Evaluation of Clinical, Systemic and Surgical Factors in the Anatomical and Functional Outcomes of Surgery for Complete Macular Hole
by Ali Tonuzi1*, Orjeta Tonuzi2, Migena Beqiri
1Associate Professor, Mother Theresa University Hospital Center, Faculty of Medicine, Tirana, Albania
2Mother Theresa University Hospital Center, Tirana, Albania
*Corresponding author: Ali Tonuzi, Associate Professor, Mother Theresa University Hospital Center, Faculty of Medicine, Tirana, Albania.
Received Date: 11 June, 2025
Accepted Date: 18 June, 2025
Published Date: 22 June, 2025
Citation: Tonuzi A, Tonuzi O, Beqiri M (2025) Evaluation of Clinical, Systemic and Surgical Factors in the Anatomical and Functional Outcomes of Surgery for Complete Macular Hole. Ophthalmol Res Rep 09: 10168. https://doi.org/10.29011/2475-5605.110168
Abstract
A Full-Thickness Macular Hole (FTMH) is a small break in the macula, the central part of the retina responsible for sharp detailed vision. The primary treatment for this condition is Pars Plana Vitrectomy (PPV), a type of eye surgery aimed at closing the hole and restoring vision. This complete retinal thickness defect in the fovea leads to significant loss of central vision. Its etiology can be idiopathic, myopic, traumatic or secondary to other retinal diseases. Pathophysiological mechanisms include anteroposterior and tangential traction forces at the vitreoretinal interface as well as degenerative changes in the foveal structure.
The study of this phenomenon approaches the evaluation of the impacts of demographic, systemic, and surgical factors, as well as the anatomical and functional outcomes of patients diagnosed and operated on with these anatomical defects of the complete macular hole.
In our study for the period 2018–2023, about 26 patients diagnosed and operated with Pars Plana Vitrectomy, Internal Limiting Membrane (ILM) skin, were tamponade with C3F8 (octafluoropropane-a perfluorocarbon gas), in the context of macular hole treatment, which is used as a long-acting intraocular gas. Surgical repair typically involves a Pars Plana Vitrectomy, where the vitreous gel is removed. After the vitreous is removed, a gas bubble like C₃F₈ is injected into the eye to act as a tamponade (internal bandage). This gas bubble helps: 1] flatten the macula; 2] keep the edges of the hole in contact, and 3] promote healing and closure of the hole.
Demographic factors, presence of comorbidities like: Impact of Hypertension (IHTN) and Diabetes Mellitus (DM) on macular hole surgery have a role for using of tamponade procedure, and changes in Best Corrected Visual Acuity (BCVA) after macular hole surgery were analyzed.
The study showed that the most represented group was the age group of 61-69 years. The most used tamponade was C3F8 in 76.9% of cases, while approximately 23.1% received silicone. The parameters of age, IHTN, diabetes, as well as the length and depth of the hole did not have a significant impact on functional improvement.
Tamponade with C3F8 remains the most effective option for visual improvement after surgical intervention for full thickness macular hole. The use of silicone, although useful for anatomical purposes, shows more limited functional benefit. Systemic parameters and anatomical dimensions of the hole did not significantly affect this limited sample.
Further studies with larger samples (patients) are recommended to further confirm this approbation.
Keywords: Macular hole; Pars plana vitrectomy; Silicone oil; Tamponade; Retinopathy.
Introduction
A full-thickness macular hole is anatomical defect of the thickness of the retina fovea, with interruption of all neural retinal layers from the internal limiting membrane to the retinal pigment epithelium, which could result in central visual loss and visual distortion of the central eyesight. Its etiology can be idiopathic, myopic, traumatic or secondary to other retinal diseases. Pathophysiological mechanisms include anteroposterior and tangential traction forces at the vitreoretinal interface as well as degenerative changes in the foveal structure [1,2].
The authors Kelly and Wendell [2,3] reported in 1991 the first successful closure of a series of full-thickness macular holes by pars plana vitrectomy and membrane peeling. Since that time the pars plana vitrectomy has become the standard treatment for full thickness macular holes, and over 95% of this phenomena close after surgery.
Common symptoms at presentation include metamorphopsia and visual deprivation, primarily due to the involvement of the central fovea. However, these symptoms can be ameliorated through successful surgical closure [4,5]. The potential contribution of anteroposterior vitreous traction forces in the development of macular hole has long been a subject of inquiry. Functional improvement, measured by best-corrected visual acuity, depends on various factors: the size and duration of the hole, the presence of high myopia, the timing of the surgical intervention, and the techniques used [5].
