P.D. Sponseller and A.A. McBeath initially described the subtrochanteric osteotomy technique, which is utilized in patients with high hip dislocation and developmental abnormalities of the hip. The technique was developed with the idea of intramedullary fixation of the osteotomy line with an uncemented stem [10,11]. Rigorous planning is necessary.
On high dislocated hips plain Xray, the place of the projection of the lower part of the original acetabulum on the femur is marked as the future place of the femoral osteotomy. The distance from the tip of the greater trochanter to this point is measured. If the axis of the femur is not perturbed, the preparation of the femur with reamers is done. Otherwise, the femoral osteotomy is performed first. In this place a marker of the femoral axis is performed for the eventual rotational osteotomy. The proximal part of the femur is reclined, and the acetabular preparation is performed. The cut of the femoral neck and the proximal preparation of the femur with reamers and probe stem prosthesis. Also, the preparation of the distal part of the femur is necessary. The necessity of shortening osteotomy is evaluated by mesuring the equality of the lower limbs, and also the necessity of the shortening osteotomy. A step-cut osteotomy at this point will be performed. The Z osteotomy assures the stability and facilitates the consolidation of the femur. After the ductal bore, we appreciate the place of the submetaphyseal osteotomy, correction of the rotation, shortening, and correction of a preexisting genu valgum - up to 100. Fig 4 The femoral non-cemented prostheses work like locking nails. A metal wire could improve the stability like a hobana. For this lot, the elongation obtained varied between 4.5 and 8 cm without any case of paralysis of sciatica. We did not do traction preoperatively. We did not have any cases of prosthesis lust in these 2 series. The use of this technique prevents the lack of supply.
Results
In this study, we present only the severe cases: type III - IV Crowe, type C Hartofilakidis, Eftekhar stage C and D, and type 2 and 3 of our classification. Forty-five hips were classified as type III, C Eftekhar, and seventy-seven hips were classified as type D Eftekhar, IV Crowe. Our classification showed that 101 were stage III and 21 were stage II. For the acetabulum, the technique remains the same, we use cemented prostheses. We resorted to the reconstruction of the cotyl with a massive graft, structuralized fixed by 2 screws. When we have not had prostheses with a small cup and when more than 20% of the cup remains uncovered. The mean age of the patients was 42 years (26-76 years). All patients have a minimum follow-up of 3 years. These cases belong to stage 3 of our classification. Forty-five hips were classified as type III Crowe, C Eftekhar, and seventy-seven hips were classified as type D Eftekhar, type C Hartofilakidis, IV Crowe. According to our classification, 82 were in stage III and 21 were in stage II. Preoperatively, the Merle D’Aubigne-Postel score of these 122 hips was 4. Postoperative results were very good in 41 hips (67,21%) of the first lot of operations and in 44 hips of the second lot of operations (72,13%), good in 17 hips of each lot (27,86%). Modest results were obtained in 3 hips on the first lot (4,91%) due to the non-union cases who necessitate the revision of the greater trochanter. The elongation obtained varied between 4,5 and 8 cm without any case of paralysis of sciatica. We did not do traction preoperatively. We did not have any cases of prosthesis lust in these 2 series. The use of this technique prevents the lack of supply.A delay in consolidation, of the femoral osteotomy on the second lot, required a percutaneous injection of the medullary juice at 4 months, and consolidation was achieved at 6 months (Figure 4).

Figure 4: Bilateral case of high dislocated hips, THA on high dislocated hips by triple femoral osteotomy, percutaneous injection of medullary juice help the delay of consolidation at 6 months.
In the first lot, 4 cases with secondary genu valgum and torsion vice of the femur necessitated a femoral correction by shortened osteotomy above the knee at a time interval varying between 6 weeks and 3 months after the hip prosthesis. The opening osteotomy permitted us to gain an additional 1 - 2 cm. In the first lot, a postoperative palsy of the femoral nerve occurred in 3 cases, but disappeared spontaneously, without neurolysis. On the second lot, the lengthening obtained varied from 4,5 to 8 cm; and we did not record any case of palsy, neither total nor partial, of the sciatic nerve. No preoperative traction was necessary. In 5 cases, a shortening of less than 2 cm persisted. No prosthesis dislocation occurred. In 20 of these 122 hips (5 on the first lot and 15 on the second lot), the dysplasias were bilateral, and we operated first on the less severely affected side; afterwards we equalised the limbs by replacement of the high-dislocated hip, after which we carried out on the same side the osteotomy of the knee.
Discussion
Considered the “operation of the century”, Total Hip Arthroplasty (THA) is one of the most successful orthopaedic surgeries carried out today. Hip arthritis is caused by a variety of architectural abnormalities that could be congenital. A wide range of congenital and/or developmental hip disorders, such as neonatal instability, acetabular or femoral dysplasia, hip subluxation, and hip dislocation, are collectively referred to as developmental dysplasia of the hip (DDH). A study of genetic and other etiological factors was conducted in 1970 by Ruth Wynne-Davies in 589 index patients with congenital hip dislocation and their families. Acetabular dysplasia, familial joint laxity, and a comparison of neonatal and late-diagnosis cases were specifically investigated [10]. Later on, Klisic changes the name of Congenital Hip Dysplasia (CDH) to DDH, emphasising the role of time in triggering the condition [1]. Hippocrates proposed 2400 years ago that children’s hip dislocations are curable if treatment is started very early. Early detection of hip dislocation and dysplasia in newborns by ultrasound results in more efficient, straightforward, patient-bearable, and costeffective therapy [2]. In newborns, the reduced hip concentrically is simple to be obtained, and a normal hip architecture is achieved. The issue occurs with cases of hip dislocation, dysplasia, or late detection. Treatment gets more aggressive, less successful, more painful, and more costly the later it is started. THA is required to return the adult hip’s normal biomechanics, lower limb equality, and hip stability. the appropriate location of the rotational center, the adjustment of the femoral offset, and the center of hip rotation.
