Extra-Pelvic Endometriosis: A Pictorial Essay
by Caroline Chabot1*, Bruno Vande Berg2
1Department of Radiology, Cliniques Universitaires Saint-Luc, Université Catholique de Louvain, Brussels, Belgium
2Department of Radiology, Clinique CHC MontLégia, Liège, Belgium
*Corresponding author: Dr. Caroline Chabot, Department of Radiology, Cliniques Universitaires Saint Luc, Université Catholique de Louvain, Avenue Hippocrate, 10 ; B-1200 Brussels, Belgium
Received Date: 08 February 2026
Accepted Date: 12 February 2026
Published Date: 16 February 2026
Citation: Chabot C, Vande Berg B. (2026). Extra-Pelvic Endometriosis: A Pictorial Essay. Ann Case Report. 11: 2531. DOI: https://doi.org/10.29011/2574-7754.102531
Abstract
Extra-pelvic endometriosis is an uncommon manifestation that may involve the abdominal wall, skeletal muscles, or peripheral nerves, presenting with painful masses or neuropathic symptoms. Magnetic resonance imaging (MRI) plays a pivotal role in lesion detection by enabling detailed assessment of tissue composition, localization, and extent, as well as evaluation of associated pelvic disease.
This pictorial essay illustrates the spectrum of MRI appearances of extra-pelvic endometriosis and emphasizes imaging features that facilitate accurate diagnosis and guide optimal patient management.
Keywords: Abdominal wall; Extra-pelvic endometriosis; MRI; Ultrasound
Introduction
Endometriosis is defined by the presence of endometrial glands and stroma outside the uterine cavity and affects approximately 5-10% of women of reproductive age. [1] Although pelvic involvement is most common, extra-pelvic manifestations can occur in the abdominal wall, skeletal muscles, peripheral nerves, or even distant sites such as the lungs and diaphragm. These atypical presentations often pose diagnostic challenges, as symptoms may not follow a cyclical pattern and may mimic other benign or malignant conditions.
Patients with extra-pelvic endometriosis may present with a painful mass, focal discomfort, or unusual neuropathic symptoms. Imaging is therefore critical for lesion identification and differentiation from desmoid tumors, granulomas, hernias, or soft tissue malignancies. [2,3] Among imaging modalities, MRI offers superior tissue characterization, enabling precise mapping of lesion composition, extent, and relation to adjacent structures, which is particularly valuable for surgical planning.
Abdominal Wall Endometriosis
Abdominal wall endometriosis is the most frequent form of extrapelvic endometriosis and is predominantly associated with prior surgical scars, most commonly following cesarean sections or laparotomies, with a reported incidence ranging from 0.03% to 1%. [2,4] The prevailing mechanism is iatrogenic implantation of endometrial cells during surgery. Nevertheless, up to 20% of cases occur in patients without prior abdominal surgery, often located in inguinal or periumbilical regions, suggesting alternative routes such as lymphatic or hematogenous dissemination. [1]
Clinical symptoms typically appear several years after surgery, with a mean delay of 3-4 years. Pain is present in the majority of patients and is cyclic in roughly half of cases. [2,5] Associated pelvic endometriosis has been reported in 13-46% of patients [4,5].
Ultrasound is often the first-line imaging modality but remains nonspecific. Lesions usually appear as ill-defined hypo- to isoechoic masses with variable vascularity on color Doppler imaging. Cystic components may be present, and lesion appearance can fluctuate throughout the menstrual cycle. Fine-needle aspiration often yields insufficient or non-diagnostic material due to the fibrotic content of the lesions. Core biopsy may be considered, but puncture tracts should be excised during subsequent surgery to prevent recurrence [3].
MRI is the reference standard for evaluating abdominal wall and intramuscular endometriosis. Imaging features vary according to lesion composition. Predominantly fibrous lesions exhibit low to intermediate signal intensity on T2-weighted images, often with ill-defined margins and infiltrative growth patterns (Figure 1). Intramuscular cystic lesions may be well-circumscribed, occasionally resembling ectopic ovarian endometriomas (Figure 2). Infiltrative intramuscular lesions with hemorrhagic microcysts present as punctate or confluent hyperintense foci on fatsuppressed T1-weighted images (Figure 3). Overall, lesions can be iso- to hyperintense relative to muscle on T2-weighted images, with focal T1 hyperintensity reflecting hemorrhagic components, a feature highly suggestive of endometriosis. [3,5] After gadolinium administration, lesions usually demonstrate moderate to marked, often heterogeneous, enhancement. Lesions may appear nodular, spiculated, or retractile and can infiltrate adjacent muscular layers, including the rectus abdominis or oblique muscles. Diffusionweighted imaging often demonstrates intermediate diffusion restriction, with reported apparent diffusion coefficient (ADC) values around 0.93 × 10⁻³ mm²/s. [5] MRI also permits accurate delineation of lesion extent through the abdominal wall layers and facilitates detection of concurrent pelvic disease, which is essential for comprehensive surgical planning [3,5].