New surgical techniques, such as the inverted internal limiting membrana flap or autologous retinal transplantation, have been developed to treat large macular holes, with increasingly better results in anatomical closure and visual improvement [6,7]. In 2010, a novel technique was introduced by Michalowski involving the use of an internal limiting membrana flap to cover large idiopathic macular holes [8]. In this method, the internal limiting membrana is not entirely removed but is instead left attached to the edges of the macular hole and inverted to cover it. This approach significantly increased the success rate for the closure of larger macular holes to approximately 98%.
Furthermore, modern classifications such as the CLOSE group (help in selecting optimal surgical strategies, based on the size, shape, and characteristics Classification of Large macular holes by Stage and Extent) of the foveal defect [9]. These advances emphasize the importance of a personalized approach to the surgical management of macular holes, taking into account individual patient factors and the specific anatomical context.
Contemporary technological improvements in Optical Coherence Tomography (OCT) have yielded higher resolution images and enabled more precise visualization of the microarchitecture of the vitreoretinal interface, which can facilitate the studies on pathologic features that were not previously visible [10,11].
Adhere the demographic factors, as well as the presence of comorbidities like: Impact of Hypertension (IHTN) and Diabetes Mellitus (DM), we have taken in consideration the proper preoperative assessment and optimization of systemic conditions (e.g., controlling blood sugar and blood pressure) are critical to achieving the best outcomes in macular hole surgery. The whole above practices for macular hole intervention surgery, have an important role, for using of tamponade procedure, and changes in Best Corrected Visual Acuity after macular hole surgery, which are analyzed in our study report.
Study objective
The aim of this multi-year study is to evaluate the impact of clinical, systemic and surgical factors on the anatomical and functional outcomes of patients treated for complete macular hole as an achievement in the health level of the patient and compared with studies by contemporary foreign authors.
Specific objectives
a) To determine, whether there is a correlation between the use of tamponade (silicone oil against C3F8 octafluoropropane-a perfluorocarbon gas) and improvement in Visual Acuity (BCVA) after surgery.
b) To analyze the role of demographic (age, gender) and systemic factors like: arterial hypertension, diabetes mellitus, large and depth of full thickness macular hole in functional outcome.
c) To assess, whether the presence of ocular complications such as Retinal Detachment (RRD) affects anatomical and visual outcome.
Time period: The study includes patients treated at the Albanian Eye Center during the period January 2018 - December 2023.
Study type: Retrospective observational study designed as a descriptive and comparative analysis.
Sample size: The study included 26 patients (26 eyes), who fulfill the inclusion criteria and had complete clinical follow-up and regular documentation according the questionnaire rules.
Data on procedures and measurements performed
1) Demographic data: Age, gender, occupation, village/city, etc.
2) Systemic comorbidities: Presence of hypertension, diabetes mellitus, controlling blood sugar and blood pressure.
3) Ocular complications: Presence of retinal detachment or high myopia.
4) Use of intraocular tamponade during surgical intervention: C3F8 (12%) or silicone oil.
5) Functional outcome: Best corrected visual acuity (BCVA) before and after the intervention, measured in decimal units.
6) Anatomic outcome: Effectiveness and documented closure of the macular hole by Optical Coherence Tomography.
Note: Why was used the tamponade with C₃F₈?, because: a] C₃F₈ expands slightly after injection and is long-lasting (can stay in the eye for up to 6–8 weeks); b] It is inert, non-toxic, and clear, making it ideal for internal tamponade, and c] Compared to SF₆ (sulfur hexafluoride), another common gas, C₃F₈ lasts longer, which may be more effective in some cases of large or chronic macular holes.
The collected data were analyzed with SPSS version 21.0 (IBM Corporation), as the appropriate statistical analysis in our study.
- Categorical data were presented as percentages and frequencies.
- The chi-square (χ²) test was used for comparison between groups.
- Spearman's rank correlation coefficient was used to assess the correlation between silicone use and improvement in best-corrected visual acuity. The value of P ≤ 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
A total of 26 patients with Full Thickness Macular Hole (FTMH) were included in the study, with a mean age of 65.7 ± 7.4 years. The prevalence of female gender was 61.5%. Comorbidities included arterial hypertension 69.2% and diabetes mellitus 30.8%. Associated Retinal Detachment (RRD) was present in 76.9% of cases. Intraocular tamponade included C3F8 is about 76.9% and silicone oil is about 23.1%.
In table and graph 1 are shown the patients distribution involved in study report according the age group.
|
Age |
Patients number |
Percentages % |
|
50-59 year |
6 |
23.10% |
|
61-69 year |
12 |
46.20% |
|
70-79 year |
8 |
30.80% |
Table 1: Distribution of patients number involved in study according the age group.