Applying prosthesis for congenital hip dysplasia in adults usually doesn’t provide any unique challenges; however, it can get quite challenging in cases of high, unstable dislocations. All present DDH classifications described the relations between the femoral head and acetabulum. The current classifications focus more on the cotyl and the ratio between it and the femur than they do on the femur itself. In our experience the abnormalities of the femoral metaphysis and diaphysis play a major role in the treatment of DDH. Femoral canal is frequently distorted in severe cases of DDH. They also frequently have femoral dysplasia. Starting from this idea, we have developed an original classification of femoral defects. In the femoral dysplasia, there are two problems: the shaft’s torsion vice and its extremely tiny shaft canal. In this study, we present only the severe cases: type IV Crowe, type C Hartofilakidis, Eftekhar stage C and D, and types 2 and 3 of our classification. Forty-five hips were classified as type III, C Eftekhar, and seventy-seven hips were classified as type D Eftekhar, IV Crowe. Our classification showed that 101 were stage III and 21 were stage II. Stage III of our classification, or Eftekhar D, has an inequality between 2 and 8 cm. In these cases the inequality is increased by the instability of the hip. The lengthening of these cases was obtained easier than in the Eftekhar A or B cases - more stable hips, or soft tissues remain more adherent. The piston sign explains that. A non-cemented stem prosthesis featuring a metaphyseal osteointegrated zone has been employed. The stem’s distal portion is smooth. Those stems function similarly to a locking nail.
This method, femoral osteotomy, was used to operate on all 61 hips. Luckily, we avoided using the straight-stem Zweimuller in these situations [12].
Conclusions
Early detection of hip dislocation and dysplasia in newborns by ultrasound results in more efficient, straightforward, patientbearable, and cost-effective therapy. In new born, the reduced hip concentrically is simple to obtain, and a normal hip architecture is achieved. The issue occurs with cases of hip dislocation, dysplasia, or late detection. Treatment gets more aggressive, less successful, more painful, and more costly the later it is started.
In adults, applying a prosthesis for congenital hip dysplasia usually doesn’t provide any unique challenges; however, it can get quite challenging in cases of high, unstable dislocations. The femoral dysplastic vice is present in DDH. According to our opinion, in the dysplastic femur, there are two problems: the shaft channel, which is very narrow, and the vice of shaft torsion. The preoperative planning is mandatory. The femoral torsion with a severe helitorsion angle is a good indication for femoral triple osteotomy. Femoral torsion defects, especially metaphyseal - can be solved by three solutions: special CAD-CAM prostheses, trochanterotomytrochanteroplasty or triple femoral metaphyseal osteotomy.These defects can be corrected by prostheses, if they are well evaluated preoperatively. Femoral torsion defects with a severe heliotorsion angle are a good indication for femoral triple osteotomy. The prosthetic replacement in cases of hips with congenital dysplasia is difficult in the high, unstable dislocations, but surgery offers the satisfaction of achieving a stable and mobile hip as well as an equal length of the limbs in patients of an average age of 42 years. The triple femoral osteotomy and uncemented femoral prostheses seem to be attractive; femoral complications have not happened so far.
Future Directions
Prevention and early detection by ultrasound in newborns of DDH is efficient. straightforward, patient-bearable, and cost-effective therapy.
Early detection of neglected hip dislocation and dysplasia could prevent arthritic sequelae.
Health programs could be implemented to prevent degenerative changes and arthritis secondary to DDH.
New implants will be developed to resolve better THA in DDH.
References
- Klisic P (1989) congenital dislocation of hip a misleading term J.Bone joint surgery 71: 136.
- Graf R (1984) Fundamentals of Sonographic Diagnosis of Infant Hip Dysplasia. Journal of Pediatric Orthopaedics 4: 735-740.
- Crowe JF, Mani VJ, Ranawat CS (1979) Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 61: 15-23.
- Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N (1996) Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am 78: 683-692.
- Hartofilakidis G, Stamos K, Ioannidis TT (1988) Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br 70:182-186.
- Eftekhar N (1978) Principles of total hip arthroplasty. C V Mosby, St. Louis 1978: 437-455.
- Kerboul M, Mathieu M, Sauzieres P (1987) Total hip replacement for congenital dislocation of the hip. In: Postel M, Kerboul M, Evrard J, Courpied JP (eds) Total hip replacement. Springer, Berlin Heidelberg New York 1987: 51-66.
- Ranawat CS, Dorr LD, Inglis AE (1980) Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis. J Bone Joint Surg 62-A : 1059-1065.
- Pierchon F, Migaud H, Duquennoy A, Fontaine C (1993) [Radiologic evaluation of the rotation center of the hip] (in French). Rev Chir Orthop Reparatrice Appar Mot 79 : 281-284.
- Wynne-Davies R (1970) Acetabular dysplasia and familial joint laxity: two etiological factors in congenital dislocation of the hip - A Review of 589 Patients and Their Families JBJS 52-B: 704 -716.
- Sponseller PD, McBeath AA (1988) Subtrochanteric osteotomy with intramedullary fixation for arthroplasty of the dysplastic hip. A case report. The Journal of Arthroplasty 3: 351-354.
- Perka C, Fischer U, Taylor WR, Matziolis G (2004) Developmental hip dysplasia treated with total hip arthroplasty with a straight stem and a threaded cup. J Bone Joint Surg Am 86: 312-319.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.