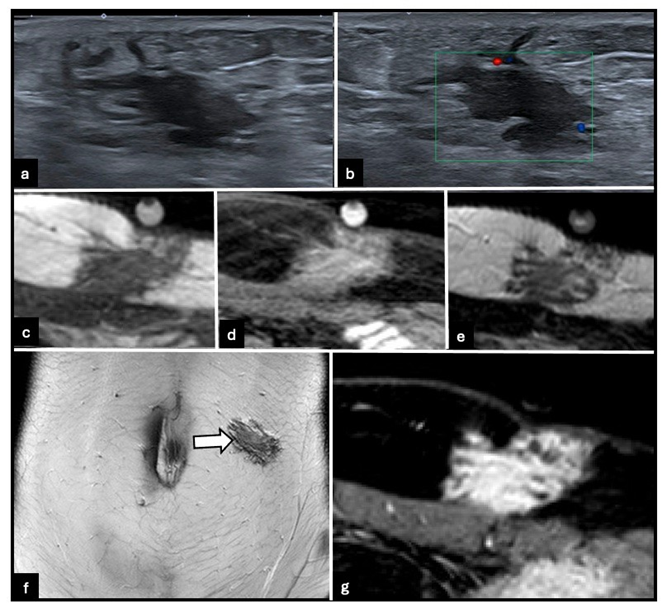
Figure 1: 33-year-old woman with predominantly fibrous hypodermic abdominal wall endometriosis on the left side. (a) B-mode ultrasound image shows an ill-defined hypodermic lesion of the left abdominal wall. (b) Color Doppler ultrasound image shows minimal vascularity. (c) Axial T1-weighted MRI image demonstrates low signal intensity. (d) Axial fat-suppressed T1-weighted MRI image shows foci of hyperintensity. (e) Axial and (f) coronal T2-weighted MRI images demonstrate low to intermediate signal intensity (arrow), consistent with a predominantly fibrous infiltrative lesion. (g) Axial contrast-enhanced 3D T1-weighted GRE MRI image shows moderate heterogeneous enhancement.
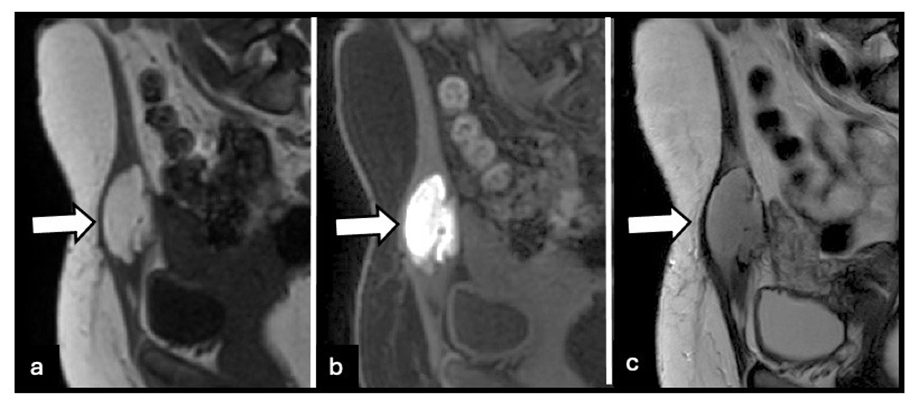
Figure 2: 25-year-old woman with intramuscular cystic abdominal wall endometriosis involving the left rectus abdominis muscle. (a) Sagittal T1-weighted MRI image shows a well-circumscribed predominantly cystic lesion with high signal intensity (arrow). (b) Fatsuppressed T1-weighted MRI image demonstrates marked hyperintensity, consistent with hemorrhagic content (arrow). (c) Sagittal T2weighted MRI image shows heterogeneous signal intensity with a well-defined fluid component (arrow), resembling an ectopic ovarian endometrioma.
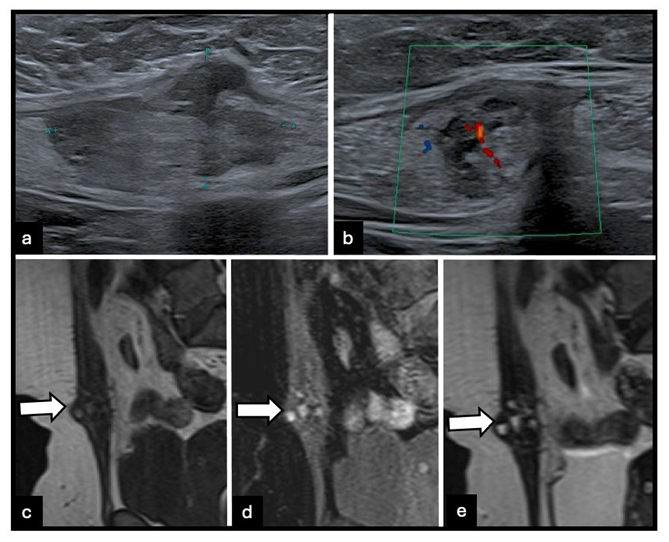
Figure 3: 51-year-old woman with infiltrative intramuscular abdominal wall endometriosis involving the right rectus abdominis muscle. (a) B-mode ultrasound image shows a parietal intramuscular lesion. (b) Color Doppler ultrasound image demonstrates mild hyperemia. (c) Sagittal T1-weighted MRI image shows slight hyperintensity (arrow). (d) Fat-suppressed T1-weighted MRI image demonstrates punctate and confluent foci of marked hyperintensity, reflecting hemorrhagic microcysts (arrow). (e) Sagittal T2-weighted MRI image shows iso- to moderately hyperintense signal relative to muscle (arrow), consistent with infiltrative endometriosis.