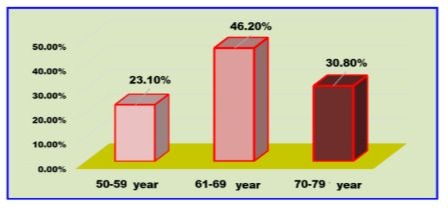
Graph 1: Distribution of patients number involved in study according the age group.
While, the table and graph 2 are shown the patients distribution involved in study report according the gender of the patients.
|
Gender |
Patients number |
Percentages % |
|
Female |
16 |
61.50% |
|
Male |
10 |
38.50% |
Table 2: Distribution of patients number involved in study according their gender.

Graph 2: Distribution of patients number involved in study according their gender.
In the table and graph 3 are shown the patients distribution involved in study report according the full thickness macular holes in the left and right eyes.
|
Eye |
Patients number |
Percentages % |
|
OD |
16 |
61.50% |
|
OS |
10 |
38.50% |
Table 3: Distribution of patients number involved in study according their operated eyes.

Graph 3: Distribution of patients number involved in study according their operated eyes.
Both, table and graph 4 shown the distribution of the patients included in our study according diabetes mellitus (DM) disease.
|
Diabetes Mellitus |
Patients number |
Percentages % |
|
Yes |
8 |
30.8 |
|
No |
18 |
69.2 |
Table 4: Distribution of patients number involved in study according the diabetes mellitus.

Graph 4: Distribution of patients number involved in study according the diabetes mellitus.
The distribution of the patients included in this study report with or without arterial hypertension are shown in tables and graph 5.
|
Arterial Hypertension |
Patients number |
Percentages % |
|
Yes |
18 |
69.20% |
|
No |
8 |
30.80% |
Table 5: Distribution of patients number involved in study according the arterial hypertension.
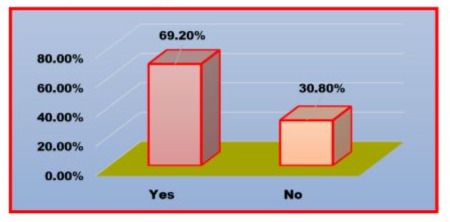
Graph 5: Distribution of patients number involved in study according the arterial hypertension.
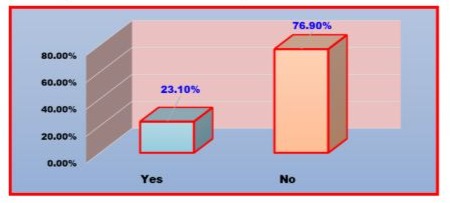
During formulation of the report, we have investigated for the patients included in our study the Retina Detachment (RRD) as well as, which phenomena was showed in table and graph 6.
|
Retinal Detachment |
Patients number |
Percentages % |
|
Yes |
6 |
23.10% |
|
No |
20 |
76.90% |
Table 6: Distribution of patients number involved in study according the retinal detachment.
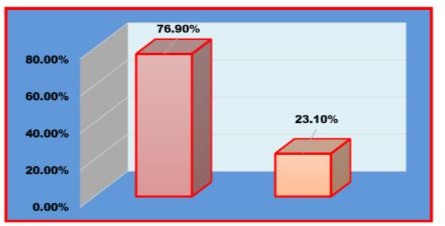
Graph 6: Distribution of patients number involved in study according the retinal detachment.
For patients whom were operated with full thickness macular holes, after their surgery intervention with C₃F₈ gas tamponade, they were usually advised to maintain a face-down position for several days to ensure the bubble presses against the macula effectively. These instructions and recommendations will serve, because the air travel is contraindicated until the gas is fully absorbed, due to the risk of gas expansion with altitude causing increased eye pressure.
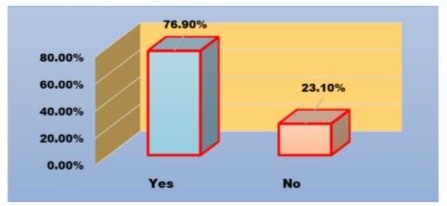
In table and graph 7, and 8, are shown the number of patients, to whom were used the C3F8 gas and silicon oil for tamponade processes during surgery intervention [12,13].
|
Easy Gas |
Patients number |
Percentages % |
|
Yes |
20 |
76.9 |
|
No |
6 |
23.1 |
Table 7: Distribution of patients number involved in study according the gas tamponade.
Graph 7: Distribution of patients number involved in study according the gas tamponade.
|
Silicon Oil |
Patients number |
Percentages % |
|
Yes |
6 |
23.10% |
|
No |
20 |
76.90% |
Table 8: Distribution of patients number involved in study according the use Silicon oil as tamponade.
Graph 8: Distribution of patients involved in study according the use Silicon as tamponade.
Myopia disease at the patient occur when the eye is attempting to focus on an object, but all that visible is a complete non-contrasting material, such as may occur when looking into dense fog. Myopia, or nearsightedness, as well as is a common vision condition where nearby objects appear clear, but distant objects appear blurry. It occurs when the eye is too long or the cornea is too curved, causing light rays to focus in front of the retina instead of directly on it. No image is produced on the retina.
The data-s given in table and graph 9 shown the patients number investigated in study report with myopia disease.
|
Myopia disease |
Patients number |
Percentages % |
|
Yes |
4 |
15.40% |
|
No |
22 |
84.60% |
Table 9: Distribution of patients involved in study according the myopia disease.
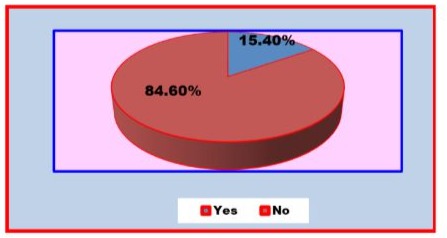
Graph 9: Distribution of patients involved in study according the myopia disease.
Improvement in Visual Acuity (VA)
Visual Acuity refers to the sharpness or clarity of vision, typically measured using a Snellen chart (e.g., the classic "20/20" vision test). The vision phenomena has: a] Normal visual acuity: “20/20” means, the patient can see at 20 feet (@ 610 cm=6,1m.), what a person with normal vision should see at that distance. b] Reduced visual acuity due to myopia: A person with myopia might have 20/100 vision, meaning they need to be at 20 feet to see what someone with normal vision can see from 100 feet (14). After surgery, most patients had improvement in Visual Acuity with varying effects depending on several clinical and anatomical factors.
Postoperative Visual Acuity by age group
The different authors in their studies reported the postoperative Visual Acuity outcome after treatment with Internal Limiting Membrane peeling or inverted Internal Limiting Membrane flap technique [15]. In our study report a weak negative correlation was observed between the age and postoperative Best Corrected Visual Acuity (BCVA), which is (r =-0.14), suggesting that younger patients have a slight tendency to benefit more functionally after the intervention. However, this correlation was not statistically significant, and requires verification in studies with larger samples carried out by other researchers. Table and graph10 shows above mentioned fact.
|
Age groups |
Patients number |
Visual Acuity (Averages) |
Standard deviation (SD) |
Interpretation of fact |
|
50–59 year |
6 |
0.75 |
0.258 |
Great improvement |
|
60–69 year |
12 |
0.525 |
0.27 |
Average improvement |
|
70–79 year |
8 |
0.456 |
0.23 |
Limited improvement |
Table 10: Correlation of age group patients and improvement of BCVA postoperative.
Average of Visual Acuity postoperative is the average vision (in decimal units) that patients in that age group achieved after surgery (for example, patients aged 50–59 had an average of 0.750, which is very good (close to 7.5/10 on Snellen).
Standard Deviation (SD) is a statistical measure that shows how spread out the individual values are around the average values. Small SD=everyone has similar results to the averages; while the Large SD, shown some patients have much better or worse results than the average values.
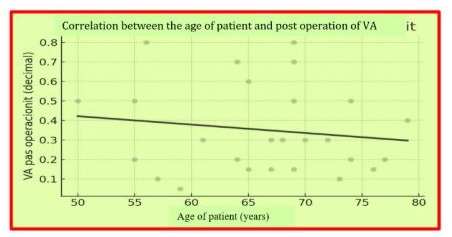
Graph 1: Correlation of age group patients and improvement of BCVA postoperative.
Comparative Analysis of postoperative Visual Acuity using C3F6 gas against Silicone
In our study we have presented the impact of two types of intraocular tamponade carried out by C3F8 and silicone to improve the Visual Acuity (VA) after surgery for macular hole. Spearman’s correlation was used to assess the correlation between the use of each tamponade and postoperative VA, which values shown in table 11 and 12.
|
Tamponade |
ρ (Spearman) |
P-value |
|
C3F |
0.39 |
0.047 |
*Table 11: Correlation between using of C3F6 gas for VA postoperative improvement.
|
Tamponade |
ρ (Spearman) |
P-value |
|
Silicon oil |
-0.42 |
0.033 |
**Table 12: Correlation between using of Silicon for VA postoperative improvement.
*C3F8 Gas correlation coefficient according the (Spearman): V =0.39 and value of P=0.047, and positive and statistically significant correlation between C3F8 use and improvement in postoperative Visual Acuity.