Nerve Endometriosis
Endometriotic involvement of peripheral nerves is rare but can lead to severe neuropathic pain, which may be cyclic or continuous. Frequently affected nerves include the sciatic nerve, lumbosacral plexus, genitofemoral nerve, ilioinguinal nerve, iliohypogastric nerve, and branches of the abdominal wall nerves. Pathophysiology typically involves perineural or endoneural infiltration, sometimes tracking along the round ligament [1].
Two main MRI phenotypes are recognized. Fibrous infiltrative lesions appear hypointense on both T1- and T2-weighted sequences and are often associated with deep endometriosis (Figure 4), whereas cystic or hemorrhagic lesions demonstrate hyperintensity on T1- and T2-weighted sequences. Advanced MRI sequences, such as high-resolution 3D T2 and diffusion tensor imaging (DTI), enhance lesion detection and allow visualization of the relationship between endometriotic tissue and nerve fascicles. Accurate imaging is crucial, as nerve-sparing surgery or targeted medical therapy may be required to prevent irreversible neurological deficits [6].
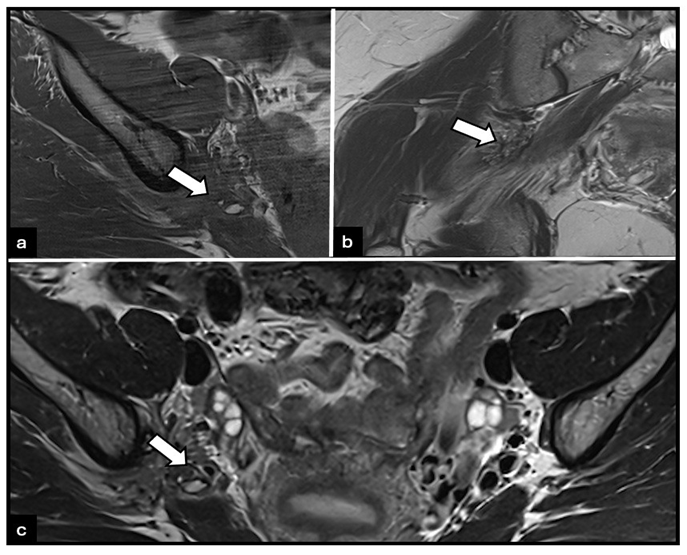
Figure 4: Woman with fibrous infiltrative right sciatic nerve endometriosis. (a) T1-weighted MRI image shows a low-signal-intensity focus along the right sciatic nerve (arrow), consistent with perineural fibrous infiltration. (b) Coronal and (c) axial T2-weighted MRI images demonstrate hypointense infiltrative tissue along the right sciatic nerve (arrows), characteristic of deep endometriosis. No abnormality is observed on the left side.
Conclusion
Extra-pelvic endometriosis, though uncommon, should be considered in women of reproductive age presenting with painful abdominal wall masses, groin pain, or atypical neuropathic symptoms. MRI provides comprehensive assessment of lesion composition, location, and extent, and enables detection of associated pelvic disease. Recognition of characteristic imaging patterns facilitates accurate diagnosis, reduces misdiagnosis, and guides appropriate management strategies, including surgical planning and medical therapy. Early identification and precise mapping of lesions can significantly improve patient outcomes and quality of life.
Funding: None.
Acknowledgment: None.
References
- Hirata T, Koga K, Osuga Y. (2020). Extra-pelvic endometriosis: a review. Reprod Med Biol. 19: 323-333.
- Hensen JH, Van Breda Vriesman AC, Puylaert JB. (2006). Abdominal wall endometriosis: clinical presentation and imaging features with emphasis on sonography. Am J Roentgenol. 186: 616-620.
- Gidwaney R, Badler RL, Yam BL, Hines JJ, Alexeeva V, et al. (2012). Endometriosis of abdominal and pelvic wall scars: multimodality imaging findings, pathologic correlation, and radiologic mimics. Radiographics. 32: 2031-2043.
- Carsote M, Terzea DC, Valea A, Gheorghisan-Galateanu AA. (2020). Abdominal wall endometriosis (a narrative review). Int J Med Sci. 17: 536-542.
- Busard MP, Mijatovic V, van Kuijk C, Hompes PG, van Waesberghe JH. (2010). Appearance of abdominal wall endometriosis on MR imaging. Eur Radiol. 20: 1267-1276.
- Colak C, Chamie LP, Youngner J, Forney MC, Luna Russo MA, Gubbels A, et al. (2024). MRI features of pelvic nerve involvement in endometriosis. Radiographics. 44: e230106.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.