** Silicon correlation coefficient according the (Spearman): V = -0.42 and value of P=0.033 and negative and have not statistically significant correlation between Silicon use and improvement in postoperative Visual Acuity.
Both analyses show that C3F8 is more effective in improving functional Visual Acuity after surgery, while silicone although necessary in specific cases, provides more limited results in terms of visual outcome. The choice of tamponade should be made on a personalized basis, according the complexity of the case and the patient profile. These results highlight the importance of personalized tamponade selection, depending on the patient’s clinical and anatomical profile.
Macular hole length and Visual Acuity after surgery intervention
The aim of this analysis was to assess whether there is a statistically significant association between macular hole length (HEIGHT) and improvement in Visual Acuity (VA) after surgery intervention. Spearman's correlation was used to measure the relationship between these two variables.
|
Parameters |
V (Spearman) |
P-value |
|
HEIGHT versus Visual Acuity after surgery |
-0.06 |
0.838 |
Table 13: Correlation between length of macular hole and Visual Acuity after surgery intervention
The analysis showed a very weak and negative association between macular hole length and improvement in Visual Acuity after surgery intervention. With a correlation coefficient V = -0.06 and value of P = 0.838, the result is not statistically significant. This suggests that in the analyzed sample, macular hole length did not clearly influence functional visual improvement.
Statistical analysis of influencing factors
The impact of DM and HTA in relation to Vision Acuity after surgery intervention was an aim of our study analysis to assess whether there is a correlation between the presence of Diabetes Mellitus (DM) and/or Arterial Hypertension (HTN) in improvement of Visual Acuity (VA) after surgery intervention for macular hole. Spearman's correlation coefficient was used to assess these statistical relationships, and these data are shown in table 14.
|
Factors |
V (Spearman) |
P-value |
Interpretation |
|
Diabeti Mellitus (DM) |
-0.08 |
0.7 |
Weak correlation, non-significant statistically |
|
Hypertension Arterial (HTA) |
0.07 |
0.73 |
Very weak correlation, non-significant statistically |
Table 14: The impact of DM & HTA in relation to VA after surgery intervention.
Analyses carried out for these data did not show any significant impact of diabetes or hypertension on functional improvement in VA after surgery. This suggests that in this sample, these systemic comorbidities were not significant limiting factors in postoperative visual outcome.
While, by the data shown in table 15 and graph 11 are summarized the statistical data carrying out for the evaluation of the correlation between clinical, anatomical and surgical factors for improvement of Visual Acuity after surgery intervention for macular hole. For every by these analysis, the Spearman correlation coefficient and the corresponding P-value are presented to determine statistical significance.
|
Factors |
V (Spearman) |
P-value |
Interpretation |
|
C3F8 |
0.39 |
0.047 |
Positive correlation, significant statistically |
|
Silicon |
-0.42 |
0.033 |
Negative correlation, significant statistically |
|
Age |
- 0.14 |
— |
Weak negative correlation, non-significant statistically |
|
Macular length hole |
-0.06 |
0.838 |
Very weak correlation, non-significant statistically |
|
Macular hole depth |
0.03 |
0.917 |
Very weak correlation, non-significant statistically |
|
Diabeti (DM) |
-0.08 |
0.7 |
Very weak correlation, non-significant statistically |
|
Hypertension (HTA) |
0.07 |
0.73 |
Very weak correlation, non-significant statistically |
Table 15: Summarize of the statistical data performing the evaluation of the correlation between clinical, anatomical and surgical factors for improvement of (VA) after surgery.
The results suggest that the use of C3F8 is the factor most positively associated with functional improvement in Visual Acuity, while silicone oil is negatively associated, probably due to its use in more complex cases. Additionally, to further evaluate the impact of the study types and macular hole size, the anatomical factors such as the length and depth of the macular hole did not show a statistically significant impact in these selected factors [16].
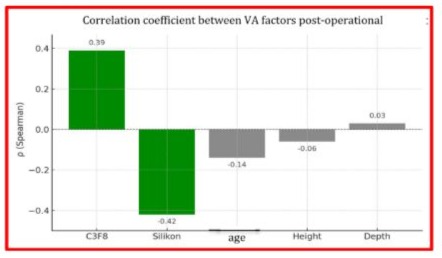
Graph 11: Summarize of the statistical data performing the evaluation of the correlation between clinical, anatomical and surgical factors for improvement of (VA) after surgery
Colors: Green color: Significant or stronger correlation (|P| > 0.3); and Gray color: Weak or non-significant correlation.
The results show that only C3F8 tamponade and silicone have shown a statistically significant correlation with postoperative Visual Acuity improvement. C3F8C is correlated with greater functional improvement, while silicone is more often used in more complex cases, where improvement is more limited. Other clinical and anatomical factors like: age, height, depth, Diabetic Mellitus and Hypertension Arterial have not shown a significant impact in this sample.
A Clinical Study Case Reported
Patient with initials A.V, diagnosed with bilateral Proliferative Diabetic Retinopathy with a history of treatment with intravitreal injections for more than three years, was operated under the local anesthesia (sub-Tenon), in the right eye, because the patient was presented with intravitreal hemorrhage and the full thickness macular hole according the personal data as below:
Preoperative data
- • BCVA OD: 0.05; • BCVA OS: 5/10; • TIOC Ou: 10 mmHg; • Fundus OD: PDR, intravitreal hemorrhage, FTMH; • Fundus OS: PDR with fibrovascular membranes.
Surgical intervention was carried out on 15/11/2024: OD: Phacoemulsification + IOL + PPV (pars plana vitrectomy) + ERM peeling + ILM peeling + Endo laser + fluid-air exchange + C3F8 .
Also, we have investigated the parameters later 6-month follow-up after the surgery intervention and those were: • BCVA OD: 0.2; • BCVA OS: 0.9 (after follow-up with intravitreal injections); • TIOC: 11 mmHg. The patient continues to be followed up for monitoring the postoperative condition and for ongoing treatment of PDR.
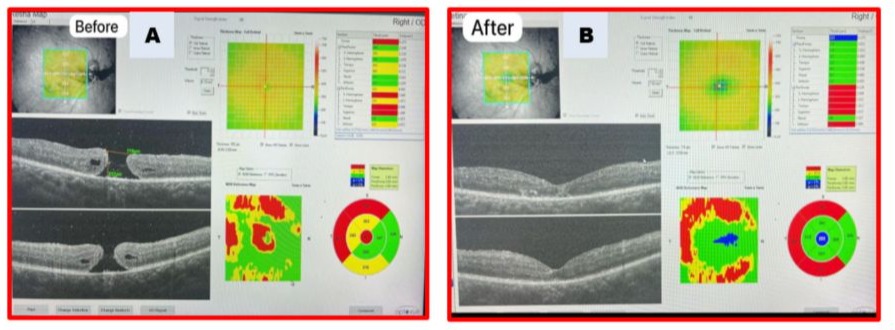
Photo 1 (A): OCT shows a large macular hole and reduced foveal thickness and active PDR associated with hemorrhage, before and after surgical intervention.
Photo 1 (B): OCT post-operative shows an anatomic closure of FTMH, and partial restauration of the foveal profile.
Intraocular tamponade
The gas C3F8 or silicone are injected into the cavity to create pressure on the macula and help close the hole. The shortly protocol is described below for full-thickness macular hole repair with C3F8 gas tamponade involving a vitrectomy procedure, followed by internal limiting membrane peeling [17]. The goal is to release the traction on the retina around the hole and provide a supportive environment for the edges of the hole to close.
1) Pars Plana Vitrectomy small incisions are made in the white part of the eye, and instruments are inserted to remove the vitreous gel, which is the gel-like substance that fills the eye;
2) Internal Limiting Membrane (ILM) peeling a delicate layer of tissue, the ILM is carefully peeled off the surface of the retina around the hole. This helps release any remaining traction on the retinal edges;
3) Fluid-Gas exchange the eye is then filled with a gas bubble, typically C3F8, which provides a tamponade to support the macular hole edges and maintain their position until the hole heals;
4) Postoperative Prone Positioning the patients are instructed to maintain a face-down or prone position for a certain period to help keep the gas bubble against the macular hole and promote its closure;
5) Postoperative Monitoring the patient is monitored for signs of the hole closing or any complications, and further treatment may be necessary if the hole does not close on its own. Regular follow-up appointments are necessary to monitor the patient's progress and address any complications that may arise. C3F8 is a type of fluorinated hydrocarbon gas that provides a long-acting tamponade. Its long-lasting nature means that it doesn't need to be replaced as frequently as other gases, and it offers a larger bubble for a longer period of time, which can be beneficial for maintaining the hole's closure [18,19].
Photo 2: The patient is advised to maintain the face-down position for several days to ensure the success of the tamponade.
Photo 3: The gas C3F8 is injected into the cavity to create pressure on the FTMH and help close
References.
Discussion
The results of this study showed that the use of C3F8 as an intraocular tamponade is statistically significantly associated with improved Vision Acuity after surgery for complete macular hole. In contrast, the use of silicone resulted in a negative correlation, suggesting a more limited functional benefit, especially in more complicated cases.
These findings are consistent with the international literature, where C3F8 has been reported to be more effective in promoting anatomical closure and improving Visual Acuity in patients with full thickness macular hole without severe complications. According to Geiger GL, et al. [20] (Ophthalmology Journal 1994), gas tamponades have more favorable functional outcomes compared to silicone, which is mainly used in cases for clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade etc.
The impact of retinal detachment on Visual Acuity improvement was negative, although not statistically significant. This is consistent with findings in the researcher authors [21], who have suggested in their references that macular involvement in retinal detachment cases may damage photoreceptor cells and negatively affect functional recovery, despite anatomical closure of the hole.
Factors such as age, diabetes, arterial hypertension, hole length and depth did not show a statistically significant association with functional outcome [9,15,22]. However, the lack of impact may be related to the small sample size selected in our study report, and clinical heterogeneity of the cases.
In our study reported were included a limited number of patients and is retrospective in nature. The lack of long-term follow-up and additional functional assessments [23], such as quality of life or visual contrast, constitute important limitations in the overall interpretation of the results.
Recommendations
Prospective studies with larger samples and long-term follow-up are recommended to more accurately assess the effect of prognostic factors on visual improvement after macular hole surgery.
Conclusions
From the analysis of the data of this retrospective study, it resulted that the use of C3F8 gas as intraocular tamponade is statistically significantly associated with a significant improvement in visual acuity after surgery for complete macular hole. This result suggests that the choice of C3F8 may be the optimal strategy in cases without severe complications, while the use of silicone, although technically effective for anatomical purposes, resulted in a more modest visual benefit [24]. This fact should be taken into account during surgical planning, especially in cases where the goal is maximum functional recovery.
The presence of retinal detachment, documented in 6 patients, was associated with a trend towards more limited visual outcomes, although this did not reach statistical significance in this limited sample. Nevertheless, the presence of retinal detachment should be evaluated as a clinically important prognostic factor.
The anatomical dimensions of the hole (length and depth) were not found to be statistically significantly associated with the functional outcome [15,22]. However, their importance cannot be excluded, given the multifactorial complexity of the visual prognosis after the intervention.
The data of this study support the personalized approach to the surgical management of patients with full thickness macular hole, taking into account not only the anatomical dimensions of the lesion, but also the presence of ocular and systemic comorbidities.
It is recommended that the results of this study serve as a basis for further prospective research with a structured design and larger samples [23], with the aim of more in-depth evaluation of the impact of prognostic factors on visual recovery after macular hole surgery.
Institution where the work was done: Referring our study case report, the data collected are reported by research register in “Albanian Center of Eyes”, Tirana, Albania, managed by Associated Prof. Ali Tonuzi.
Auhor Contributions: Conceptualization and methodology: Associated Prof. Ali Tonuzi and Migena Beqiri, Ph.D. Investigation and resources: Secretary of “Albanian Eyes Clinic”, Tirana, Albania. Data curation and writing to the draft of manuscript: Prof. Dr. R. Qafmolla. Writing, review, editing and managing of manuscript Luan Qafmolla. Both authors have read and agreed to the published version of the manuscript.
Plagiarism: The study case report was designed and written by the authors presenting a significant contribution with an effort to ensure that the accuracy of the published parts of the cited literature sources is integrity with the approved norms and rules of the OR&R journal. We declare that for the drafting and revision of the paper, we have strictly respected the rules of acceptance, and in terms of references and citations of the literature used in our scientific research, ethical and academic norms have been taken into account and respected.
Acknowledgement: Both authors of manuscript thank Dr. Luan Qafmolla for obligation and regulation of our manuscript according the guidance of OR & R journal, as well as for contacting with editorial board of this journal. Also, acknowledgements for Prof. Dr. R. Qafmolla and Associated Prof. Ali Tonuzi and his “Albanian Eyes Center” for the contribution in data base and treatment of patients in respective clinics.
Declaration of Figures’ Authenticity: All tables and graphs submitted are created and processing by the authors and well-ordered by Dr. Luan Qafmolla, whom confirm that these data are original with no duplication and have not been previously published in whole or in part in other journals abroad.
Conflicts of Interest: The authors declare that they have no financial or non-financial interests to disclose.
Funding: This research received no external funding
Corresponding person: Dr. Luan Qafmolla, managing of the project for this research article.
References
- Ezra E (2001) “Idiopathic full-thickness macular hole: natural history and pathogenesis”. Br J Ophthalmol 85: 102–108.
- Duker JS, Kaiser PK, et al. (2013) “The International Vitreomacular Traction Study Group classification”. Ophthalmology 120: 2611–2619.
- Kelly NE, Wendel RT (1991) “Vitreous surgery for idiopathic macular holes. Results of a pilot study”. Archives of Ophthalmology Journal 109: 654–659.
- Majumdar S, Tripathy K (2023) “Macular holes in State Pearls; Treasure Island (FL)”: State of Pearls; Publishing: August 25, 2023.
- Mann DF (1996) “Idiopathic macular hole”. Ophthalmology Clinical Journal 5: 95–110.
- Steel DW, Sandinha T, White K (2017) “The macular hole: A review of current management strategies of surgical intervention in eyes” (London. 2017; 31: 492–504.
- Aneesha Kalur, Justin Muste, Rishi P Singh (2022) A Review of Surgical Techniques for the Treatment of Large Idiopathic Macular Holes. Ophthalmic Surg Lasers Imaging Retina 53: 52-61.
- Michalewska Z, Michalewski J, et al. (2010) “Inverted internal limiting membrane flap technique for large macular holes”. Ophthalmology 117: 2018–2025.
- Rezende FA, et al. (2023) “Surgical classification for large macular hole: Based on different surgical techniques results”: The CLOSE Study Group. Internal Journal Retina Vitreous. 9: 1-9.
- Privat E, Gaucher D, et al. (2007) “Residual defect in the foveal photoreceptor layer detected by optical coherence tomography in eyes with spontaneously closed macular holes”. American Journal Ophthalmology 143: 814–819.
- Preti RC, Zacharias LC, Cunha LP, et al. (2020) “Spontaneous macular hole closure after posterior vitreous detachment in an eye with hyperreflective optical coherence tomography stress line”. Am J Ophthalmol Case Rep 20: 95-100
- Alvarez MB, Sabate S, Gomez-Resa M, et al. (2020) “Anatomical and visual outcomes of inverted internal limiting membrane flap technique versus internal limiting membrane peeling in myopic macular hole without retinal detachment”: A preliminary retrospective study. Retina Journal 40: 233–240.
- “Full thickness macular hole: Early intervention is an important factor in visual prognosis”; www.Wikependia.org.; Malaysian Physician Family; 2014 Dec 31.
- F., A, Devis Company; “Taber’s Cyclopedic Medical Dictionary; Illustrated in Full Color”, Edition 18, 1993, pp. 1293; 2091.
- Manasa S, Kakkar P, et al. (2018) “Comparative evaluation of standard ILM peel with inverted ILM flap technique in large macular holes: A prospective, randomized study”. Ophthalmic Surgery Lasers Imaging Retina 49: 236–240.
- Iwasaki M, Kinoshita T, et al. (2019) “Influence of inverted, internal limiting membrane flap technique on the outer retinal layer structures after a large macular hole surgery”. Retina Journal 39: 1470–1477.
- Madreperla SA, Geiger GL, et al. (1994) “Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade. Ophthalmology 101: 682–686
- Ohana E, Blumenkranz M (1998) “Treatment of reopened macular hole after vitrectomy by laser and outpatient fluid gas exchange”. Ophthalmology 105: 1398–1403.
- Jiang J, Chen S, Jia YD, et al. (2021) “Evaluation of macular vessel density changes after vitrectomy with silicone oil tamponade in patients with rhegmatogenous retinal detachment”. Int J Ophthalmol 14: 881–886.
- Madreperla SA, Geiger GL, et al. (1994) “Clinicopathologic correlation of a macular hole treated by cortical vitreous peeling and gas tamponade”. Ophthalmology 101: 682-686.
- Foos RY, Wheeler NC (1982) “Vitreoretinal juncture. Synchesis senilis and posterior vitreous detachment”. 1982; Ophthalmology 89: 1502–1512.
- de NFJ, Preti RC, Monteiro MLR, et al. (2016) Autologous internal limiting membrane fragment transplantation for large, chronic, and refractory macular holes. Ophthalmic Res 2016 55: 45–52.
- Elhusseiny AM, Schwartz SG, et al. (2020) “Long term outcomes after macular hole surgery”. Ophthalmology Retina Journal 369-376.
- Rizzo S, Vento A, Miniaci S (2009) “Heavy silicone oil (Densiron 68) for the treatment of persistent macular holes”; Graefe’s Archives Clinical Experimental Ophthalmology 247: 1471–1476.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.